84 Knee and Lower Leg Injuries
• Knee dislocations are associated with a high risk for neurovascular injury and constitute an orthopedic emergency.
• A grossly unstable knee should be assumed to have been dislocated.
• Patients with fractures or dislocations of the knee and lower extremity and neurovascular compromise should undergo emergency reduction or realignment before any radiographic evaluation.
• Patients discharged home in knee immobilizers with stable injuries should be instructed to remove the device several times a day and perform range-of-motion and quadriceps-strengthening exercises.
• The cast or splint should be removed from any patient with increasing pain after a lower leg fracture to allow careful assessment of neurovascular status and evaluation of the lower leg compartments.
Pathophysiology
Knee
Anatomy
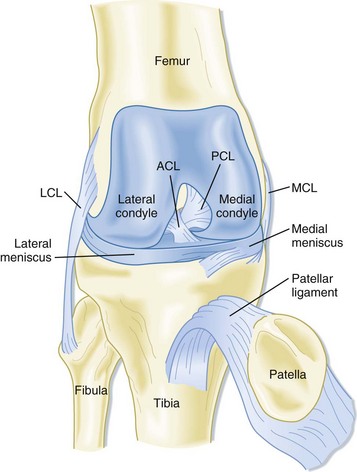
Knee stability is provided solely by ligaments and tendons in and around the joint (Fig. 84.1). The knee joint is encapsulated by fibrous connective tissue lined by a synovial membrane. The knee capsule is continuous with the suprapatellar bursa, which expands when a joint effusion is present.
Evaluation
Key aspects of evaluation of knee are listed in Box 84.1. In general, evaluation of knee complaints should also include an examination of the hip and back to prevent overlooking a source of pain referred to the lower extremity.
Box 84.1 Evaluation of the Knee
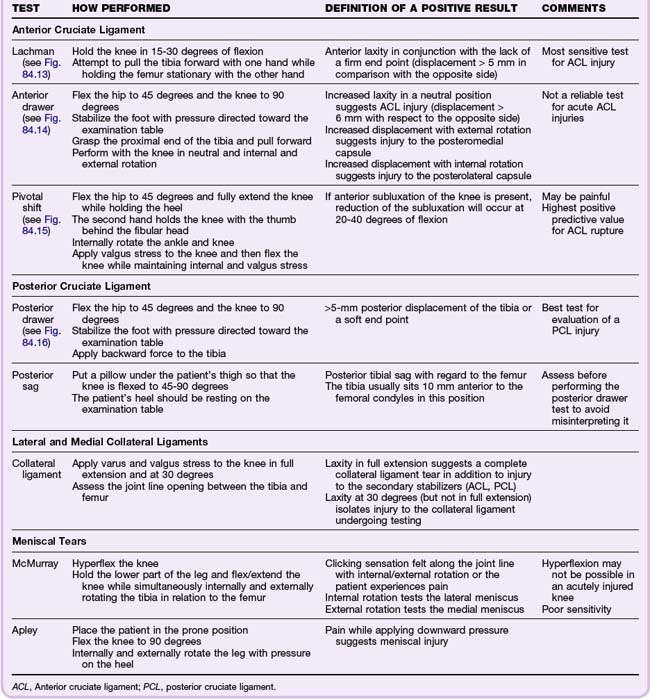
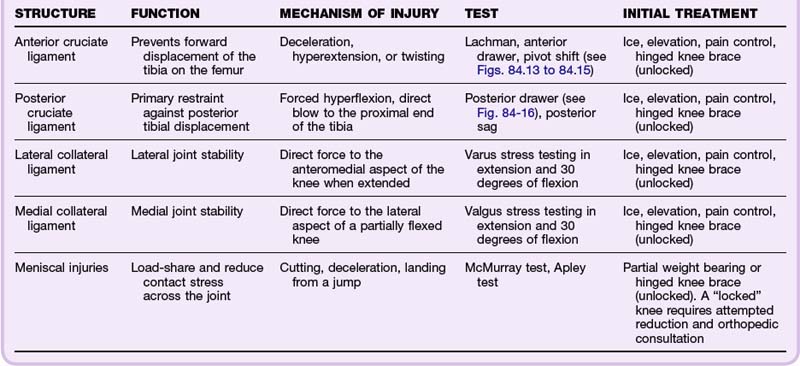
During evaluation, the point of maximal tenderness should be assessed last. Specific tests for evaluating ligamentous and meniscal injuries are detailed in Table 84.1. Comparison with the uninjured or normal knee is helpful, especially for assessment of ligamentous laxity.
Diagnostic Testing
Because acute injuries to the knee commonly involve soft tissue, plain radiographic examination is not always indicated. The Ottawa Knee Rules1 (Box 84.2) and the Pittsburgh Knee Rules2 (Box 84.3) are useful guides to aid in the decision of whether to order plain radiographs. Both criteria are sensitive for fractures, but the Pittsburgh criteria are more specific and can be applied to both children and adults.
Box 84.2 Ottawa Knee Rules
Radiographs indicated if any one of the following is present:
Box 84.3
Pittsburgh Knee Rules
• The patient is younger than 12 or older than 50 years.
• The patient is unable to walk four weight-bearing steps in the emergency department.
Data from Seaberg DC, Yealy DM, Lukens T, et al. Multicenter comparison of two clinical decision rules for the use of radiography in acute, high-risk knee injuries. Ann Emerg Med 1998;32:8–13.
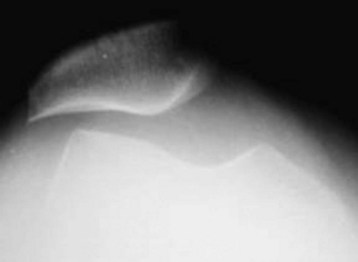
If plain radiographs are indicated, a minimum of an anteroposterior (AP) and a lateral view should be obtained. Oblique radiographs are helpful for detecting subtle tibial plateau fractures. The intercondylar or tunnel view is helpful in evaluating for tibial spine fractures and osteochondral defects (Fig. 84.2). Assessment of the patellofemoral joint and evaluation for the presence of patellar tilt (increased propensity for patellar subluxation or dislocation) can be done with the Merchant or sunrise view (Fig. 84.3). Comparison radiographs of the unaffected extremity are helpful in discerning problems in skeletally immature patients.

Fig. 84.2 Knee radiograph, tunnel or intercondylar view, showing an osteochondritis dissecans lesion (arrows).
When describing the knee radiograph, the examiner should note the alignment and joint spacing of the femoral condyles in relation to the tibial plateau. Narrowing of the joint space (particularly in weight-bearing views) indicates articular cartilaginous and meniscal degeneration. The patella should be examined for possible fractures (in the event of a direct blow to the anterior aspect of the knee) and the presence of a bipartite or tripartite patella. Significant joint effusions are evident as a water-density radiolucency on the lateral view, anterior to the distal end of the femur.3 Effusions seen shortly after injury are suggestive of anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL) tears, tibial plateau fractures, femoral condyle fractures, or patellar fractures.4
In the setting of acute injuries, radiographs should be examined for the presence of fractures involving the tibial plateau (depression fracture) or tibial spine (suggesting rupture of the ACL). Segond fractures are avulsion fractures of the lateral tibial plateau at the site of attachment of the lateral capsular ligament. These fractures are associated with ACL and meniscal injuries. The presence of posterior opaque bodies should also be noted. These may be fabellae (congenital sesamoid) or loose bodies. More than 75% of loose bodies originate from osteochondral lesions.3 Occult fractures that are commonly missed on plain radiographs include patellar, tibial plateau, fibular head, and Segond fractures.5
Musculoskeletal ultrasound techniques can be used to diagnose ACL and PCL tears and may be helpful in the diagnosis of meniscal injuries.4 Magnetic resonance imaging (MRI) can be used to confirm suspected meniscal injuries, ligamentous disruptions, osteochondral lesions, and occult fractures; however, it is rarely indicated in the acute setting. Computed tomography (CT) is helpful for establishing the extent of certain fractures (e.g., tibial plateau fractures) and is often more readily available than MRI.
Lower Leg
Anatomy
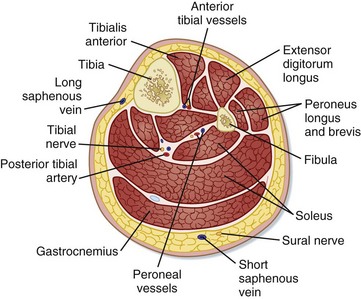
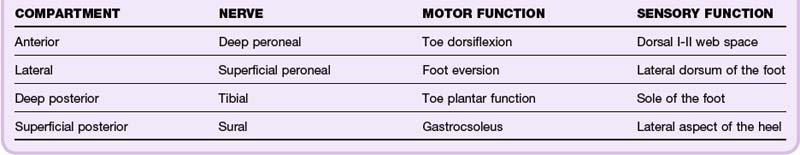
The thigh muscles attach to the upper part of the tibia and lend stability to the knee joint. The muscles of the lower part of the leg, which are enclosed by fascia, can be divided into four compartments: anterior, posterior, deep posterior, and lateral (Fig. 84.4). Specific motor and sensory nerve distributions are listed by compartment in Table 84.2.
Dislocations and Fractures
Dislocations
Knee Dislocations
Knee dislocations are relatively uncommon and represent, at most, 0.2% of all orthopedic injuries. They require disruption of at least three of the four major ligaments of the knee. Common mechanisms include traffic accidents, sporting injuries, or simple mechanical falls. Dislocations are classified on the basis of the direction of tibial movement in relation to the femur. Anterior and posterior dislocations account for approximately 70% of all knee dislocations. Knee dislocations may also have associated intraarticular fractures involving the tibial plateau or femoral condyles.6
Knee dislocations are associated with a high risk for neurovascular injury and should be considered an orthopedic emergency. The neurovascular bundle runs posterior to the bony and ligamentous structures in the popliteal fossa. The popliteal artery and nerve are fixed in the fibrous tunnel of the adductor magnus muscle proximally and traverse the fibrous arch of the soleus muscle and interosseous membrane distally. The relative immobility of the neurovascular bundle makes it susceptible to injury. The popliteal artery may be injured in up to 14% of all knee dislocations (Fig. 84.5). Traction injuries to the common peroneal and, less commonly, to the tibial nerve may also be present.6
Neurovascular status should be documented before and after reduction. All patients with a suspected or confirmed knee dislocation should have the ankle-brachial index (ABI) calculated. An ABI of less than 0.9 has high predictive value for a vascular injury, and such patients should undergo either CT or traditional angiography. Patients with normal findings on vascular examination and an ABI lower than 0.9 should be observed for at least 24 hours with neurovascular checks every 2 to 3 hours.4 Prompt diagnosis of vascular injury is essential given the chance of development of progressive distal ischemia. When injury to the popliteal artery has occurred, patient outcome is directly related to the duration of ischemia.
Standard AP and lateral radiographs are adequate for initial evaluation of knee dislocations. After appropriate analgesia and sedation, emergency reduction of the dislocated knee should be attempted. Longitudinal traction on the tibia (to free it from the femur) should be followed with a force in the opposite direction of the dislocation. The rotary components should also be corrected to restore normal leg alignment. After reduction, the knee should be immobilized in 15 to 20 degrees of flexion.4 Orthopedic consultation in the ED is mandatory for all suspected and confirmed knee dislocations.
Patellar Dislocation
The patella normally articulates in the groove between the femoral condyles. The vastus medialis, medial and lateral patellofemoral, and patellotibial ligaments and the medial retinaculum all stabilize the patella (Fig. 84.6).

Fig. 84.6 Patellofemoral and patellotibial ligaments.
These structures act as static stabilizers of the patella.
(From DeLee JC, Drez Jr D, Miller MD. DeLee & Drez’s orthopaedic sports medicine: principles and practice. 2nd ed. Philadelphia: Saunders; 2003.)
The overall incidence of patellar dislocations is estimated to be 7 per 100,000 per year and as high as 31 per 100,000 per year in patients between the age of 10 and 19 years.7 Patellar dislocations most commonly occur when a varus force is applied to a flexed knee or after forced contraction of a flexed quadriceps. Dislocations may be associated with meniscal tears, disruption of the medial collateral ligament, and osteochondral fractures.4
The patient may report that the knee “gave out,” followed by pain and swelling. Patients may not be able to bear weight on or flex the knee. An acute hemarthrosis is most commonly seen if an associated osteochondral fracture is present. A patellar apprehension test may be useful in a patient who reports a dislocation that resolved spontaneously. This test is performed by moving a nondisplaced patella laterally. The result is positive if the patient shows apprehension, senses pain, or feels a sensation of impending dislocation when the patella is moved laterally (Fig. 84.7). AP, lateral, and sunrise radiographs are adequate to evaluate for acute dislocations and associated fractures.

Fig. 84.7 Positive apprehension test.
(From DeLee JC, Drez Jr D, Miller MD. DeLee & Drez’s orthopaedic sports medicine: principles and practice. 2nd ed. Philadelphia: Saunders; 2003.)
After reduction, the patient should be told to use conservative therapeutic measures, such as ice, elevation, and pain control. The knee should be placed in a straight leg immobilizer, and the patient can start progressive weight bearing when comfortable. Follow-up should be arranged within 1 to 2 weeks. Complications include persistent instability, subluxation, repeated dislocation, and osteoarthritis.4
Proximal Tibiofibular Joint Dislocations
Tibiofibular dislocations are reduced by flexing the knee to 90 degrees and everting and dorsiflexing the ankle while applying direct pressure to the head of the fibula. General anesthesia may be necessary. After reduction, the knee should be immobilized in extension or partial flexion. Posterior dislocations may be unstable, and recurrent subluxation may be seen. Degenerative joint disease and arthritis can develop after injury to this joint.8
Fractures
Patellar Fracture
The patient usually has a swollen, painful knee. Patellar evaluation includes palpation for pain and bony disruption and assessment for extensor weakness. AP, lateral, and sunrise views of the knee should be obtained. A bipartite patella may be difficult to distinguish from a patellar fracture and is most often seen in the superolateral part of the patella. A high-riding patella, or a patella alta position, may signify disruption of the distal extensor mechanism; this is best visualized on AP and lateral views.8
Acute treatment of patellar fractures consists of ice, elevation, pain control, and a straight leg knee immobilizer. Nonoperative intervention is considered for nondisplaced fractures (<3 to 4 mm) when the extensor mechanism is intact. Patients with a disrupted extensor mechanism should have immediate orthopedic consultation because these injuries are often repaired within 24 hours.4
Proximal Tibial Fractures
Proximal tibial fractures include fractures above the tibial tuberosity.
Tibial Plateau Fractures
The proximal end of the tibia comprises the medial and lateral condyles, which make up approximately three fourths of the proximal tibial surface. The condyles ensure appropriate knee alignment, stability, and motion. Tibial plateau fractures account for about 1% of all proximal tibial fractures.9
Tibial plateau fractures are caused by side loading secondary to either a varus or a valgus force combined with axial compression, which results in the femoral condyle impacting on the tibia. Common mechanisms are motor vehicle crashes, falls, and athletic activities such as skiing (Fig. 84.8). A Segond fracture is bony avulsion of the lateral tibial plateau at the site of attachment of the lateral capsular ligament. This fracture is an important marker for ACL disruption and anterolateral rotary instability. Associated soft tissue injuries to the collateral ligaments, menisci, and neurovascular structures are common, although low-energy injuries (from athletic activities) usually result in less soft tissue damage.9

Fig. 84.8 Lateral tibial plateau fracture.
(From Browner BD, Jupiter JB, Levine AM, et al. Skeletal trauma: basic science, management, and reconstruction. 3rd ed. Philadelphia: Saunders; 2003.)
Patients with tibial plateau fractures exhibit pain and swelling of the knee and hold their knee in a slightly flexed position. A valgus or varus deformity of the knee generally indicates a depressed fracture. Careful assessment of associated ipsilateral bony, soft tissue, and neurovascular status is essential given the high rate of association of such injuries with tibial plateau fractures.9
AP, lateral, and oblique radiographs are necessary to evaluate tibial plateau fractures. In addition, a tibial plateau view is helpful in assessing the amount of depression present. CT with 2-mm cuts and three-dimensional reconstruction is useful to further investigate indeterminate plain films, evaluate fracture patterns, show the precise extent of articular depression, and assist in planning for optimal operative treatment.4
Absolute indications for surgery are open fractures, arterial injuries, and compartment syndrome. Relative indications for surgery are displaced fractures leading to joint instability and depression of the plateau. The amount of depression that requires operative intervention is controversial and ranges from 3 to 10 mm; however, 3 mm is the usual cutoff in athletic patients.9
Tibial Spine Fractures
The intercondylar eminence, or tibial spine, is the central portion of the proximal tibial surface. Tibial spine injuries usually result from a hyperextension force with or without a valgus or rotational moment about the knee. The fracture may also occur after a direct blow to the distal end of the femur while the knee is flexed (Fig. 84.9).
Fractures with little or no displacement should be immobilized in a long leg splint with the knee flexed at approximately 10 to 20 degrees. Displaced fractures necessitate orthopedic consultation because they may require closed reduction (if no ligamentous damage is present) or open or arthroscopic reduction with fixation of the fragments.10
Subcondylar Fractures
Routine AP and lateral radiographs are adequate for evaluation of subcondylar fractures. Acute management of these injuries involves ice, elevation, and immobilization in a long leg splint. Stable extraarticular nondisplaced transverse fractures are treated with a long leg cast for 8 weeks. Fractures that are comminuted or associated with a condylar component require open reduction and internal fixation.8
Tibial Shaft Fractures
Tibial shaft fractures result from either direct (motor vehicle accidents) or indirect (rotary or compressive forces) trauma. High-energy direct injuries usually cause transverse or comminuted fractures (most common). Indirect trauma commonly results in spiral or oblique fractures (Fig. 84.10).
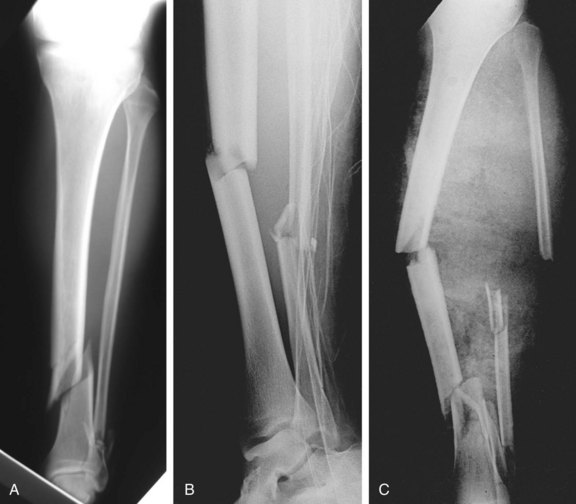
Fig. 84.10 Radiographic examples of the three grades of severity of tibial fractures.
(From Browner BD, Jupiter JB, Levine AM, et al. Skeletal trauma: basic science, management, and reconstruction. 3rd ed. Philadelphia: Saunders; 2003.)
Open fractures should be gently cleaned, dressed with sterile dressings, and placed in a splint while awaiting orthopedic consultation. Patients should receive prophylactic antibiotics and tetanus prophylaxis. Emergency reduction is necessary for injuries accompanied by neurovascular compromise. Nonunion or delayed union is more likely with fractures that are open, severely displaced, or comminuted or with fractures associated with severe soft tissue injuries or infections.11
Proximal Fibular Fractures
Isolated proximal fibular fractures are treated with protected weight bearing. The EP must rule out other associated injuries, such as lateral collateral ligament injury, common peroneal nerve injury, arterial injuries, and Maisonneuve fractures.11
Tibial Tuberosity Fractures
Tibial tubercle avulsion fractures are rare injuries. Although they can occur in adults, these fractures are more commonly seen in adolescents undergoing a growth spurt. Most fractures are the result of an indirect force delivered by an eccentric load.12 A sudden flexion force is applied while the knee is in flexion and the quadriceps is tightly contracted. The quadriceps resists the force, which causes avulsion of the tibial tubercle.
The physical findings depend on the extent of the injury. Swelling and tenderness are present over the anterior aspect of the tibia. A joint effusion may result from associated intraarticular injuries. The injured knee is usually held in 20 to 40 degrees of flexion secondary to hamstring spasm. In addition, the patient may not be able to extend the knee because of either pain or loss of the extensor mechanism.13
Routine AP and lateral radiographs are useful for ruling out associated fractures (Fig. 84.11). Initial treatment is similar to that for both quadriceps and patellar tendon injuries. Minimally displaced fractures are treated conservatively. Displaced fractures frequently require open reduction and internal fixation.12
Soft Tissue and Cartilaginous Injuries
Extensor Mechanism Injuries
The extensor mechanism of the knee is composed of the quadriceps muscles and tendon, the patella, the patellar tendon, and the tibial tubercle. Injuries can result from direct trauma (direct blow or laceration) or an indirect force (forced flexion of the knee). Rupture of the extensor mechanism is relatively uncommon in comparison with other injuries involving the knee joint.12
Quadriceps and Patellar Tendon Injuries
Quadriceps ruptures typically occur in patients older than 40 years. Rupture is usually the result of forced quadriceps contraction with a flexed knee, which loads the tendon. Direct blows and lacerations can also cause disruption of the tendon. The most common site of rupture is at or near its insertion on the patella. Predisposing factors are listed in Box 84.4.
Ligamentous and Meniscal Injuries
Knee stability depends on the static stability of the ligaments and the dynamic stability of the muscles. Injuries to the knee involve the following six common mechanisms: (1) valgus stress (laterally directed), (2) varus stress (medially directed), (3) hyperextension, (4) rotational stress, (5) direct anterior stress, and (6) direct posterior stress. These stressors, working in isolation or combination, may result in myriad of ligamentous, meniscal, or chondral injuries.12
Common mechanisms of ligamentous knee injuries are shown in Figure 84.12. Diagnosis is based on clinical examination; plain radiographs are indicated if a fracture is suspected. MRI offers a direct, noninvasive view of the knee ligaments, menisci, and other soft tissue structures; however, it is rarely indicated in the ED setting.
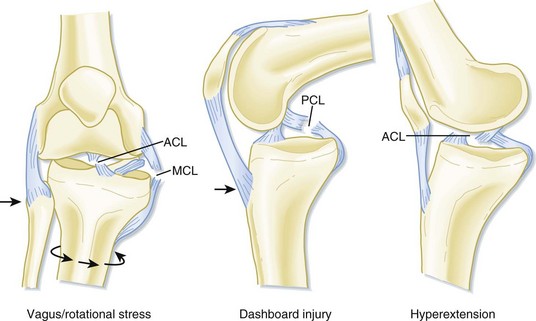
Fig. 84.12 Common mechanisms of knee injuries.
(From Browner BD, Jupiter JB, Levine AM, et al. Skeletal trauma: basic science, management, and reconstruction. 3rd ed. Philadelphia: Saunders; 2003.)
Stability testing for ligamentous and meniscal injuries is outlined in Table 84.1 and Figures 84.13 to 84.16. Ligament function, mechanism of injury, diagnosis, and treatment are outlined in Table 84.3. Most ligamentous and meniscal injuries should be reevaluated by an orthopedist in 3 to 5 days.4
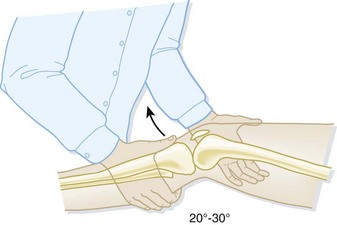
Fig. 84.13 Lachman test for anterior drawer instability.
(From Browner BD, Jupiter JB, Levine AM, et al. Skeletal trauma: basic science, management, and reconstruction. 3rd ed. Philadelphia: Saunders; 2003.)

Fig. 84.14 Anterior drawer test.
(From Brown JR, Trojian TH. Anterior and posterior cruciate ligament injuries. Prim Care 2004;31:925–56.)
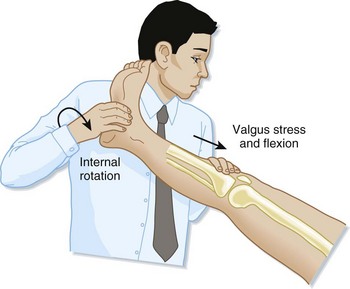
Fig. 84.15 Pivot shift test.
(From Brown JR, Trojian TH. Anterior and posterior cruciate ligament injuries. Prim Care 2004;31:925–56.)
Muscle Strains
Gastrocnemius Muscle Strain
Patients may describe sudden calf pain while running or making a sudden stop or cut. Pain and swelling of the calf develop over the next day, and tenderness is typically found at the musculotendinous junction of the medial (more common) or lateral head of the gastrocnemius muscle. Complete rupture of the head of the gastrocnemius muscle is associated with retraction of the muscle belly. Acute posterior compartment syndrome has been associated with rupture of the medial head of the gastrocnemius muscle.14
Overuse Injuries
Common tendinopathies and bursitis of the knee are described in Chapter 86.
Osgood-Schlatter Disease
Osgood-Schlatter disease is generally a self-limited condition. In most cases, treatment is nonoperative and consists of modification of activity, nonsteroidal antiinflammatory drugs (NSAIDs), and physical therapy. The family of an adolescent with this disorder should be counseled that the symptoms may take up to 12 to 18 months to resolve.13
Stress Fractures
Evidence of a stress fracture may not appear on plain radiographs for up to 2 to 10 weeks after the onset of symptoms. The presence of a transverse fracture line across the entire anterior shaft of the tibia on a plain radiograph is considered a poor prognostic sign and is associated with a greater likelihood of nonunion.8 Radionuclide scintigraphy can confirm the diagnosis as early as 2 to 8 days after the onset of symptoms.
Initial treatment consists of conservative therapy: ice, antiinflammatory pain medication, and rest for several weeks or until the extremity is free of pain. Tibial fractures that do not improve with conservative management may require splinting in a walking boot or air splint. A midshaft tibial fracture is splinted until the extremity is pain free with radiographic evidence of healing.15
Other Disorders
Osteochondritis Dissecans
Osteochondritis dissecans is a potentially reversible idiopathic lesion of subchondral bone. It is seen more often in children and adolescents. Osteochondritis dissecans of the knee occurs most commonly on the posterolateral aspect of the medial femoral condyle (70% to 80%) (Fig. 84.17). Inflammation, genetics, ischemia, ossification, and repetitive trauma have all been hypothesized as possible causes.
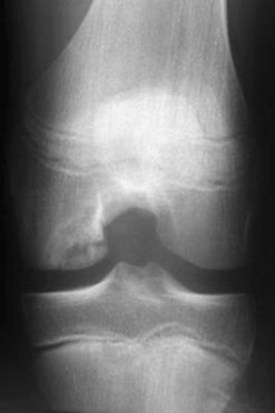
Fig. 84.17 Tunnel radiograph of a juvenile osteochondritis dissecans lesion of the medial femoral condyle.
Stable osteochondritis dissecans lesions have a favorable healing rate with conservative management alone (modified activity, NSAIDs, rehabilitative exercises). Patients and their parents should be instructed that it takes up to 12 to 18 months for healing to be complete.16
Osteonecrosis
Patients with early stages of osteonecrosis are treated conservatively with partial weight bearing and antiinflammatory medications. Patients with advanced disease may require surgery to restore the articular surface. Total knee arthroplasty is reserved for disease that has expanded to the lateral compartment.17
Patellofemoral Pain Syndrome
Patellofemoral pain syndrome refers to the clinical manifestation of anterior knee pain related to changes in the patellofemoral articulation. Patients are generally between the ages of 10 and 20 years and usually have complaints of nonspecific anterior knee pain that is not related to trauma. Athletes may experience symptoms after periods of overactivity. Elderly patients may exhibit symptoms if they have arthritis that affects the patellofemoral joint. The most important risk factors are overuse, quadriceps weakness, and soft tissue tightness. In most cases the etiology is multifactorial.18
The patient has a history of mild to moderate anterior knee pain. The knee may be more painful with prolonged flexion, stair climbing, or kneeling. Physical examination may show a slight effusion, along with patellar crepitus on range of motion. Applying direct pressure to the anterior aspect of the patella may reproduce the patient’s pain.5
Plain radiographs are not indicated. CT or MRI can detect abnormalities in the articular surface of the patella. In most cases, a physical therapy program that strengthens the quadriceps muscle can successfully reduce the symptoms. Surgery may be required for the minority of patients who do not respond to conservative management.18
Popliteal Cyst
Ultrasonography is helpful to distinguish Baker cysts from other disorders, such as popliteal artery aneurysms, neoplasms, and thrombophlebitis. Treatment is based on the underlying cause. Asymptomatic cysts found incidentally need no further treatment.19
![]() Documentation
Documentation
The following issues should be clearly documented in a patient with knee or lower leg injury:
• History: Mechanism of injury; duration and location of symptoms; associated symptoms; exacerbating or alleviating factors; complaints of weakness, numbness, or instability; complicating medical factors; and previous interventions, imaging, or evaluations
• Physical examination: Neurovascular status (before and after splint placement or reduction), compartment assessment, skin integrity, stability assessment, and associated injuries
• Radiography: Anteroposterior or lateral films of the joint above and below the injury; prereduction and postreduction films indicated for most reductions
• Medical decision making: Any emergency reduction secondary to neurovascular compromise and reasons for emergency or nonemergency consultation or follow-up
• Procedures: Neurovascular status both before and after reduction or splint placement, skin integrity, and postreduction fracture alignment
• Patient instructions: Discussion with the patient regarding splint care, appropriate crutch use, importance of range-of-motion exercises, weight-bearing status, warning signs for neurovascular impairment and compartment syndromes, and arrangements for follow-up or return to the emergency department
![]() Patient Teaching Tips
Patient Teaching Tips
A patient in whom a strain, sprain or stable injury of the knee is diagnosed should be discharged home in a hinged brace (fully unlocked). If discharged in a knee immobilizer, the patient should be instructed to perform gentle range-of-motion exercises multiple times per day to prevent joint stiffness.
A patient with a tibia fracture who is sent home should be educated about compartment syndrome and told to return to the emergency department if either severe pain or numbness in the foot or leg develops within the first 48 hours.
A patient with an acute injury should be instructed to:
In a patient discharged from the emergency department on crutches:
Davenport M. Knee and leg injuries. Emerg Med Clin North Am. 2010;28:861–884.
Howells NR, Brunton LR, Robinson J, et al. Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury. 2010. Available at http://www.ncbi.nlm.nih.gov/pubmed/21156317
Seaberg DC, Yealy DM, Lukens T, et al. Multicenter comparison of two clinical decision rules for the use of radiography in acute, high-risk knee injuries. Ann Emerg Med. 1998;32:8–13.
Stiell IG, Wells GA, McDowell I, et al. Use of radiography in acute knee injuries: need for clinical decision rules. Acad Emerg Med. 1995;2:966–973.
1 Stiell IG, Wells GA, McDowell I, et al. Use of radiography in acute knee injuries: need for clinical decision rules. Acad Emerg Med. 1995;2:966–973.
2 Seaberg DC, Yealy DM, Lukens T, et al. Multicenter comparison of two clinical decision rules for the use of radiography in acute, high-risk knee injuries. Ann Emerg Med. 1998;32:8–13.
3 Allen JE, Taylor KS. Physical examination of the knee. Prim Care. 2004;31:887–907.
4 Davenport M. Knee and leg injuries. Emerg Med Clin North Am. 2010;28:861–884.
5 Calmbach WL, Hutchens M. Evaluation of patients presenting with knee pain. Part II: differential diagnosis. Am Fam Physician. 2003;68:917–922.
6 Howells NR, Brunton LR, Robinson J, et al. Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury. 2010. Available at http://www.ncbi.nlm.nih.gov/pubmed/21156317
7 Andrish J. The management of recurrent patellar dislocation. Orthop Clin North Am. 2008;39:313–327.
8 Simon RR, Koenigsknecht SJ. Emergency orthopedics: the extremities, 4th ed. New York: McGraw-Hill; 2001.
9 Bharam S, Vrahas MS, Fu FH. Knee fractures in the athlete. Orthop Clin North Am. 2002;33:565–574.
10 Accousti WK, Willis RB. Tibial eminence fractures. Orthop Clin North Am. 2003;34:365–375.
11 Hanlon DP. Leg, ankle, and foot injuries. Emerg Med Clin North Am. 2010;28:885–905.
12 Perryman JR, Hershman EB. The acute management of soft tissue injuries of the knee. Orthop Clin North Am. 2002;33:575–585.
13 Duri ZA, Patel DV, Aichroth PM. The immature athlete. Clin Sports Med. 2002;21:461–482.
14 El-Dieb A, Yu JS, Huang GS, et al. Pathologic conditions of the ligaments and tendons of the knee. Radiol Clin North Am. 2002;40:1061–1079.
15 Wilder RP, Sethi S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81.
16 Kocher MS, Tucker R, Ganley TJ, et al. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34:1181–1191.
17 Soucacos PN, Johnson EO, Soultanis K, et al. Diagnosis and management of the osteonecrotic triad of the knee. Orthop Clin North Am. 2004;35:371–381.
18 LaBella C. Patellofemoral pain syndrome: evaluation and treatment. Prim Care. 2004;31:977–1003.
19 Handy JR. Popliteal cysts in adults: a review. Semin Arthritis Rheum. 2001;31:108–118.