Emboli to SMA from cardiac sources most commonly
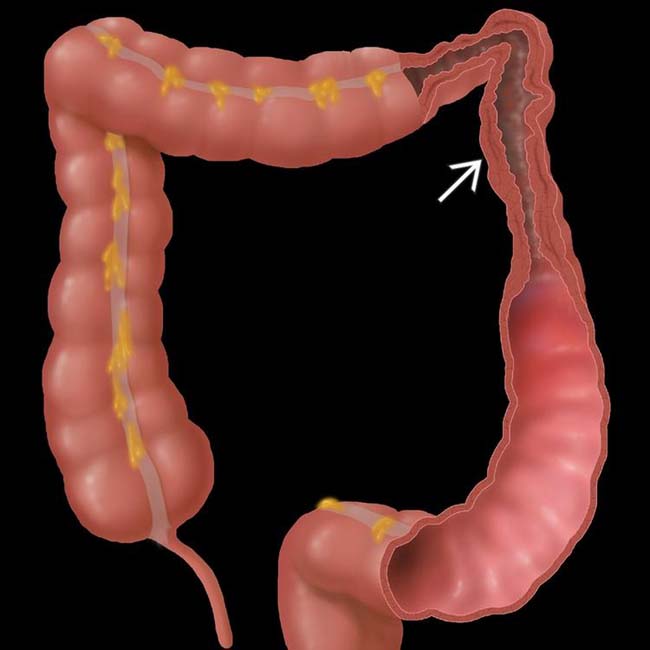
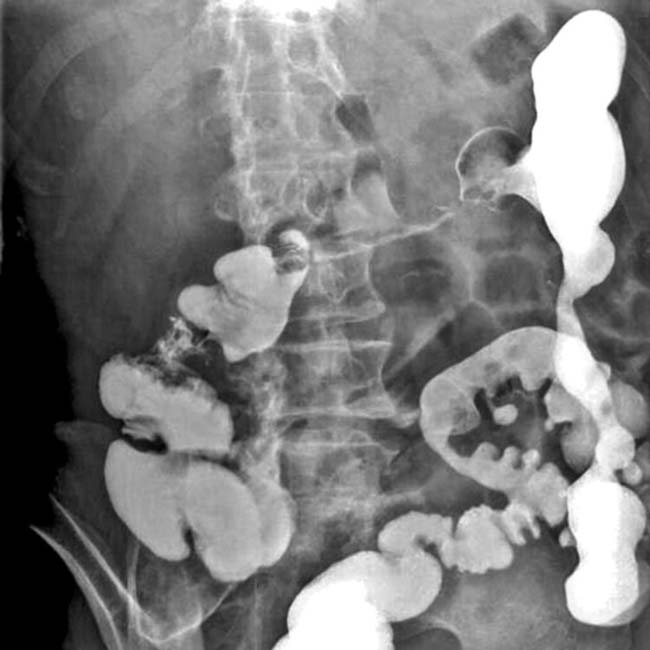
 near the splenic flexure, a “watershed” area between the vascular distribution of the SMA and IMA.
near the splenic flexure, a “watershed” area between the vascular distribution of the SMA and IMA.
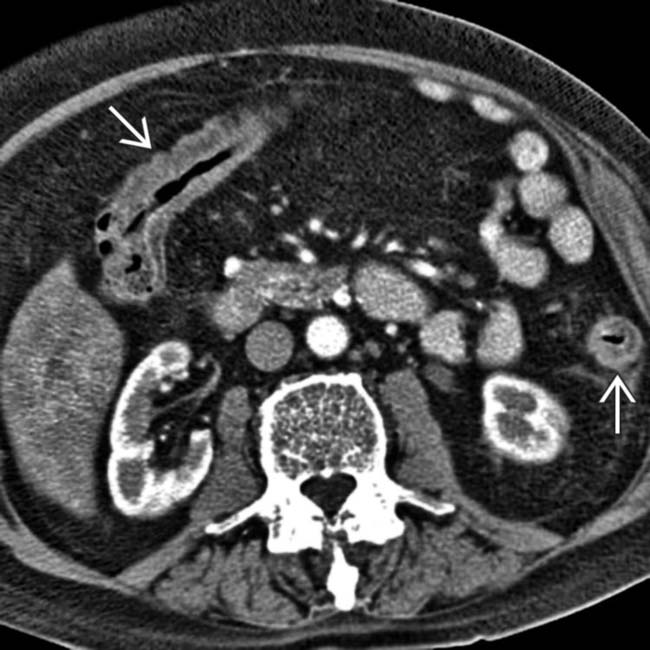
 . Incidental renal allograft noted
. Incidental renal allograft noted  .
.
 . The SMA and SMV are patent.
. The SMA and SMV are patent.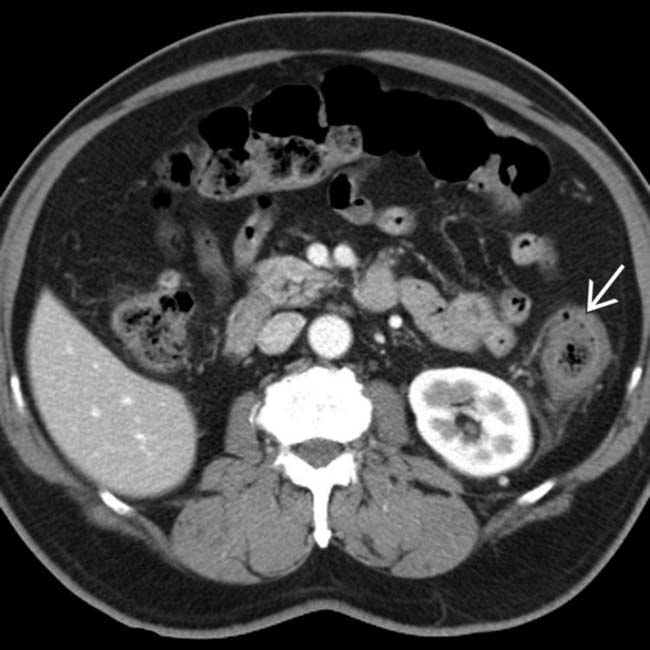
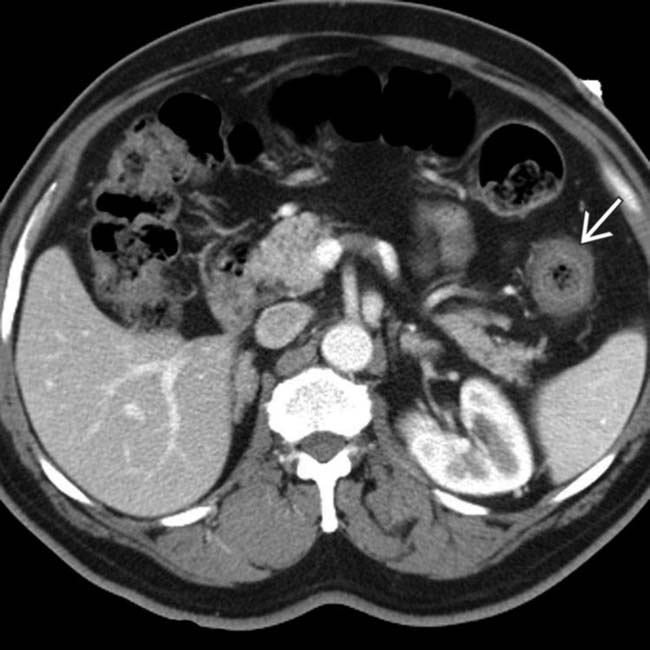
 , whereas the remaining colon is normal. The rectum (not shown) was normal. These are classic clinical and CT features of ischemic colitis due to a hypotensive episode in an elderly patient.
, whereas the remaining colon is normal. The rectum (not shown) was normal. These are classic clinical and CT features of ischemic colitis due to a hypotensive episode in an elderly patient.IMAGING
General Features
 , whereas the more proximal colon is gas-distended with a normal wall.
, whereas the more proximal colon is gas-distended with a normal wall.
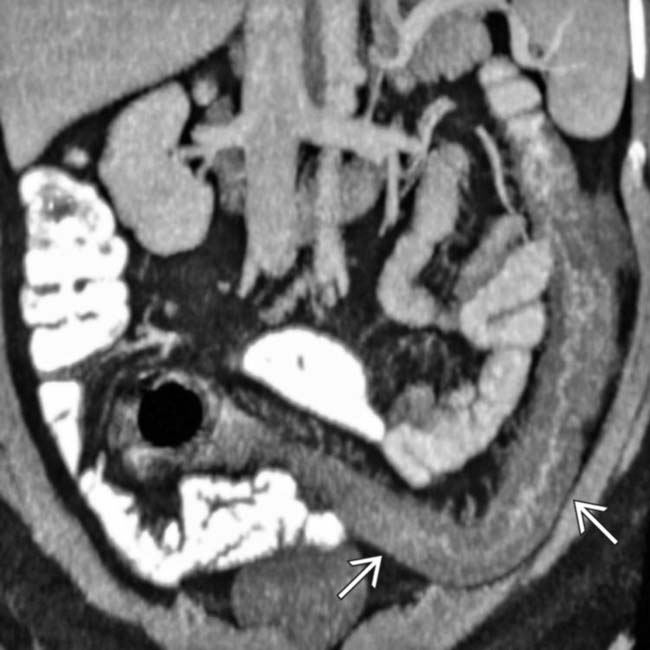
 . The rectum
. The rectum  is spared. Ascites
is spared. Ascites  is noted. These are classic clinical and CT features of ischemic colitis.
is noted. These are classic clinical and CT features of ischemic colitis.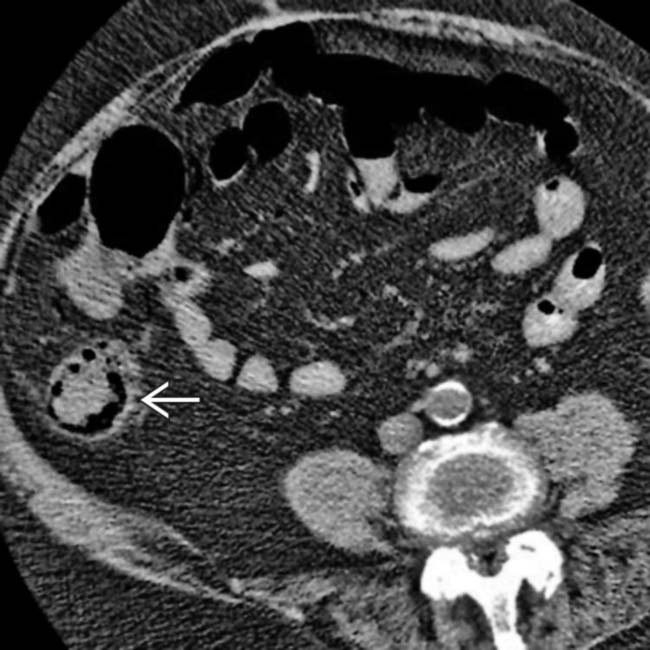
 , which is otherwise relatively normal in appearance.
, which is otherwise relatively normal in appearance.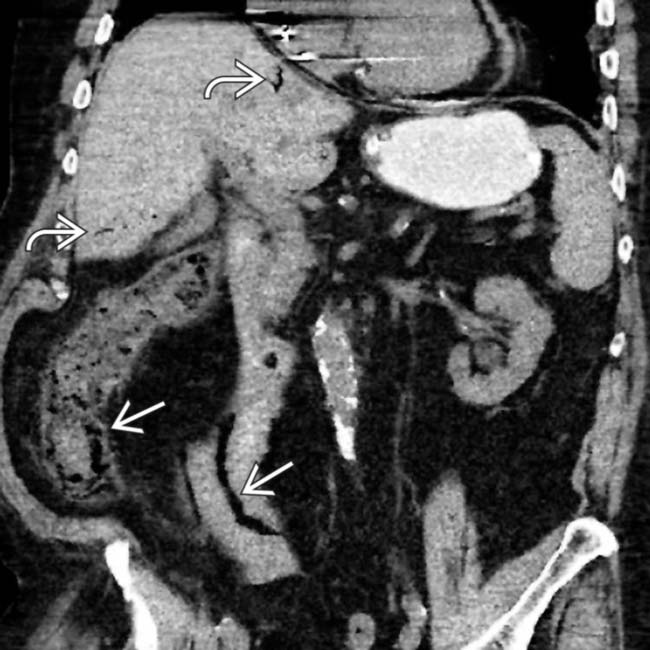
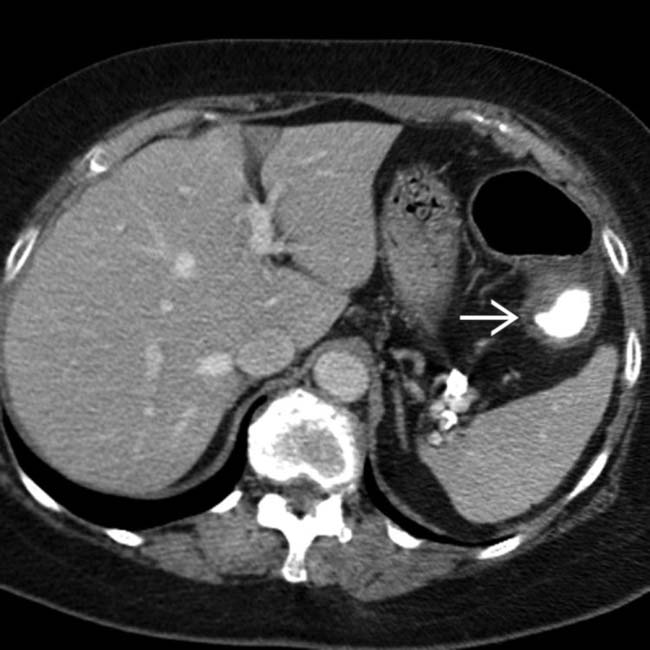
 as well as the ascending colon. Portal venous gas
as well as the ascending colon. Portal venous gas  is also present. These are typical features of thromboembolic occlusion of the SMA.
is also present. These are typical features of thromboembolic occlusion of the SMA.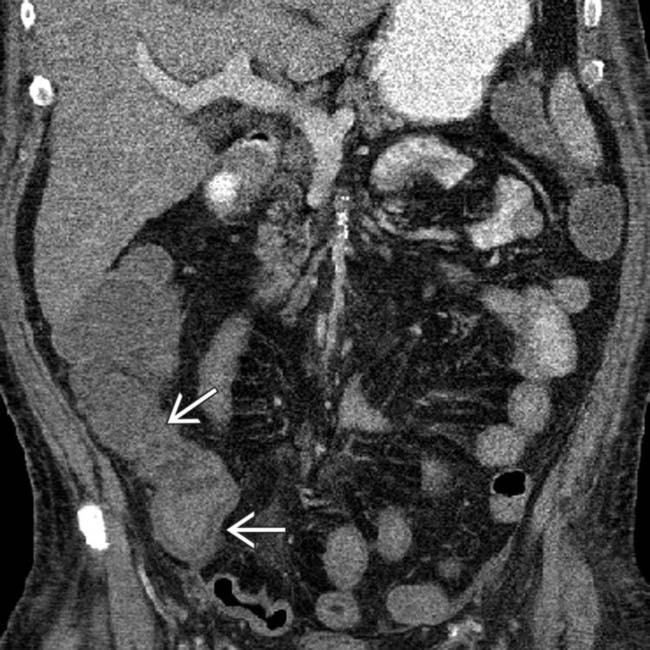
 and transverse colon (not shown).
and transverse colon (not shown).
 , whereas the distal colonic wall
, whereas the distal colonic wall  is normal. This distribution of ischemic injury likely resulted from a combination of atherosclerotic narrowing of the SMA and the hypotensive episode.
is normal. This distribution of ischemic injury likely resulted from a combination of atherosclerotic narrowing of the SMA and the hypotensive episode.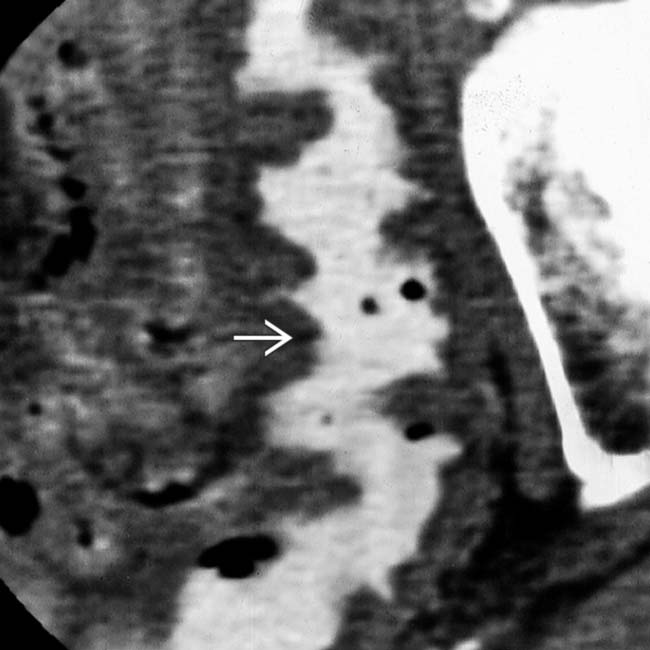
 due to submucosal hemorrhage.
due to submucosal hemorrhage.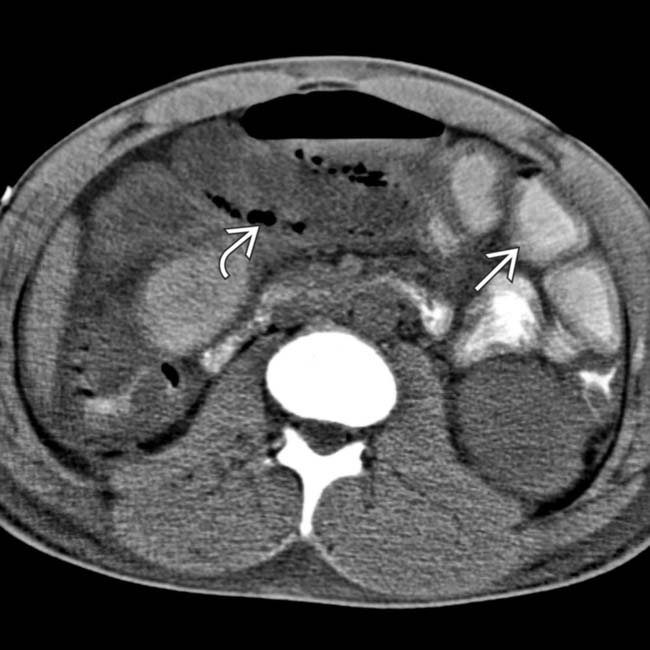
 and focal pneumatosis
and focal pneumatosis  .
.
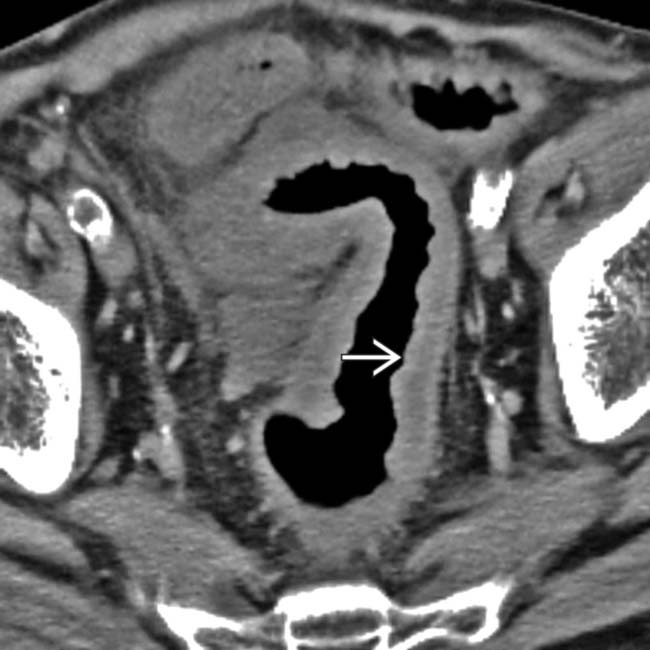
 . Note the abrupt transition to normal sigmoid colon
. Note the abrupt transition to normal sigmoid colon  .
.
 . Ischemia was confirmed endoscopically.
. Ischemia was confirmed endoscopically.
 .
.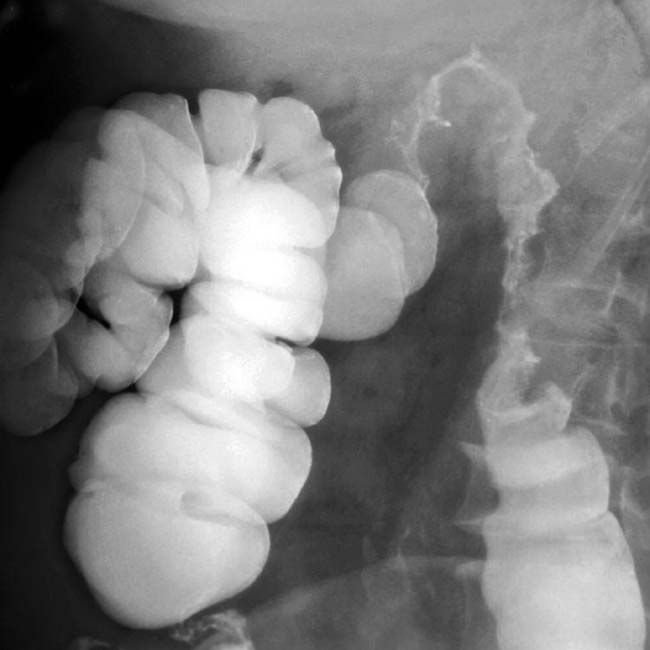
 , submucosal edema, and luminal narrowing of the colon.
, submucosal edema, and luminal narrowing of the colon.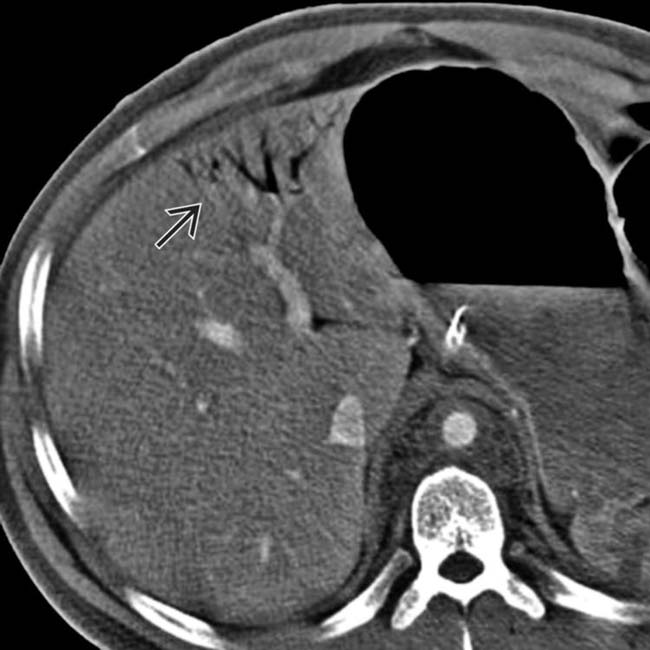
 .
.












































































 .
.
 .
.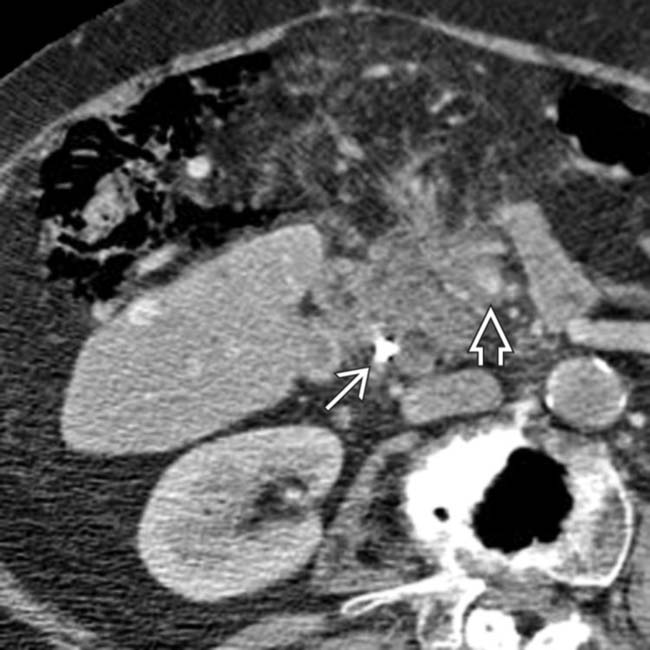
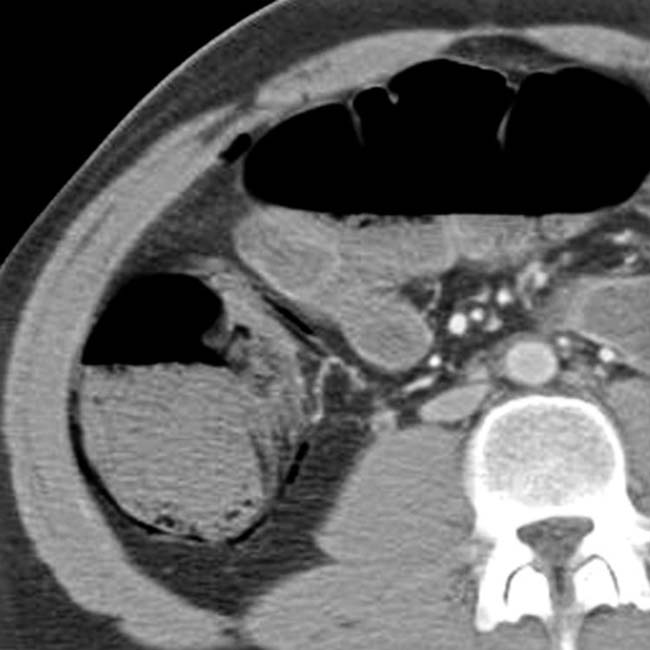
 . The superior mesenteric artery and vein
. The superior mesenteric artery and vein  are encased and narrowed. Gas is present in the colon wall.
are encased and narrowed. Gas is present in the colon wall.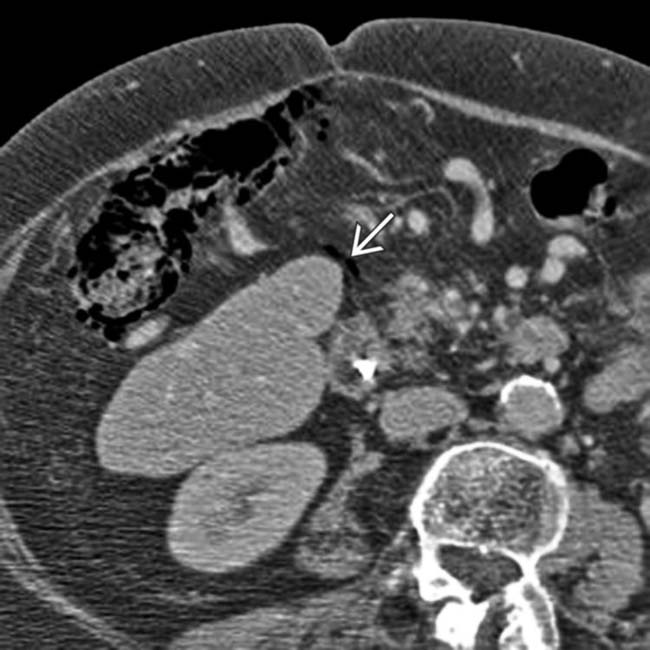
 gas present due to colon infarction.
gas present due to colon infarction.


