Solitary or multifocal strictures of variable length
• Cholangiography: Gold standard for diagnosis
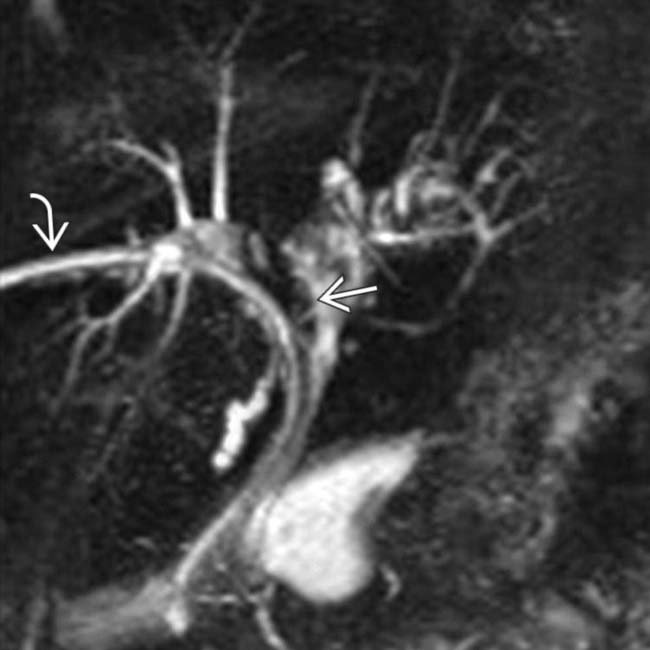
• MR: Linear high T1 signal intensity may be visualized within dilated central ducts, characteristic of biliary cast
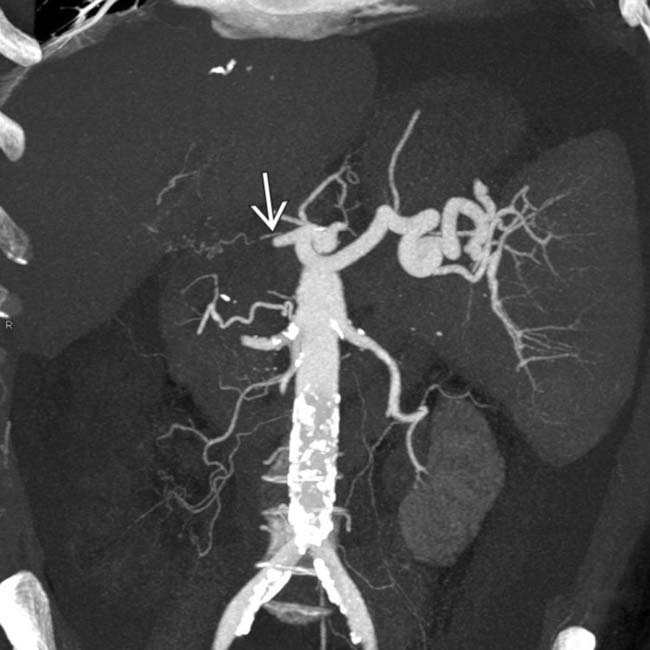
 near its origin from the celiac artery.
near its origin from the celiac artery.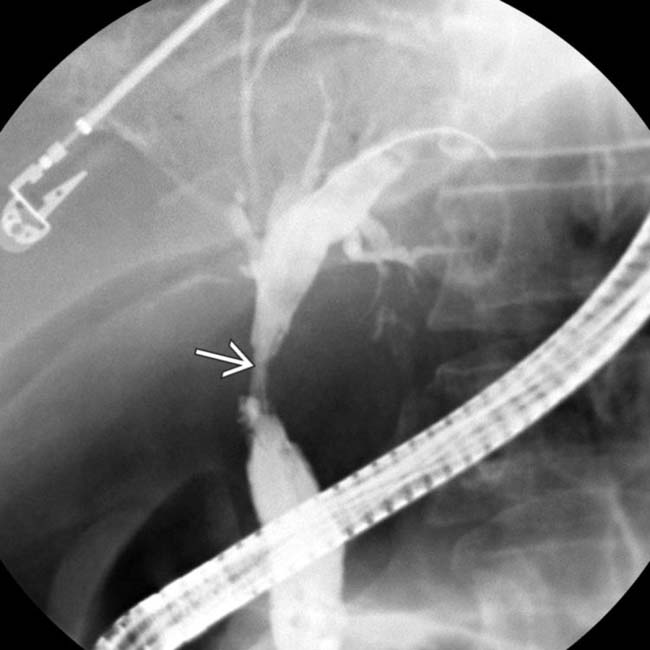
 and irregularity of the intrahepatic ducts.
and irregularity of the intrahepatic ducts.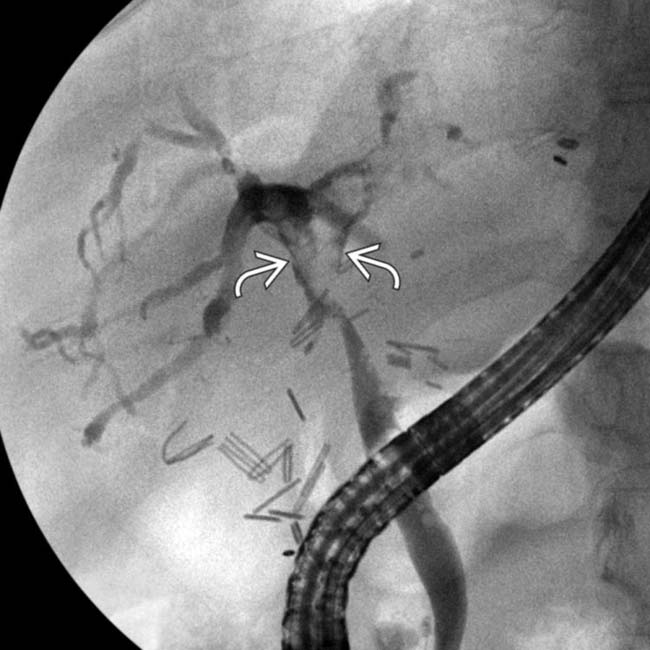
 , and diffusely irregular intrahepatic ducts. The patient’s course was complicated by portal vein thrombosis and rejection, but the hepatic artery was patent on US.
, and diffusely irregular intrahepatic ducts. The patient’s course was complicated by portal vein thrombosis and rejection, but the hepatic artery was patent on US.
 at the duct bifurcation. Multiple ischemic and immunological insults may result in the strictures and casts that are characteristic of ischemic cholangiopathy.
at the duct bifurcation. Multiple ischemic and immunological insults may result in the strictures and casts that are characteristic of ischemic cholangiopathy.IMAGING
General Features
Radiographic Findings
• Cholangiography (ERCP or PTC) is gold standard for diagnosis of ischemic cholangitis
CT Findings
• Scattered irregular biliary dilatation with bile duct wall thickening and hyperenhancement
 Presence of intrahepatic biloma or liver infarct in post-transplant setting should prompt careful assessment of hepatic artery for HAT/HAS
Presence of intrahepatic biloma or liver infarct in post-transplant setting should prompt careful assessment of hepatic artery for HAT/HAS
 Presence of intrahepatic biloma or liver infarct in post-transplant setting should prompt careful assessment of hepatic artery for HAT/HAS
Presence of intrahepatic biloma or liver infarct in post-transplant setting should prompt careful assessment of hepatic artery for HAT/HAS
MR Findings
• Hepatobiliary contrast agents (i.e., Eovist) can be used for cholangiographic images in hepatobiliary phase
• T2WI, MRCP, and T1WI C+ Eovist cholangiographic images demonstrate luminal irregularity, stenosis, and scattered biliary ductal dilatation
• Linear high T1 signal intensity may be visualized within dilated central ducts, characteristic of biliary cast
Ultrasonographic Findings
• Grayscale ultrasound
 Advanced biliary ischemia due to HAT or HAS may result in presence of intrahepatic fluid collections (bilomas)
Advanced biliary ischemia due to HAT or HAS may result in presence of intrahepatic fluid collections (bilomas)
 Advanced biliary ischemia due to HAT or HAS may result in presence of intrahepatic fluid collections (bilomas)
Advanced biliary ischemia due to HAT or HAS may result in presence of intrahepatic fluid collections (bilomas)PATHOLOGY
General Features
• Etiology
 Nonanastomotic biliary strictures initially described in setting of hepatic artery thrombosis and were thought to be a merely ischemic entity
Nonanastomotic biliary strictures initially described in setting of hepatic artery thrombosis and were thought to be a merely ischemic entity
 Biliary epithelial cells are more prone to ischemic injury
Biliary epithelial cells are more prone to ischemic injury
 Nonanastomotic biliary strictures initially described in setting of hepatic artery thrombosis and were thought to be a merely ischemic entity
Nonanastomotic biliary strictures initially described in setting of hepatic artery thrombosis and were thought to be a merely ischemic entity
 Biliary epithelial cells are more prone to ischemic injury
Biliary epithelial cells are more prone to ischemic injury
CLINICAL ISSUES
Presentation
 in the central bile ducts, compatible with ischemic cholangiopathy. A biliary drainage catheter
in the central bile ducts, compatible with ischemic cholangiopathy. A biliary drainage catheter  is in place.
is in place.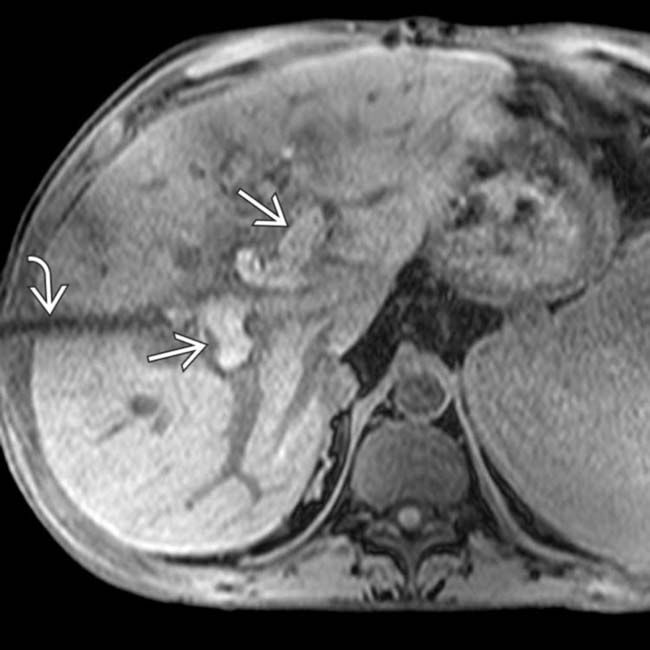
 distending the ducts. The biliary drainage catheter
distending the ducts. The biliary drainage catheter  is again noted.
is again noted.
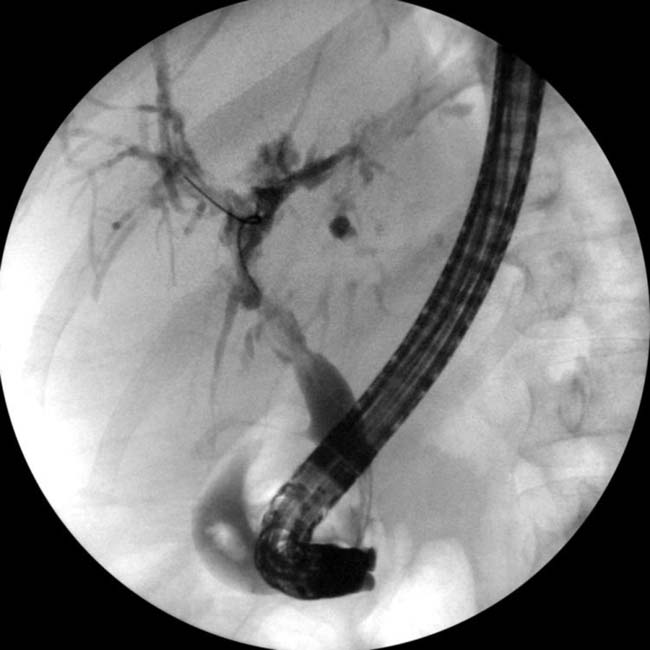

 is expanded and irregular, and the right duct
is expanded and irregular, and the right duct  is obscured by an adjacent biloma
is obscured by an adjacent biloma  . The patient was retransplanted.
. The patient was retransplanted.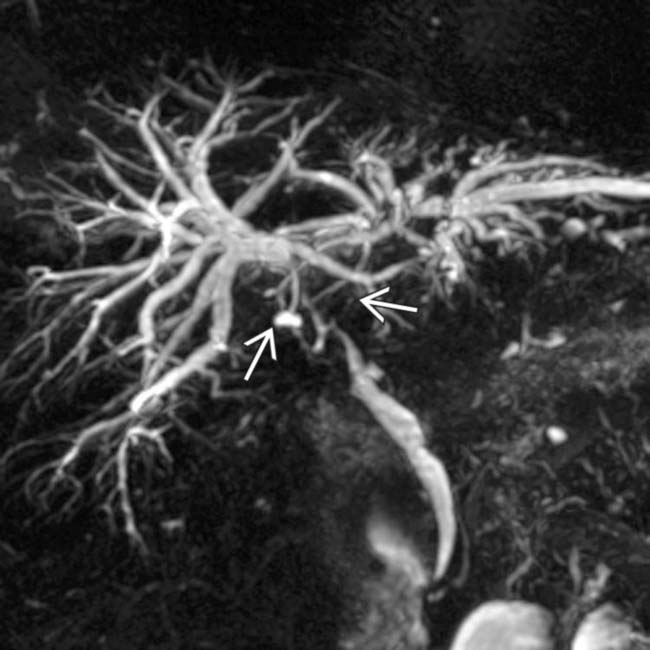
 and moderate intrahepatic ductal dilatation. The hepatic artery was patent on Doppler US. Brush biopsies of the stricture were negative, and a liver biopsy showed changes compatible with ischemic reperfusion injury.
and moderate intrahepatic ductal dilatation. The hepatic artery was patent on Doppler US. Brush biopsies of the stricture were negative, and a liver biopsy showed changes compatible with ischemic reperfusion injury.
 distending the ducts. A biliary drainage catheter
distending the ducts. A biliary drainage catheter  is in place.
is in place.
 with echogenic biliary “cast” material
with echogenic biliary “cast” material  distending the ducts.
distending the ducts.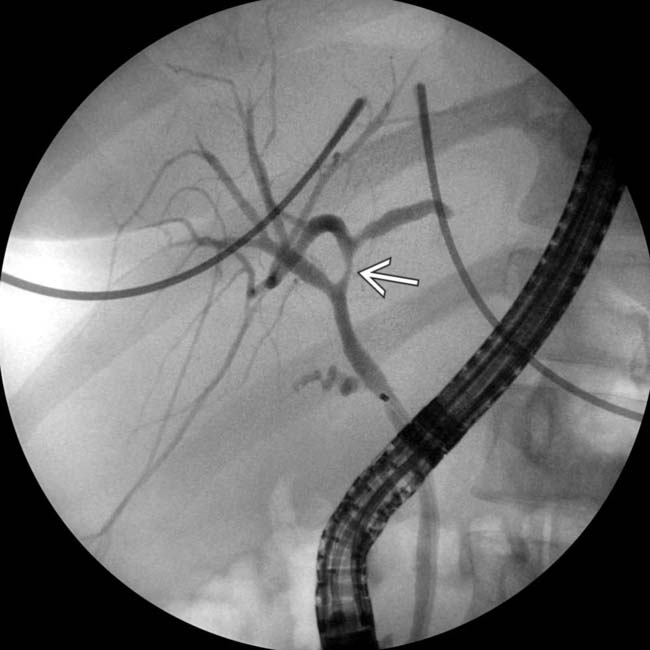
 and irregularity of the left ducts proximally.
and irregularity of the left ducts proximally.
 of the proximal hepatic artery at its origin from the celiac. Some perfusion of the liver is noted via collaterals
of the proximal hepatic artery at its origin from the celiac. Some perfusion of the liver is noted via collaterals  .
.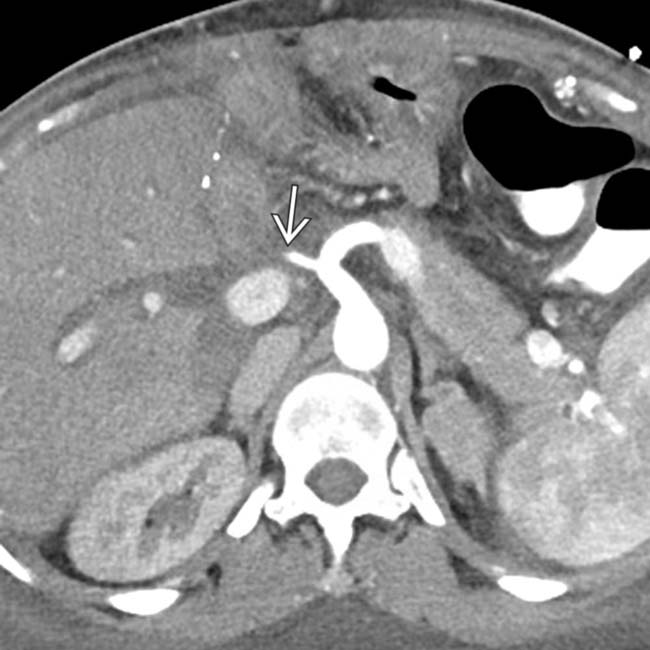
 of the proximal hepatic artery.
of the proximal hepatic artery.
 in a liver transplant patient.
in a liver transplant patient.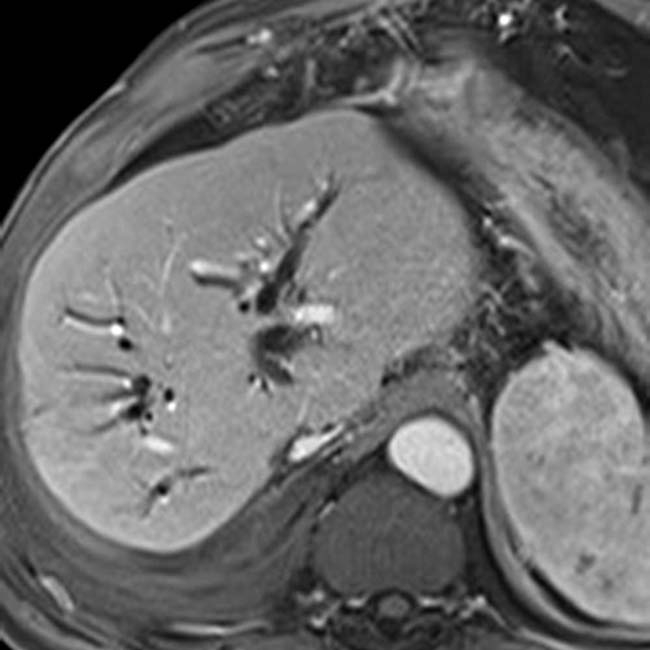

 in the liver with a branching configuration that roughly parallels the portobiliary tracts, highly suggestive of a biloma resulting from hepatic artery stenosis or thrombosis.
in the liver with a branching configuration that roughly parallels the portobiliary tracts, highly suggestive of a biloma resulting from hepatic artery stenosis or thrombosis.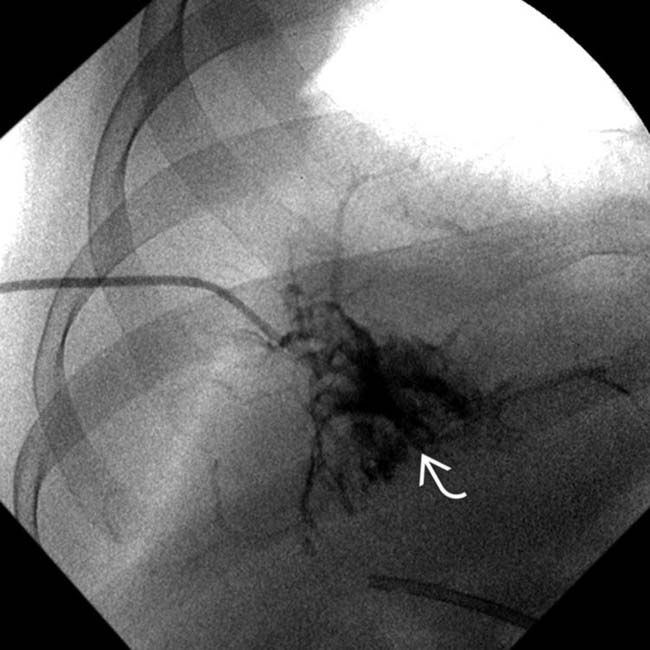
 of bile and contrast medium.
of bile and contrast medium.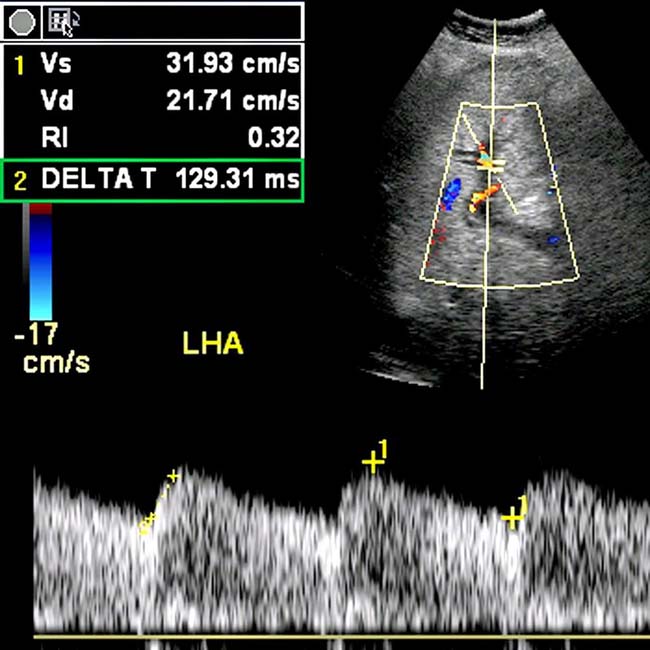
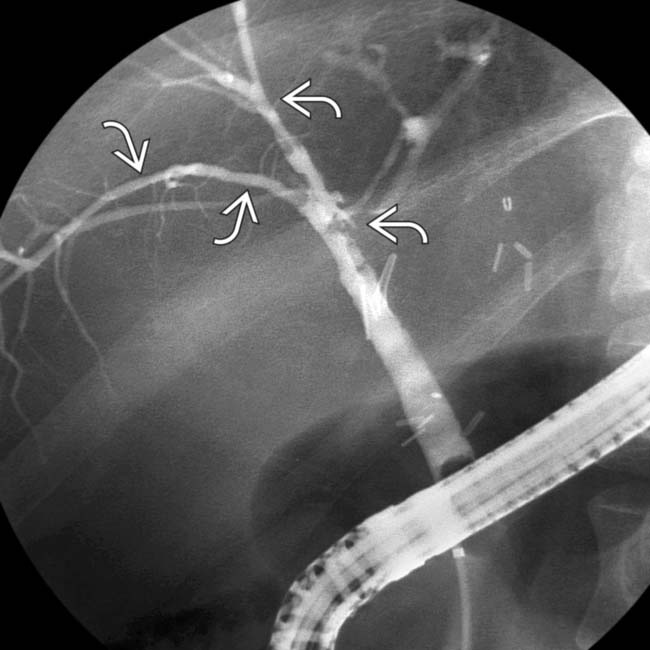
 , characteristic features of ischemic cholangiopathy. Irregularity improved with successive stent exchanges.
, characteristic features of ischemic cholangiopathy. Irregularity improved with successive stent exchanges.
 within the right common bile duct. The hepatic artery was widely patent at Doppler and CT examinations.
within the right common bile duct. The hepatic artery was widely patent at Doppler and CT examinations.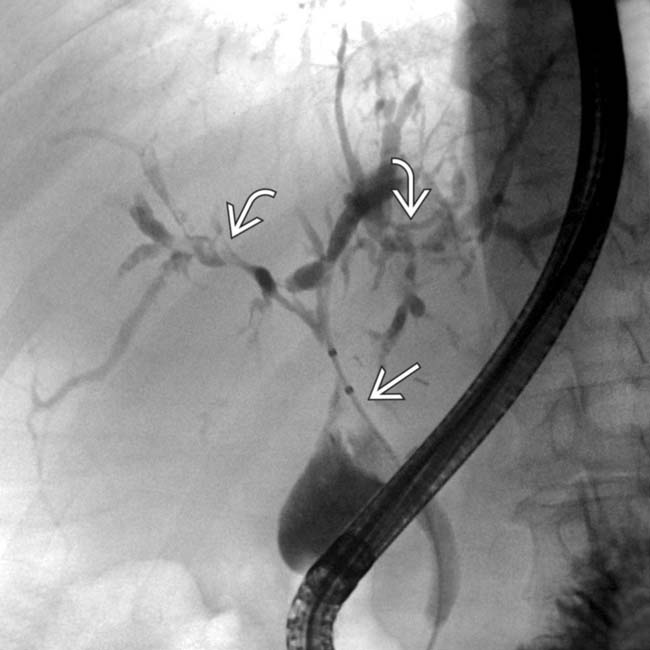
 and extrahepatic biliary casts
and extrahepatic biliary casts  . Note extensive intrahepatic biliary strictures and beading. Biliary ischemic injury may be due to a variety of microangiopathic and immunogenetic insults.
. Note extensive intrahepatic biliary strictures and beading. Biliary ischemic injury may be due to a variety of microangiopathic and immunogenetic insults.
 within dilated bile ducts. Treatment included multiple stent exchanges and cast retrieval.
within dilated bile ducts. Treatment included multiple stent exchanges and cast retrieval.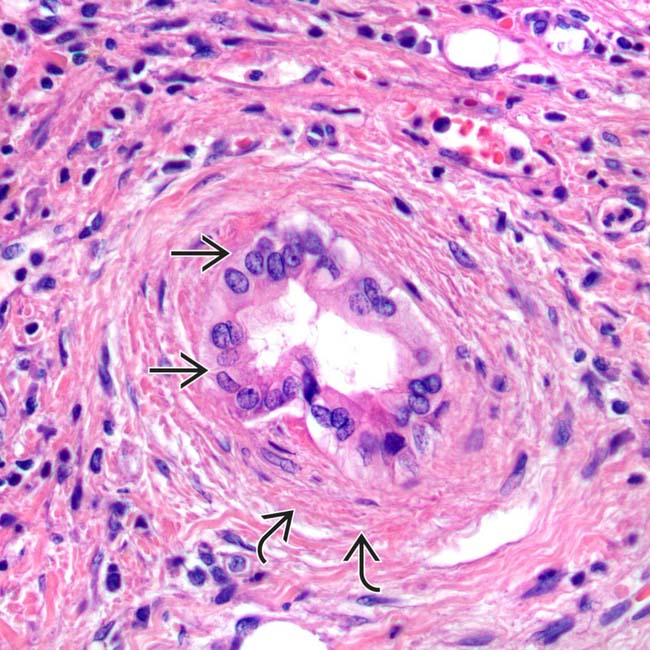
 (uneven nuclear spacing and loss of polarity) and periductal fibrosis
(uneven nuclear spacing and loss of polarity) and periductal fibrosis  in chronic ischemic cholangitis.
in chronic ischemic cholangitis.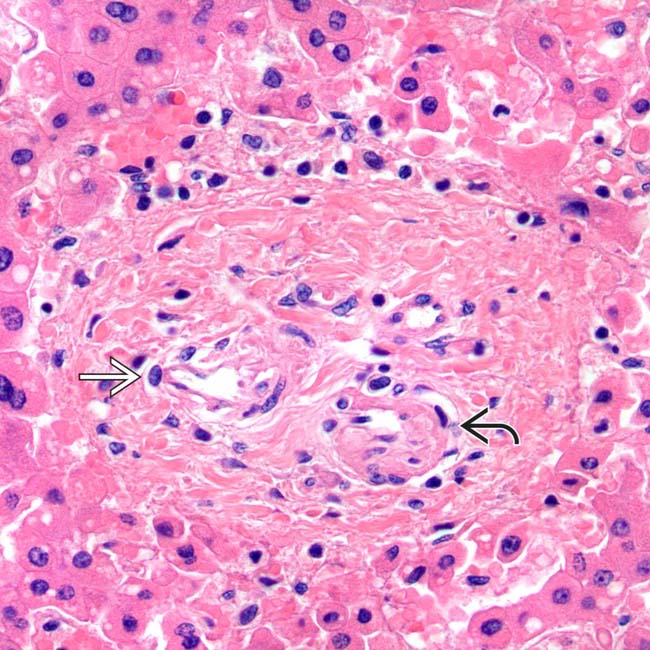
 and portal vein
and portal vein  branches but lacks an identifiable bile duct profile.
branches but lacks an identifiable bile duct profile.


































































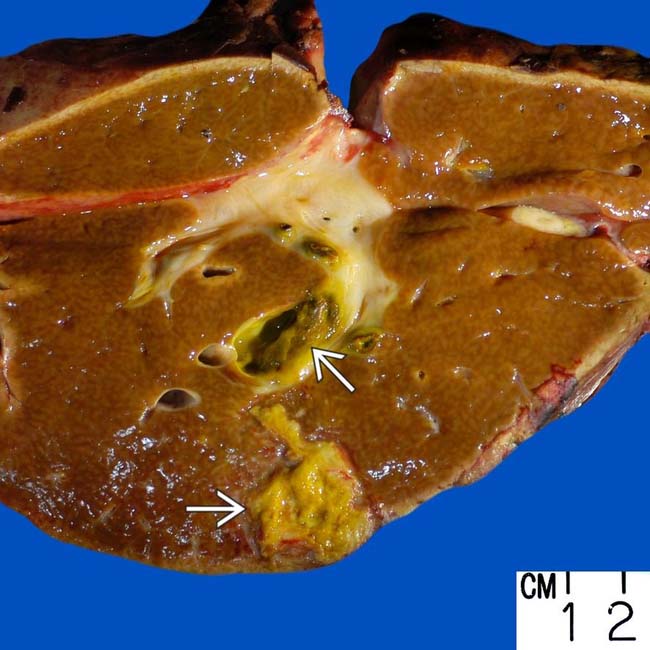
 is shown in this liver.
is shown in this liver.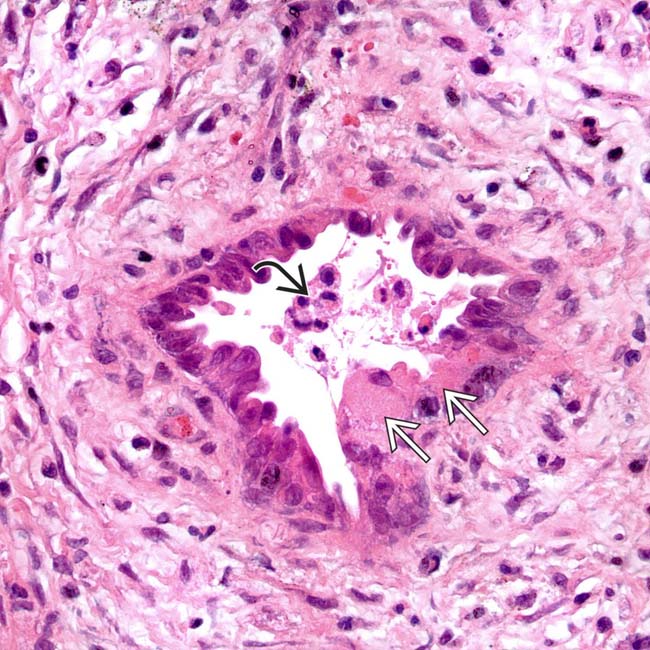
 and sloughing into the bile duct lumen
and sloughing into the bile duct lumen  to form biliary casts in acute ischemic cholangitis.
to form biliary casts in acute ischemic cholangitis.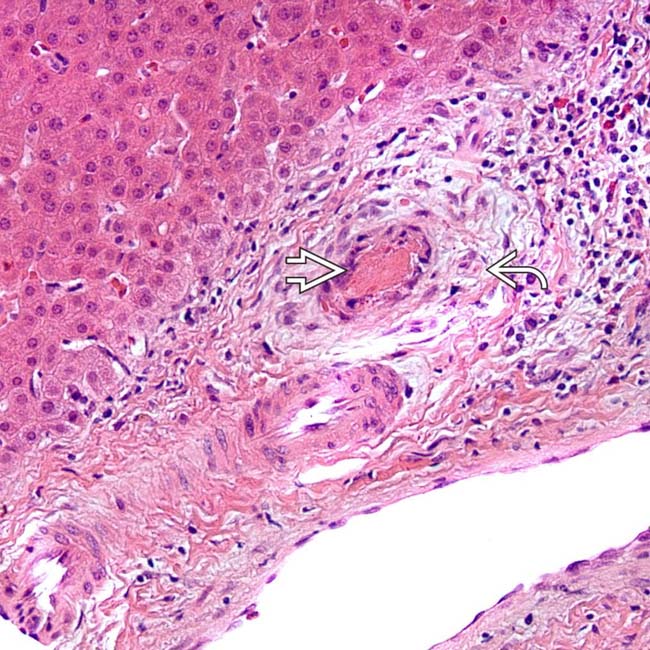
 in acute ischemic cholangitis. There is also mild portal inflammation and periductal edema
in acute ischemic cholangitis. There is also mild portal inflammation and periductal edema  .
.


