FIGURE 12.1 Acute versus cumulative irritation—a thought starter.
So what should be done in practice? Firstly, it is appropriate to adopt a protocol in which the skin exposure bears some resemblance to real-life exposure. Exposure may need to be repetitive, carried out for days, or even weeks. Next, it is essential to ensure that there is sufficient sensitivity built into the study to gain a meaningful response—a wholly negative set of skin reactions means nothing in isolation. Therefore, what is required is a panel with a sufficient number of volunteers and/or selection of panelists known to react with greater vigor to the type of irritancy problem associated with test material. It is almost always necessary to include a positive control material—a common choice is the anionic surfactant SLS, but it should generally be a last resort, since a better positive control is a related chemical or product formulation, relevant to the test material. For example, a clinical study of a new hand wash detergent formulation could involve several short exposures per day, with rinsing on one skin site, compared to a positive control site in which a product known to produce skin irritation in the exposed population is deployed. This study can then compare both the time to develop a cumulative irritant response, the nature and the degree of the irritant response, and as with all clinical studies, any observations on other aspects of the skin reaction, including sensory events. Ultimately, the question is “Does my clinical study have scientific integrity?”
There is one additional general question that has to be considered—how should any irritant reactions be assessed/measured? An argument can be made that properly trained skin assessors are more than sufficient to the task (14). However, and notwithstanding the additional time and expense, a good case can be made for use of one or (more usually) more instrumental assessment techniques (reviewed in the study by Berardesca and Maibach (15)).
Urticaria
In the preceding sections, it has been documented that urticaria has little relationship to skin irritation. This should hardly be a surprising statement. The mechanisms driving the two reactions are not at all the same (even if we do not necessarily always know what those mechanisms are!). Irritation is largely some combination of damage to the skin barrier function together with the activation of inflammatory pathways and, even with the acute response, occurs over a time period measured in hours/days (16). Skin contact urticaria on the other hand (we are not speaking here of systemic disease types classed as urticaria) arises within a few minutes and typically fades over an hour or so. Commonly, two types of contact urticaria are described (17). Here, we will focus only on the nonimmunologic variety, avoiding the complexity of immunoglobulin E-mediated protein allergic responses.
Nonimmunologic contact urticaria is perhaps not only particularly common, but also relatively easy to screen for. A good number of common chemical urticants are known, and from these, valuable insights have been derived, if not into the precise mechanism(s) of action, at least into the general characteristics of the response (18). Firstly, almost all individuals will produce a typical erythematous response, perhaps with a wheal, a few minutes after skin contact with a strong urticant (e.g., ethyl nicotinate, dimethylsul phoxide [DMSO]). Weaker urticants (e.g., benzoic acid, sorbic acid) do not produce any reaction in many subjects, particularly at lower concentrations (17). However, the use of a range of urticants shows that an individual giving a strong reaction to one urticant is in no way predictive of the reaction of that individual to a different urticant (19). The use of these benchmarks may permit the identification and calibration of a suitable volunteer panel.
So what should be done in practice? Skin contact urticaria is an acute response to a single contact (although of course it may be experienced repetitively). Thus, the use of a test panel, perhaps comprised of individuals who are known to have a greater level of response to a range of weaker urticants, can be exposed to the test agents, for example, on volar forearm skin sites, for 10–20 minutes, with assessment of responses from initial contact up to 60 minutes (longer if the reaction has not subsided). Occlusion may be used to enhance the sensitivity of the study (e.g., the study by Basketter and Wilhelm (19)).
Sensory Effects
As has already been mentioned earlier, any study involving human volunteers offers the benefit that those same volunteers can inform on any dermal effects that they perceive. However, although that aspect of clinical studies is extremely valuable in its own right, there is also the possibility of undertaking specifically directed assessment of sensory effects. Again, mention has already been made of the LAST (10). Unfortunately, a common error made has been to assume that individuals who are more susceptible to lactic acid-induced stinging are also more likely to experience other sensory responses, such as burning or itching. The most compelling demonstration of the problem arises from a study using DMSO (3). This substance generates many responses (including urticaria and, later, irritation), but the experiment reported using 86 volunteers also noted that stinging, tingling, itching, and burning triggered by DMSO was more or less equal in lactic acid stingers and nonstingers, with the latter if anything a little higher. Importantly, the stinging status was confirmed contemporaneously with the DMSO application.
Conclusions
Sensitive skin is an elusive entity (20). A heightened reactivity to one aspect of nonimmune skin responses is in no way indicative of a generally elevated sensitivity to any type of skin insult. The simple message therefore is that a test panel has to be selected according to the specific end point of interest. This cannot be achieved by using a lactic acid stinging screen on the nasolabial fold or an SLS patch test for acute irritancy any more than by using subjects with self-reported sensitive skin. Where human testing is conducted on sensitive skin in an attempt to use higher reactors as an enhanced indicator for a wider consumer population, the chance of achieving a scientifically defensible outcome is at best poor. However, where the testing is established with panels suitably screened for the particular end point of concern, where it employs sufficient numbers of individuals and contains concurrent positive and negative control materials, it can offer the optimum strategy for the identification and management of potentially adverse skin effects in a susceptible population.
REFERENCES
1. Marriott M, Basketter DA, Cooper K. Complex problem of sensitive skin. In: Berardesca E, Fluhr J, Maibach HI, editors. Sensitive Skin Syndrome. Boca Raton, FL: Taylor & Francis; 2006a. p. 61–65.
2. Marriott M, Basketter DA, Cooper K, Peters L. Identification of a sensitive skin panel. In: Berardesca E, Fluhr J, Maibach HI, editors. Sensitive Skin Syndrome. Boca Raton, FL: Taylor & Francis; 2006b. p. 107–119.
3. Coverly J, Peters L, Whittle E, Basketter DA. Susceptibility to skin stinging, non-immunologic contact urticaria and skin irritation—Is there a relationship? Contact Dermat. 1998; 38:90–95.
4. Frosch P, Kligman AM. Method for appraising the sting capacity of topically applied substances. J Soc Cosmet Chem. 1977; 28:197–209.
5. Lammintausta K, Maibach HI, Wilson D. Mechanisms of subjective (sensory) irritation: Propensity to non-immunologic contact urticaria and objective irritation in stingers. Dermatosen. 1988; 36:45–49.
6. Basketter DA, Griffiths HA. A study of the relationship between susceptibility to skin stinging and skin irritation. Contact Dermat. 1993; 29:185–188.
7. Schliemann S, Antonov D, Manegold N, Elsner P. The lactic acid stinging test predicts susceptibility to cumulative irritation caused by two lipophilic irritants. Contact Dermat. 2010; 63:347–356.
8. Schliemann S, Antonov D, Manegold N, Elsner P. Sensory irritation caused by two organic solvents-short-time single application and repeated occlusive test in stingers and non-stingers. Contact Dermat. 2011; 65:107–114.
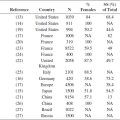
9. Modjtahedi SP, Maibach HI. Ethnicity as a possible endogenous factor in irritant contact dermatitis: comparing the irritant response among Caucasians, blacks and Asians. Contact Dermatitis 2002; 47: 272–278.
10. Robinson MK. Population differences in acute skin irritation responses: Race, sex, age, sensitive skin and repeat subject comparisons. Contact Dermat. 2002; 46:86–93.
11. Lee E, Kim S, Lee J, Cho SA, Shin K. Ethnic differences in objective and subjective skin irritation response: An international study. Skin Res Technol. 2014; 20:265–269.
12. Basketter DA, Jirova D, Kandarova H. Review of skin irritation/corrosion hazards on the basis of human data: A regulatory perspective. Interdiscip Toxicol. 2012; 5:98–104.
13. Hannuksela A, Hannuksela, M. Irritant effects of a detergent in wash and chamber tests. Contact Dermat. 1995; 32:163–166.
14. Basketter DA, Reynolds FS, Rowson M, Talbot C, Whittle E. Visual assessment of human skin irritation: A sensitive and reproducible tool. Contact Dermat. 1997; 37:218–220.
15. Berardesca E, Maibach NI. Non-Invasive Diagnostic Techniques in Clinical Dermatology. Berlin: Springer; 2014.
16. Chew AL, Maibach HI. Irritant Dermatitis. Berlin: Springer-Verlag; 2006.
17. Basketter DA, Lahti A. Immediate contact reactions. In: Johansen JD, Frosch PF, Lepoittevin JP, editors. Contact Dermatitis. 5th edition. Berlin: Springer; 2011. p. 137–154.
18. Gimenez-Arnau A, Maibach HI. Contact Urticaria Syndrome. Boca Raton, FL: CRC Press; 2014.
19. Basketter DA, Wilhelm KP. Studies on non-immune immediate contact reactions in an unselected population. Contact Dermat. 1996; 35:237–240.
20. Berardesca E, Fluhr JW, Maibach HI. Sensitive Skin Syndrome. New York: Informa Healthcare; 2006.