Intussusception
Intussusception is an acquired invagination of the bowel into itself, usually involving both small and large bowel (Fig. 108-1). The more proximal bowel that invaginates into more distal bowel is termed the intussusceptum, whereas the recipient bowel that contains the intussusceptum is termed the intussuscipiens. Invagination of the bowel leads to edema, and ischemic changes eventually supervene; thus intussusception is an urgent condition, but prolonged delay in diagnosis is not uncommon, resulting in increased risk for patients to present with obstruction, necrosis, and bowel perforation.
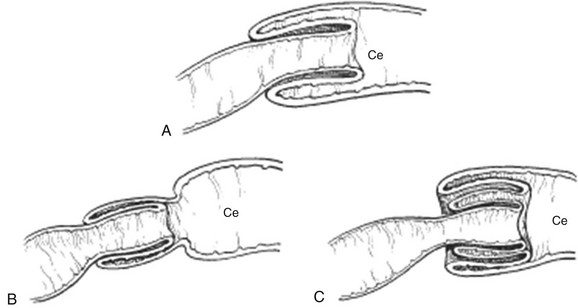
Figure 108-1 The common types of infantile intussusception, in longitudinal section.
A, Ileocecal. B, Ileoileal. C, Ileoileocolic. Ce, Cecum.
Intussusception occurs with an incidence of at least 56 per 100,000 children per year in the United States, and it is the most common cause of small bowel obstruction in children.1 In frequency, it is second only to pyloric stenosis as a cause of gastrointestinal tract obstruction in children, occurring in boys more often than girls at a ratio of 3 : 2. Classic pediatric intussusception involves invagination of the distal ileum into the colon, as ileocolic or ileoileocolic intussusception; however, intestinal intussusception may occur along the entire length of the bowel from the duodenum to the colon. Cases of intussusception range from the classic, symptomatic, and urgent presentation, to short-segment, transient, and asymptomatic events, typically isolated to the small bowel, and seen increasingly on ultrasound or on computed tomography (CT) of the abdomen performed for other indications (e-Fig 108-2).2 This chapter will focus on ileocolic and ileoileocolic intussusception.
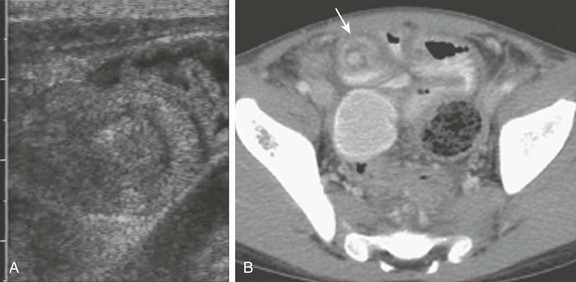
e-Figure 108-2 Transient intussusception of the small bowel.
A, A transverse image of ileoileal intussusception incidentally identified in an infant with gastroenteritis; on longitudinal image it measured <3 cm, and it could not be identified on rescanning of the area. B, An abdominopelvic computed tomography image of a young child undergoing routine follow-up imaging of a testicular tumor. An asymptomatic, short-segment, small bowel intussusception (arrow) resolved spontaneously. (A, Courtesy Dr. Marta Hernanz-Schulman, Nashville, TN.)
Etiology
Most cases of ileocolic intussusception occurring in children are idiopathic. It is hypothesized that the typical childhood ileocolic intussusception results from hypertrophied lymphoid tissue in the terminal ileum (Peyer patches). Some reports suggest a viral etiology, most commonly adenovirus, but enterovirus, echovirus, and human herpes virus 6 also have been implicated.1,3 An accompanying pathologic lead-point mass lesion may be present in 5% to 6% of all children,4,5 particularly when intussusception occurs outside of the typical idiopathic age range or when symptomatic intussusception is confined to the small bowel or the colon.
Rotavirus Vaccine
Shortly after the first rotavirus vaccine was introduced in the United States in 1998 for routine vaccination of infants at ages 2, 4, and 6 months, several reports to the Centers for Disease Control and Prevention suggested an association between the vaccine and intussusception. The vaccine was removed from the world market in 1999. Subsequent investigations have demonstrated clear benefits in reducing morbidity and mortality, although some authors report a very small risk of intussusception after rotavirus vaccination.6,7 Two new vaccines are now available.
Pathologic Lead Points
Approximately 5% to 6% of intussusceptions in children are caused by pathologic lead points, either focal masses or a diffuse bowel wall abnormality.4,5,8 The traditional view is that focal lead points are more common in older children. Although the absolute numbers of lead points are approximately equal in infants and in older children, the percentage of lead points in infants is lower because of the greater number of intussusceptions occurring in this age group.4 The most common focal lead points are (in decreasing order of incidence) Meckel diverticulum, duplication cyst, polyp, and lymphoma. In older children, lymphoma is the more likely lead point, typically Burkitt lymphoma. Diffuse lead points are most commonly associated with cystic fibrosis or Henoch-Schönlein purpura. Colonic polyps can result in colocolic intussusception.
Clinical Presentation
Idiopathic intussusception occurs most commonly in infants between 2 months and 3 years of age, with a peak at age 5 to 9 months; authors of studies with a large series report that 57% to 85% of cases present before the age of 1 year (average, 67%).8,9
The classic clinical presentation of the child with intussusception is colicky abdominal pain, vomiting, bloody stools, and a palpable abdominal mass.9 Children with intussusception should be diagnosed as early as possible to avoid bowel ischemia, necrosis, and surgery; however, this goal remains elusive. The clinical signs and symptoms of intussusception are often nonspecific and may overlap with those of gastroenteritis, malrotation with volvulus, and in older children, Henoch-Schönlein purpura. The classic triad of colicky abdominal pain (58% to 100% of cases), vomiting (up to 85% of cases), and bloody stools (up to 75% of cases)10,11 is present in less than 25% of children.10,12 No reliable clinical prediction models exist that can identify all children with intussusception.12–14 In one study, it was found that only 50% of children were correctly diagnosed at initial presentation to a health care provider.15
Clinical Predictors of Intussusception and Nonsurgical Reduction
The most important factor, either alone or in combination with other factors, that predicts an unsuccessful enema reduction is a longer duration of symptoms; 48 to 72 hours typically is considered a significant delay.8,9 Other factors associated with lower rates of successful reduction include age less than 3 months, dehydration, small bowel obstruction, and intussusception encountered in the rectum (resulting in a 25% reduction rate).8,9,15–17 Additional findings that affect bowel edema, bowel viability, and success of nonsurgical reduction relate to imaging findings and are addressed in the next section. On the basis of sonographic or enema diagnosis before surgery, the rate of spontaneous reduction is estimated to be 10%.4,18,19
Diagnosis and Imaging
Box 108-1 summarizes the evidence regarding imaging management of intussusception.
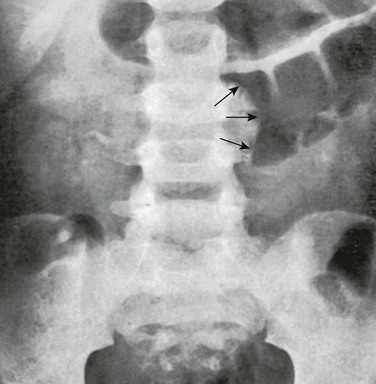
Abdominal Radiographs
Abdominal radiographs have a limited sensitivity and specificity for the detection of intussusception, even when viewed by experienced pediatric radiologists.9,20 Sargent and colleagues16 reported a sensitivity of 45% in 60 children when they were evaluated prospectively by pediatric radiologists, using an enema as the reference standard. Adding a left side down decubitus has been shown to improve sensitivity.21 The presence of a curvilinear mass within the course of the colon (the crescent sign), particularly in the transverse colon just beyond the hepatic flexure, is a nearly pathognomonic sign of intussusception (Fig. 108-3). The absence of stool or recognizable colonic gas in the ascending colon is one of the more suggestive signs of intussusception on radiographs. However, fluid filling the ascending colon in a patient with gastroenteritis may falsely suggest intussusception, and small bowel gas located in the right abdomen on radiographs may mimic ascending colon or cecal gas.
Ultrasonography
Ultrasound is highly sensitive in the detection of intussusception (see Table 108-1), even when it is performed by relatively inexperienced operators and with equipment that is no longer state of the art.22,23 Although the diagnosis can be confirmed when the enema procedure is performed, ultrasound is the primary imaging modality for the initial diagnosis outside of the United States; it is used by 93% of European pediatric radiologists,24 as well as by a growing number of pediatric radiologists in the United States. Initial evaluation by ultrasound circumvents the more invasive enema in patients who do not have intussusception, and it allows diagnosis of other conditions, such as mesenteric adenitis or colitis, for which performance of an enema would not be the procedure of choice.12,25,26
Table 108-1
Sensitivity and Specificity of Diagnostic Imaging for Ileocolic Intussusception
| Test | Sensitivity (%) | Specificity (%) |
| Abdominal radiograph | 45 | Unknown |
| Ultrasound | 98-100 | 88-100 |
| Enema* | 100 | 100 |
Intussusception can be diagnosed by ultrasound when a donut, target, or “pseudokidney” sign is seen, most often in the right upper quadrant of the abdomen.27 This appearance arises from intussuscepted bowel and mesentery within the intussuscipiens, producing the donut or target appearance on transverse images and a hypoechoic mass with hyperechoic center on longitudinal images; the hyperechoic center represents the intussuscepted mesentery. Using a linear transducer, the more specific bowel-within-bowel appearance can be seen, and the leading edge of the intussusception can be inspected to confirm that a pathologic lead point is not present (Fig. 108-4). Optimal sonographic techniques are well described,26–28 and there are no known contraindications to, or complications resulting from, ultrasound used for this purpose.
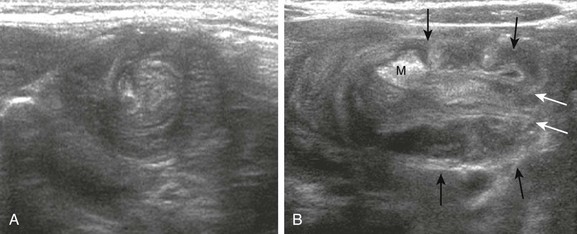
Figure 108-4 Intussusception.
A, A 3-month-old boy with intussusception. A transverse ultrasound image through the intussusceptum complex shows the donut or target sign, with intussusceptum composed of small bowel, nodes, and mesentery surrounded by the intussuscipiens. B, A longitudinal section of intussusception in the same patient as depicted in part A. The image shows the terminal end of the intussusception, with the inner and outer sleeves of the intussusceptum (white arrows) containing the intussuscepted mesentery (M). Black arrows outline the outer edge of the intussuscipiens. Note that no lead point is present. (Courtesy Dr. Marta Hernanz-Schulman, Nashville, TN.)
Ultrasound evaluation in children suspected of intussusception has been suggested to reduce cost, radiation exposure, and anxiety in both patients and parents over the discomfort of the enema.12 The accuracy of ultrasound evaluation approaches 100% with a sensitivity of 98% to 100% and a specificity reported at 88% to 100%.12,22,23,29 Its cost effectiveness, of course, depends on the prevalence of intussusception, because very few positive diagnoses would be expected in a population in which the prevalence of intussusception is very low.
Ultrasound Predictors of Enema Reducibility and Bowel Necrosis
Anechoic fluid trapped between the intussusceptum and the intussuscipiens has been associated with lack of reducibility, whereas abundant flow on color Doppler interrogation is a predictor of reducibility (Fig. 108-5).25,30 Free intraperitoneal fluid in small or moderate amounts is present in approximately half of children,27 and reports are conflicting as to whether free peritoneal fluid is associated with fewer successful reductions.18,28 Similarly, authors of some reports note that a thicker bowel wall is associated with fewer successful enema reductions, but others have not been able to verify this association. Other authors report that the presence of lymph nodes within the intussusceptum complex is associated with decreased success of reduction.22,27,31 Although some of these findings are associated with fewer successful reductions, none represents a contraindication to enema reduction. Contraindications to enema reduction are signs of peritonitis or free intraperitoneal air.
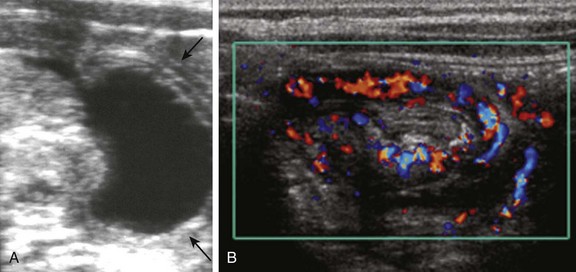
Figure 108-5 Intussusception.
A, Trapped fluid in an infant with intussusception. Fluid is visible at the leading edge of the intussusceptum complex. Arrows point to the outer edge of the intussuscipiens. B, A color Doppler transverse image of the right flank in a different patient outlines abundant flow to intussusceptum and intussuscipiens. The intussusception was successfully and rapidly reduced with air enema. (A, Courtesy Dr. Marta Hernanz-Schulman, Nashville, TN.)
Pathologic Lead Points
The detection of lead points by imaging is challenging. Ultrasound is the noninvasive standard of reference (Fig. 108-6). Ultrasound is reported to identify approximately 66% of lead points,32 whereas approximately 40% are identified by positive-contrast liquid enema.4,8,9,32 Air enema has a lower rate of detection (11%), leading some investigators to suggest that ultrasound be used afterward to search for lead points.19 However, such an approach would be hindered by air introduced during the enema, and it seems to offer little advantage over a pre-enema diagnostic ultrasound examination. Other cross-sectional imaging modalities, such as CT, can be used for further evaluation in selected patients (see Fig. 108-7).
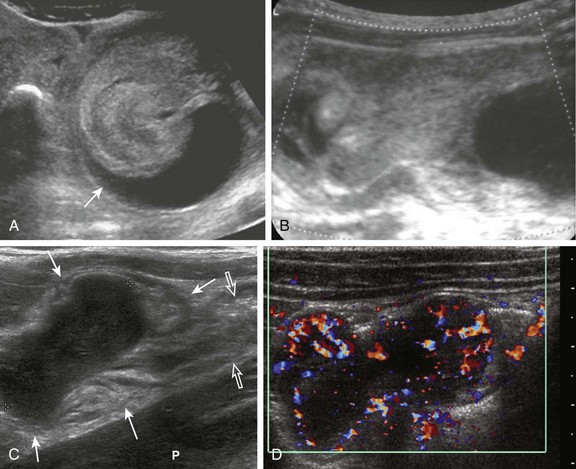
Figure 108-6 Lead points.
A, An adolescent boy with Burkitt lymphoma presenting with intussusception. An ultrasound image shows the intussuscepted mass and bowel, with anechoic fluid (arrow) trapped within the lumen of the intussuscipiens adjacent to the intussusceptum. B, A 3-month-old infant with intussusception as a result of an ileal duplication cyst that is acting as a lead point. Note the difference in appearance from that of trapped fluid in a child without a lead point (Fig. 108-5, A). C and D, 8-year-old boy presenting with severe, intermittent abdominal pain. Examination of the right lower quadrant shows an anechoic, solid mass (between crosshairs) with abundant flow on color Doppler interrogation (D), intussuscepted into the cecum (arrows). Open arrows indicate the terminal ileum. P, Psoas muscle. The pathologic diagnosis was Burkitt lymphoma. (B, Courtesy Dr. Marta Hernanz-Schulman, Nashville, TN.)
CT and MRI are not part of the routine evaluation of suspected intussusception in children, although CT may be the initial modality in a child presenting with atypical abdominal pain. If the examination is done for other reasons, the intussusception should be recognized either in the cross-sectional or longitudinal plane, with the characteristic bowel-within-bowel appearance. As is the case with ultrasound, attention should be given to the potential existence of a lead point, such as an ileal duplication cyst in a young infant, or Burkitt lymphoma in an older child (Fig. 108-7).
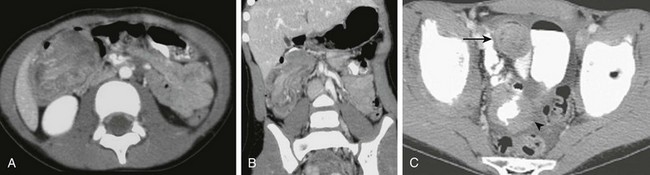
Figure 108-7 Intussusception on computed tomography (CT) images.
A and B, Axial and coronal reformatting of a CT scan of a 6-year-old girl presenting with abdominal pain. The examination shows an intussusception with a solid mass at the leading end in the proximal transverse colon; the pathologic diagnosis was Burkitt lymphoma. C, CT in an adolescent with Burkitt lymphoma presenting with abdominal pain. The examination shows both the intussusception in the right lower quadrant anteriorly (arrow) and also ascites and tumor caking (arrowhead) on the outer wall of a loop of ileum dorsal to the intussusception.
Treatment
Enema reduction should be undertaken in children with intussusception after surgical consultation. As previously indicated, the only absolute contraindications to enema reduction are signs of peritonitis on clinical examination or free air on abdominal radiographs (Box 108-2). The rate of successful overall reduction is better with air enema than with liquid enema, but the outcome depends on the patient’s risk factors and on the experience of the radiologist. Children with intussusception have fewer surgeries and a lower cost of care when they are treated at a children’s hospital, where staff tend to have greater familiarity with the condition, along with greater expertise and experience with nonoperative reduction and expedient management of potential complications.33 Between 1979 and 1997, 323 intussusception-associated deaths in U.S. infants were reported to the Centers for Disease Control and Prevention, with a higher rate of intussusception-related deaths among infants whose mothers were younger than 20 years old, unmarried, and nonwhite and who had less than a grade 12 education, suggesting that reduced access to specialized care or delay in seeking care contribute to the mortality risk.1
Enema Techniques and Reduction Rates
For reduction of intussusception, the air enema is considered superior to the positive-contrast liquid enema, and since its introduction, the air enema has had increasing acceptance among pediatric radiologists; in 2004, 65% of pediatric radiologists in the United States reported using air enema, a proportion that is likely higher today.34 An air enema is considered superior for several reasons. It is cleaner, because no liquid or stool spillage occurs on the table, on the patient, or on the field of view. It is much easier to see the progress of the reduction through the distended sigmoid when it is filled with gas than when it is filled with dense positive-contrast media. An air enema is also considered safer than a liquid enema because if perforation does occur, it has been shown that there is less spillage of fecal material and liquid into the peritoneal cavity. Reduction usually is achieved more quickly, and air is less dense than positive-contrast media, translating into less radiation exposure. The rates of recurrence of intussusception after air or after liquid enema reductions do not differ; both are approximately 10%.11,15,35–37
In more than 70 published studies of enema reduction, investigators report an average reduction rate of 76% (Table 108-2).8,38 When the reduction rates are weighted by the number of children in each study, the average reduction rate for air is significantly better than for liquid (82% for air and 73% for liquid). In the largest published series, Gu and colleagues36 used air enema in 9028 children and reported reduction rates of 95%. However, although the air enema may be preferred in experienced hands, the liquid enema is also effective. In two randomized, controlled trials of reduction rate or air versus liquid enema, one trial concluded that air enema was superior to liquid enema,39 and the other showed no difference,40 although the sample size was small.
Table 108-2
Summary of Published Studies* of Enema Reduction and Perforation Rates†
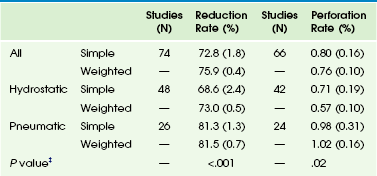
*Excludes two very large studies by Guo et al. (1986) and Zhang et al. (1986).
†All values are mean (standard error) from unweighted (simple) and weighted estimates. Weighted estimates use the sample size to adjust the reported mean reduction and perforation rates.
‡p-values based on logistic regression. Compare hydrostatic with pneumatic rate and perforation rate.
Reprinted with permission from Applegate KE. Intussusception in children: diagnostic imaging and treatment. In: Medina LS, Applegate KE, Blackmore CC, eds. Evidence-based imaging in pediatrics. New York: Springer; 2010.
Air Enema Technique
To perform the air enema technique, the enema tip should be placed in the child’s rectum and taped in place. The tape can be shaped into a funnel along the tube to help form a seal. The buttocks are taped together tightly, and an assistant should hold the buttocks closed, whether the child is in a supine or a prone position. This technique is important because air leaking around the tube diminishes the pressure head. Air is rapidly insufflated into the colon under fluoroscopic observation, up to a constant mean pressure of 120 mm Hg, thus maximizing reduction and minimizing the risk for perforation. Once the intussusception is encountered, it is monitored fluoroscopically until it is completely reduced. The use of pulsed fluoroscopy at a low frame rate is an important factor for reducing the radiation dose, particularly when the reduction is lengthy. Fluoroscopy “grabs” (or “last image hold”) can document the progress of the reduction, without additional exposures. Air should flow freely from the cecum into the distal small bowel loops to signify complete reduction (Fig. 108-8; Video 108-1).
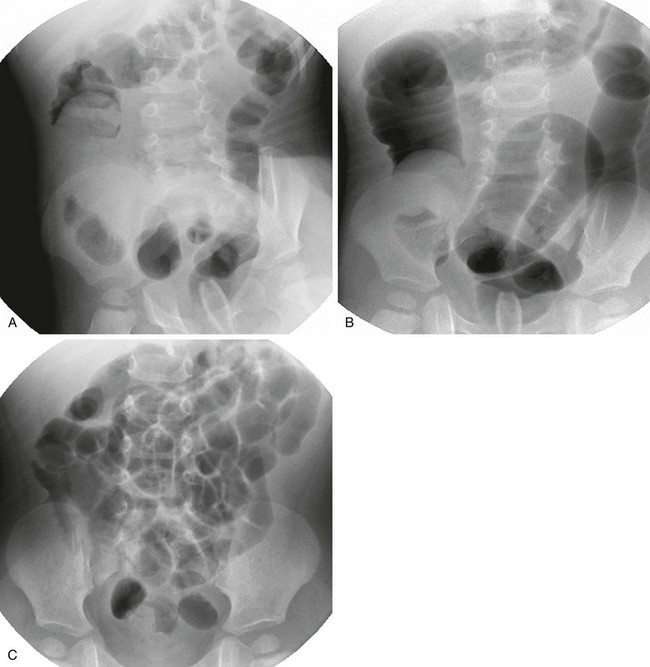
Figure 108-8 Pneumatic reduction of intussusception.
A, An initial fluoroscopic image shows the tube tip in the rectum and the leading edge of the intussusception at the hepatic flexure. B, After continued insufflation and further distension of the colon, the leading edge has moved into the right lower quadrant. C, After successful reduction, gas fills multiple loops of small bowel. (Courtesy Dr. Marta Hernanz-Schulman, Nashville, TN.)
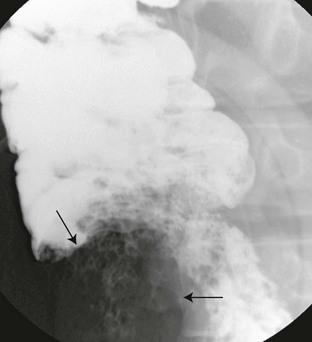
A positive-contrast liquid enema tends to outline the small bowel loops to better advantage and may outline the appendix at the cecal tip (e-Fig. 108-9). Ileoileal components may be more conspicuously identified. Rarely, the appendix intussuscepts into the cecum, causing abdominal pain (e-Fig. 108-10). A general guideline to the liquid enema technique is the “rule of 3s”: three attempts of 3 minutes’ duration, with the liquid enema bag at 3 feet above the fluoroscopy table (see Box 108-2). Although little evidence exists to support this rule, particularly regarding the height of the enema bag,8,41 it serves well as a general guideline. A study by Kuta and Benator42 of the pressures generated by a column of liquid media indicates that media differ in the height at which a pressure of 120 mm Hg is generated. This differs from the air enema technique, which allows control and documentation of the pressure used. The examination is tailored to the patient and performed in collaboration with the surgeon.
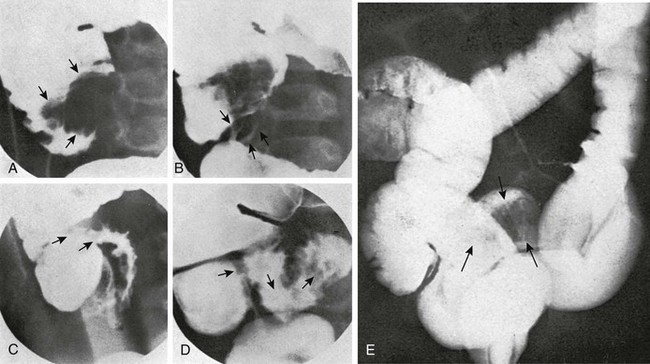
e-Figure 108-9 Hydrostatic reduction.
Serial radiographic changes at the ileocecal valve during hydrostatic reduction of intussusception in an 18-month-old infant. A, The intussusception has moved proximally from the transverse colon into the cecum, where it causes a filling defect (arrows). B, The appendix is beginning to fill (arrows), and the cecal filling defect is smaller. C, The terminal ileum is beginning to fill (arrows), and the cecal filling defect has disappeared. D, The terminal ileum is normally dilated (arrows), with normal mucosal relief. E, In another child, residual ileoileal intussusception (arrows) in the terminal ileum after hydrostatic reduction of the colic component of an ileoileocolic intussusception. The leading edge initially was encountered at splenic flexure.
Radiation Exposure
The radiation exposure a child receives depends on a number of factors, including the type of fluoroscopy equipment, the use of pulsed fluoroscopy, the ease or rapidity of reduction, the fluoroscopy time, and the contrast medium used. Experienced pediatric radiologists performing an air enema average approximately 95 seconds of fluoroscopy time to reduce an intussusception.36 Air enema radiation exposures have been calculated to be less than one third those given during a barium enema.43 In 2003, Henrikson and coworkers26 estimated that the mean radiation exposure was 25 mSv for enema reductions in a group of patients receiving both air and positive-contrast media reductions.
Perforation
The potential complication of enema reduction that causes the most concern is bowel perforation.11,44,45 The risk for perforation depends on each radiologist’s patient population and technique. Although determination of clinical predictors of perforation is complicated by a lack of prospective studies, a key factor is symptoms that last longer than 48 hours. Several reports of studies in porcine models and in children suggest that a preexisting focal perforation in the necrotic intussuscipiens or less commonly the intussusceptum, may exist that is rarely radiographically apparent as free air before reduction but is uncovered during the reduction process.8,11,15,44–46 The most common site is at or just proximal to the intussusception in the transverse colon.
In a summary of more than 60 studies, the mean perforation rate is less than 1%39 (see Table 108-2). In 1989, Campbell47 surveyed enema techniques and complications of North American pediatric radiologists. Respondents’ combined experience was 14,000 intussusception enemas. Although they did not report enema reduction rates, the combined perforation rate was 0.39% (55 per 14,000, or 1 per 250 to 300 patients), with only one death. This study remains the basis for the perforation risk when it is explained to parents prior to enema reduction.47
Barium is no longer the liquid contrast medium of choice for reduction of intussusception among most pediatric radiologists because of the risks for barium peritonitis, infection, and adhesions when perforation occurs during the enema. If liquid media are to be used, iodinated contrast material is now preferred and is considered a safer agent than barium; nevertheless, such media are hypertonic and may produce fluid and electrolyte shifts if perforation occurs.11,46,48–50
Alternative Enema Approaches
A number of different approaches have been described to try to improve intussusception reduction via enema. These approaches include sedation, anesthesia, use of glucagon, manual palpation, and a delayed repeat enema. Except for the delayed repeat enema, none of these approaches has been proved to increase the rate of successful reduction. Sedation may reduce the intraabdominal pressure children create by the Valsalva maneuver, a factor that increases success of reduction and decreases the perforation rate.8,35
Fluoroscopy Versus Sonography
In North American and most European centers, fluoroscopy is almost always used during enema reduction. In Asian and some European centers, sonographic guidance is used, thus avoiding any radiation exposure. Reports on the use of sonography with water or other liquid media such as normal saline solution show rates of successful reduction to be as high or higher than with fluoroscopic techniques.51,52 However, the experience level required for these techniques has not been evaluated.
Delayed Repeat Enema
When an initial enema reduction attempt fails to completely reduce the intussusception, a delayed repeat enema may be successful and thus avoid the need for surgical reduction. The use of such an additional, delayed attempt between 30 minutes and 19 hours after the initial procedure has shown promise in increasing the success of enema reductions. Four studies report further reduction in 50% to 82% of cases in which reduction fails at the initial enema.53–55 Further research to understand optimal timing and technique for delayed repeat enemas is needed. The largest reported experience to date suggests a delay of 2 to 4 hours, until further research yields more rigorous guidelines.8 The child must remain clinically stable and be appropriately monitored during this time interval. A delayed enema is useful when movement of the intussusception occurred at the initial attempt, but the final reduction could not be accomplished; a delayed enema should not be attempted if the intussusception is not partially reduced during the initial attempt.
Surgical Management and Complications
The costs of surgical care are four to five times the costs of nonsurgical management.33,56 Depending on the patient population, approximately 20% to 40% of children for whom nonsurgical treatment fails and who undergo surgical reduction of their intussusception will require bowel resection.57
Management of Recurrent Cases
In patients with recurrent intussusception, including multiple recurrences, enema remains the preferred method of reduction. Intussusception recurrence rates average up to 10% in large series (range, 5% to 15%), regardless of whether the reduction technique involved an air or liquid enema. The recurrence rates are less than or equal to 5% when surgical reduction is performed, presumably because of the development of adhesions.58 Enema reduction is both safe and effective in cases of recurrent intussusception, as long as the child remains clinically stable. Approximately 50% of children in whom recurrent intussusception develops present within 48 hours, although recurrences have been reported up to 18 months later. No clear risk factors have been discovered to explain why some children have recurrences, although some children have focal pathologic lead points. Nevertheless, the risk for lead points in children with recurrent intussusception remains low. In a large series of 763 children reported by Daneman and colleagues,46 lead points were present in only 8% of recurrent intussusceptions, only slightly higher than the 5% to 6% incidence of lead points at first presentation of intussusceptions.
When the presence of pathologic lead points is a concern, ultrasound may play an important role, detecting as many as 60% of the lead points (see Fig. 108-6).4,5 Although ultrasound does not detect all lead points, the risk of missing a lead point without other signs or symptoms to guide management is thought to be unlikely.5,58 To test the hypothesis that recurrent intussusception in some patients might be related to lymphoid hyperplasia at the terminal ileum, Lin and colleagues3 conducted a randomized, double-blind trial comparing 144 children who received intramuscular corticosteroid drugs with 137 children who received placebo before air enema reduction. No recurrences occurred in the children who received dexamethasone, compared with a 5% recurrence rate in the placebo group. These investigators hypothesized that steroids decreased the volume of mesenteric adenopathy and lymphoid hyperplasia in the terminal ileum and thus decreased the risk for recurrence.3 However, further investigation is needed for confirmation and to evaluate the risks and benefits of this intervention.
Applegate, KE. Clinically suspected intussusception in children: evidence-based review and self-assessment module. AJR Am J Roentgenol. 2005;185(suppl 3):S175–S183.
Daneman, A, Navarro, O. Intussusception. Part 1: A review of diagnostic approaches. Pediatr Radiol. 2003;33:79–85.
Daneman, A, Navarro, O. Intussusception. Part 2: An update on the evolution of management. Pediatr Radiol. 2004;34:97–108.
Navarro, O, Daneman, A. Intussusception. Part 3: Diagnosis and management of those with an identifiable or predisposing cause and those that reduce spontaneously. Pediatr Radiol. 2004;34:305–312.
References
1. Parashar, UD, et al. Trends in intussusception-associated hospitalizations and deaths among US infants. Pediatrics. 2000;106(6):1413–1421.
2. Strouse, PJ, DiPietro, MA, Saez, F. Transient small-bowel intussusception in children on CT. Pediatr Radiol. 2003;33(5):316–320.
3. Lin, SL, Kong, MS, Houng, DS. Decreasing early recurrence rate of acute intussusception by the use of dexamethasone. Eur J Pediatr. 2000;159(7):551–552.
4. Navarro, O, Daneman, A. Intussusception. Part 3: Diagnosis and management of those with an identifiable or predisposing cause and those that reduce spontaneously. Pediatr Radiol. 2004;34(4):305–312. [quiz 369].
5. Ein, SH. Leading points in childhood intussusception. J Pediatr Surg. 1976;11(2):209–211.
6. Rennels, MB, et al. Lack of an apparent association between intussusception and wild or vaccine rotavirus infection. Pediatr Infect Dis J. 1998;17(10):924–925.
7. Desai, R, et al. Potential intussusception risk versus health benefits from rotavirus vaccination in Latin America. Clin Infect Dis. 2012;54(10):1397–1405.
8. Daneman, A, Navarro, O. Intussusception. Part 2: An update on the evolution of management. Pediatr Radiol. 2004;34(2):97–108. [quiz 187].
9. Daneman, A, Navarro, O. Intussusception. Part 1: a review of diagnostic approaches. Pediatr Radiol. 2003;33(2):79–85.
10. Losek, JD, Fiete, RL. Intussusception and the diagnostic value of testing stool for occult blood. Am J Emerg Med. 1991;9(1):1–3.
11. Shiels, WE, 2nd., et al. John Caffey Award. Colonic perforation by air and liquid enemas: comparison study in young pigs. AJR Am J Roentgenol. 1993;160(5):931–935.
12. Harrington, L, et al. Ultrasonographic and clinical predictors of intussusception. J Pediatr. 1998;132(5):836–839.
13. Klein, EJ, Kapoor, D, Shugerman, RP. The diagnosis of intussusception. Clin Pediatr (Phila). 2004;43(4):343–347.
14. Kuppermann, N, et al. Predictors of intussusception in young children. Arch Pediatr Adolesc Med. 2000;154(3):250–255.
15. Beasley, S. Intussusception. Pediatr Radiol. 2004;34(4):302–304.
16. Sargent, MA, Babyn, P, Alton, DJ. Plain abdominal radiography in suspected intussusception: a reassessment. Pediatr Radiol. 1994;24(1):17–20.
17. West, KW, et al. Intussusception: current management in infants and children. Surgery. 1987;102(4):704–710.
18. Littlewood Teele, R, Vogel, SA. Intussusception: the paediatric radiologist’s perspective. Pediatr Surg Int. 1998;14(3):158–162.
19. Kornecki, A, et al. Spontaneous reduction of intussusception: clinical spectrum, management and outcome. Pediatr Radiol. 2000;30(1):58–63.
20. Eklof, O, Hartelius, H. Reliability of the abdominal plain film diagnosis in pediatric patients with suspected intussusception. Pediatr Radiol. 1980;9(4):199–206.
21. Hooker, RL, et al. Radiographic evaluation of intussusception: utility of left-side-down decubitus view. Radiology. 2008;248(3):987–994.
22. Pracros, JP, et al. Acute intestinal intussusception in children. Contribution of ultrasonography (145 cases). Ann Radiol (Paris). 1987;30(7):525–530.
23. Verschelden, P, et al. Intussusception in children: reliability of US in diagnosis—a prospective study. Radiology. 1992;184(3):741–744.
24. Schmit, P, Rohrschneider, WK, Christmann, D. Intestinal intussusception survey about diagnostic and nonsurgical therapeutic procedures. Pediatr Radiol. 1999;29(10):752–761.
25. del-Pozo, G, et al. Intussusception: trapped peritoneal fluid detected with US—relationship to reducibility and ischemia. Radiology. 1996;201(2):379–383.
26. Henrikson, S, et al. The effect of screening sonography on the positive rate of enemas for intussusception. Pediatr Radiol. 2003;33(3):190–193.
27. Swischuk, LE, Hayden, CK, Boulden, T. Intussusception: indications for ultrasonography and an explanation of the doughnut and pseudokidney signs. Pediatr Radiol. 1985;15(6):388–391.
28. del-Pozo, G, et al. Intussusception in children: current concepts in diagnosis and enema reduction. Radiographics. 1999;19(2):299–319.
29. Shanbhogue, RL, et al. Ultrasonography is accurate enough for the diagnosis of intussusception. J Pediatr Surg. 1994;29(2):324–327. [discussion 327-328].
30. Lim, HK, et al. Assessment of reducibility of ileocolic intussusception in children: usefulness of color Doppler sonography. Radiology. 1994;191(3):781–785.
31. Britton, I, Wilkinson, AG. Ultrasound features of intussusception predicting outcome of air enema. Pediatr Radiol. 1999;29(9):705–710.
32. Navarro, O, et al. The impact of imaging in the management of intussusception owing to pathologic lead points in children. A review of 43 cases. Pediatr Radiol. 2000;30(9):594–603.
33. Bratton, SL, et al. Intussusception: hospital size and risk of surgery. Pediatrics. 2001;107(2):299–303.
34. Daneman A: Unpublished survey, Savannah, GA, Society for Pediatric Radiology Annual Meeting, May 2004.
35. Shiels, WE, 2nd., et al. Air enema for diagnosis and reduction of intussusception: clinical experience and pressure correlates. Radiology. 1991;181(1):169–172.
36. Gu, L, et al. John Caffey Award. Intussusception reduction in children by rectal insufflation of air. AJR Am J Roentgenol. 1988;150(6):1345–1348.
37. Guo, JZ, Ma, XY, Zhou, QH. Results of air pressure enema reduction of intussusception: 6,396 cases in 13 years. J Pediatr Surg. 1986;21(12):1201–1203.
38. Applegate, KE. Intussusception in children: diagnostic imaging and treatment. In: Medina LS, Applegate KE, Blackmore CC, eds. Evidence-based imaging in pediatrics. New York: Springer, 2010.
39. Hadidi, AT, El Shal, N. Childhood intussusception: a comparative study of nonsurgical management. J Pediatr Surg. 1999;34(2):304–307.
40. Meyer, JS, et al. Air and liquid contrast agents in the management of intussusception: a controlled, randomized trial. Radiology. 1993;188(2):507–511.
41. McAlister, WH. Intussusception: even Hippocrates did not standardize his technique of enema reduction. Radiology. 1998;206(3):595–598.
42. Kuta, AJ, Benator, RM. Intussusception: hydrostatic pressure equivalents for barium and meglumine sodium diatrizoate. Radiology. 1990;175(1):125–126.
43. Phelan, E, de Campo, JF, Malecky, G. Comparison of oxygen and barium reduction of ileocolic intussusception. AJR Am J Roentgenol. 1988;150(6):1349–1352.
44. Armstrong, EA, et al. Intussusception complicated by distal perforation of the colon. Radiology. 1980;136(1):77–81.
45. Mercer, S, Carpenter, B. Mechanism of perforation occurring in the intussuscipiens during hydrostatic reduction of intussusception. Can J Surg. 1982;25(5):481–483.
46. Daneman, A, et al. Patterns of recurrence of intussusception in children: a 17-year review. Pediatr Radiol. 1998;28(12):913–919.
47. Campbell, JB. Contrast media in intussusception. Pediatr Radiol. 1989;19(5):293–296.
48. Kirks, DR. Diagnosis and treatment of pediatric intussusception: how far should we push our radiologic techniques? Radiology. 1994;191(3):622–623.
49. Hernanz-Schulman, M, et al. Experimental study of mortality and morbidity of contrast media and standardized fecal dose in the peritoneal cavity. Pediatr Radiol. 2000;30(6):369–378.
50. Hernanz-Schulman, M, et al. Effect of radiographic contrast agents on leukocyte metabolic response. Pediatr Radiol. 2000;30(6):361–368.
51. Wang, GD, Liu, SJ. Enema reduction of intussusception by hydrostatic pressure under ultrasound guidance: a report of 377 cases. J Pediatr Surg. 1988;23(9):814–818.
52. Gu, L, et al. Sonographic guidance of air enema for intussusception reduction in children. Pediatr Radiol. 2000;30(5):339–342.
53. Gorenstein, A, et al. Intussusception in children: reduction with repeated, delayed air enema. Radiology. 1998;206(3):721–724.
54. Saxton, V, et al. Intussusception: a repeat delayed gas enema increases the nonoperative reduction rate. J Pediatr Surg. 1994;29(5):588–589.
55. Sandler, AD, et al. Unsuccessful air-enema reduction of intussusception: is a second attempt worthwhile? Pediatr Surg Int. 1999;15(3-4):214–216.
56. Stein, JE, Beasley, SW, Phelan, E. The cost benefit of changing protocols in the management of intussusception. Aust N Z J Surg. 1997;67(6):330–331.
57. Kaiser, AD, Applegate, KE, Ladd, AP. Current success in the treatment of intussusception in children. Surgery. 2007;142(4):469–475. [discussion 475-477].
58. Ein, SH. Recurrent intussusception in children. J Pediatr Surg. 1975;10(5):751–755.