Introduction to radiological interpretation
• To identify the presence or absence of disease
• To provide information on the nature and extent of the disease
To achieve these objectives and maximize the diagnostic yield, interpretation should be carried out under specified conditions, following ordered, systematic guidelines.
Essential requirements for interpretation
The essential requirements for interpreting dental radiographs can be summarized as follows:
• Understanding the nature and limitations of the black, white and grey radiographic image
• Knowledge of what the radiographs used in dentistry should look like, so a critical assessment of individual image quality can be made
• Detailed knowledge of the range of radiographic appearances of normal anatomical structures
• Detailed knowledge of the radiographic appearances of the pathological conditions affecting the head and neck
• A systematic approach to viewing the entire radiograph and to viewing and describing specific lesions
Optimum viewing conditions
For film-captured images these include:
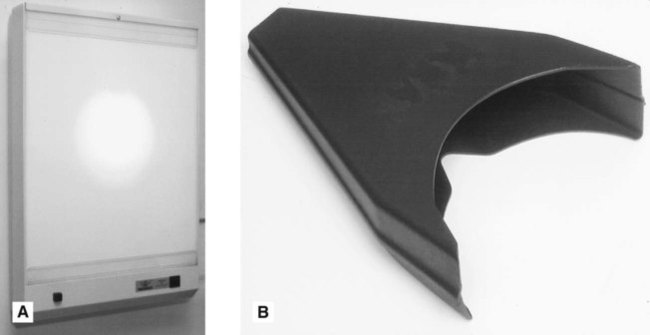
• An even, uniform, bright light viewing screen (preferably of variable intensity to allow viewing of films of different densities) (see Fig. 19.1)
• A quiet, darkened viewing room
• The area around the radiograph should be masked by a dark surround so that light passes only through the film
• Use of a magnifying glass to allow fine detail to be seen more clearly on intraoral films
These ideal viewing conditions give the observer the best chance of perceiving all the detail contained within the radiographic image. With many simultaneous external stimuli, such as extraneous light and inadequate viewing conditions, the amount of information obtained from the radiograph is reduced. Film-captured radiographs should be viewed once they have dried as films still wet from processing may show some distortion of the image.
Digital images should be viewed on bright, high-resolution monitors in subdued lighting (see Fig. 19.2). Table 19.1 outlines the minimum and ideal specifications of the monitor (image display device) as recommended in the UK by the Health Protection Agency and by the Royal College of Radiologists.
Table 19.1
Summary of the minimum and ideal specifications for the monitor when viewing digital images
| Minimum specification | Ideal specification | |
| Screen resolution | ≥1280 × 1024 (~1.3 megapixels) | ≥1500 × 2000 |
| Screen size (viewable diagonal) | ≥42cm (~17″) | ≥50cm (~20″) |
| Maximum luminance | >170 cd/m2 | ≥500cd/m2 |
| Luminance contrast ratio | ≥250 : 1 | ≥500 : 1 |
| Greyscale bit depth | 8-bit greyscale (24-bit colour) | ≥10-bit greyscale |
The nature and limitations of different radiographic images
The importance of understanding the nature of different types of radiographic images – film-captured or digital (depending on the type of image receptor used) and their specific limitations was explained in Chapter 1. How the visual images are created by processing – chemical or computer – was explained in Chapter 5. Revision of both of these chapters is recommended. To reiterate, the final image whether captured on film or digitally is ‘a two-dimensional picture of three-dimensional structures superimposed on one another and represented as a variety of black, white and grey shadows’ – a shadowgraph.
Critical assessment of image quality
1. WHY each projection was taken
2. HOW the projections were taken using different image receptors
Film-captured images
The practical factors that can influence film quality were discussed in Chapter 17, and included:
A critical assessment of radiographs can be made by combining these factors and by asking a series of questions about the final image. These questions relate to:
Here are some typical examples.
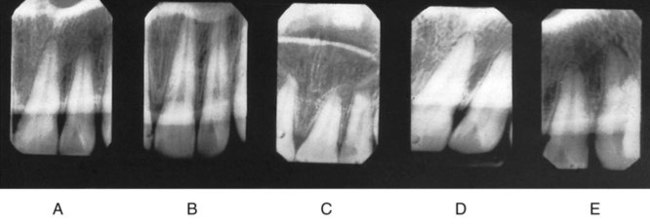
Radiographic Technique (see Fig. 19.3)
• Which technique has been used?
• How were the patient, film and X-ray tubehead positioned?
• Is this a good example of this particular radiographic projection?
• How much distortion is present?
• Is the image foreshortened or elongated?
• Is there any rotation or asymmetry?
• How good are the image resolution and sharpness?
• Which artefactual shadows are present?
• How do these technique variables alter the final radiographic image?
Digitally captured images
The practical factors that can affect digitally captured images, how the images are created and how they can be altered using computer software were discussed in Chapter 5 and included:
• The image receptor – solid-state or photo-stimulable phosphor plate
As with film-captured images a critical assessment of digital images can be made by combining these factors and by asking a series of questions about the final image. These questions relate to:
Radiographic Technique
• Which technique has been used?
• How were the patient, digital receptor and X-ray tubehead positioned?
• Is this a good example of this particular radiographic projection?
• How much distortion is present?
• Has the whole area of interest been included?
• Is the image foreshortened or elongated?
• Is there any rotation or asymmetry?
• How good are the image resolution and sharpness?
• Which artefactual shadows are present?
• How do these technique variables alter the final radiographic image?
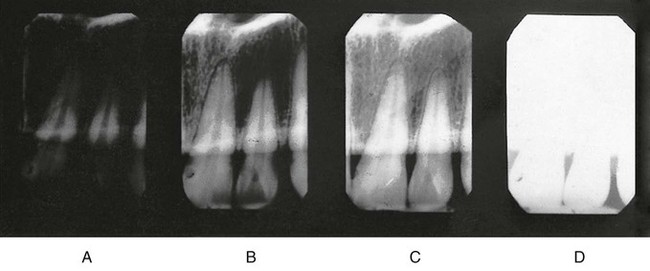
Image processing
With experience, this critical assessment of image quality is not a lengthy procedure but it is never one that should be overlooked. A poor radiographic image is a poor diagnostic aid and sometimes may be of no diagnostic value at all. Clinicians used to using film-captured images who decide to ‘go digital’ should take time to understand the nature of the digital image, the effect on the image of using powerful computer software manipulation and the importance of viewing digital images on high resolution, calibrated monitors.
Detailed knowledge of normal anatomy
• The type of radiograph being interpreted (e.g. conventional radiograph or tomograph)
• The position of the patient, image receptor and X-ray tubehead.
Only with all this information can clinicians appreciate how the various normal anatomical structures, through which the X-ray beam has passed, will appear on any particular radiograph.
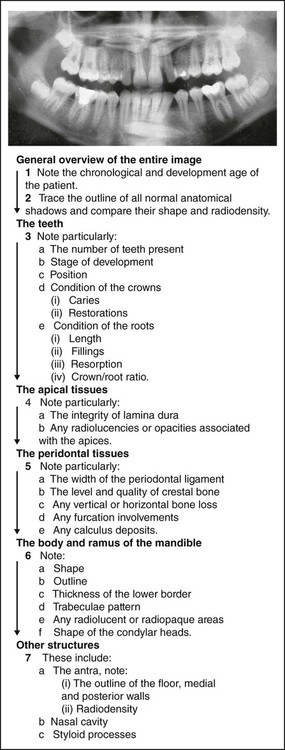
Systematic approach
The entire radiograph
Any systematic approach will suffice as long as it is logical, ordered and thorough. Several suggested sequences are described in later chapters. By way of an example, a suggested systematic approach to the overall interpretation of panoramic radiographs (see Ch. 15) is shown in Fig. 19.5.
Specific lesions
A systematic description of a lesion should include its:
Making a radiological differential diagnosis depends on this systematic approach. It is described in detail and expanded on later (see Ch. 25).