INTRODUCTION
What is respiration?
The ‘bottom line’ of an account of the complicated process of respiration begins with a flow of
The need for respiration
One definition of the success of a species of organism, in evolutionary terms, is how well it can maintain constant the composition of the fluid surrounding its individual cells (its internal environment) despite changes in its external environment (surroundings getting dryer, colder, warmer etc.). This process is called homeostasis and requires energy. Most of the energy generated by our tissues is the result of oxidation of food substrates, and this is the reason we need a flow of OXYGEN IN. Neophytes in physiology often emphasize the role of the respiratory system in providing this oxygen, and certainly an uninterrupted supply is important, particularly for the nervous system, but of more immediate importance is the removal of CO2. The word oxygen means ‘acid producer’ (Greek, oxy; acid; gen, to produce), and the major product of our oxidative metabolism is the acid gas CO2. The accumulation of CO2 would result in acidification of the body fluids. The importance of removing this CO2 can be demonstrated by rebreathing from a plastic bag for a few minutes. The unpleasant sensation that forces you to stop this rather dangerous experiment is due to over stimulation of the reflex that controls breathing to get rid of this gas. You will see later (Chapter 8) that CO2 produces its acidic effect by reacting with water to form carbonic acid.
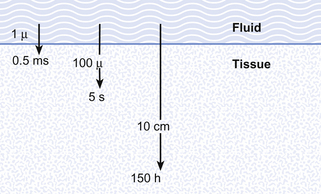
Diffusion in respiration and the circulation
Although in human beings the same passive mechanism of diffusion alone supplies and removes these gases from our bodies (there is no active chemical transport), the phenomenon of diffusion is maximized by complicated respiratory and circulatory systems which accomplish what the pond water does for the amoebae in providing a supply of and a sink for these gases. The lungs promote diffusion by having an enormous surface area, which is very thin, through which diffusion can take place easily. A surface of over 90 m2 is enclosed in a lung volume of less than 10 L. This functional 90 m2 is often reduced in disease, by thickening of the membrane, excess fluid in the lungs, or by a reduction in the supply of air or blood. The circulation of the blood forms the transport link between the diffusion site of the lungs and the diffusion site of the capillaries within the tissues. The distances involved in this link are enormous in molecular terms, and diffusion would be totally useless to transport gas over the metre or so between the lungs and distal tissues of our bodies. This transport is accomplished in seconds by the circulation (Fig. 1.1).
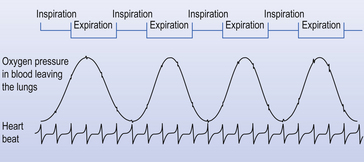
Timing in the circulation and respiration
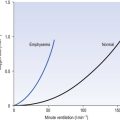
The processes of breathing and the beating of the heart are both cyclic events. One involves the inhalation of air and then its exhalation; the other involves filling of the heart with blood and then its ejection into the circulation. The time courses of these two cycles are very different: at rest you may take 12 breaths in the minute the heart beats 60 times, ejecting 5 L of blood through the lungs (see Fig. 1.2).
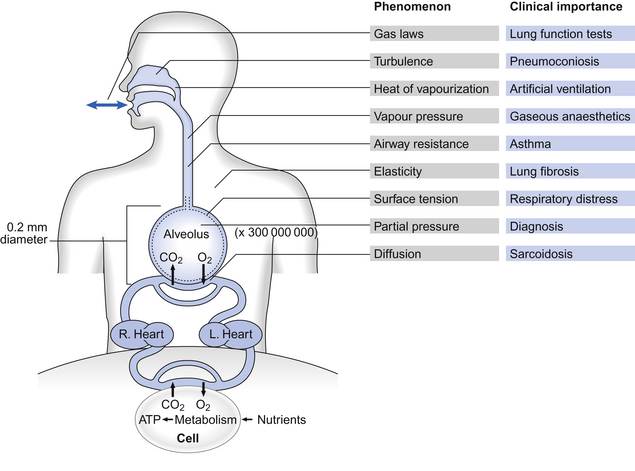
Basic science of respiration
All these changes, just like all the events in respiration, are properly described in terms of the basic sciences physics and chemistry. These are generally not the favourite subjects of students of the basic medical sciences. We have therefore included at the end of the book a short section (Appendix) on the most relevant parts of physics and chemistry that a student should understand in order to understand respiration. That section is not obligatory to students confident with these subjects. The Appendix, which is intended to aid not torment, will repay scrutiny by students who have any doubts about their grasp of basic science. That this basic science is integral to understanding normal respiration and diseased states is illustrated when we take an overview of human respiration and point out where the phenomena we describe apply (Fig. 1.3).
These examples of the importance of the basic sciences in understanding the respiratory system do not mean that a great deal, or a great depth, of knowledge is required. The Appendix contains all that is required to understand the contents of this book. However, there is a vocabulary that is specific to the respiratory system, and it is probably helpful for you to be introduced to it here.
Respiratory symbols – the language of the respiratory system
Primary units are given in capital letters (see Table 1.1):
Table 1.1
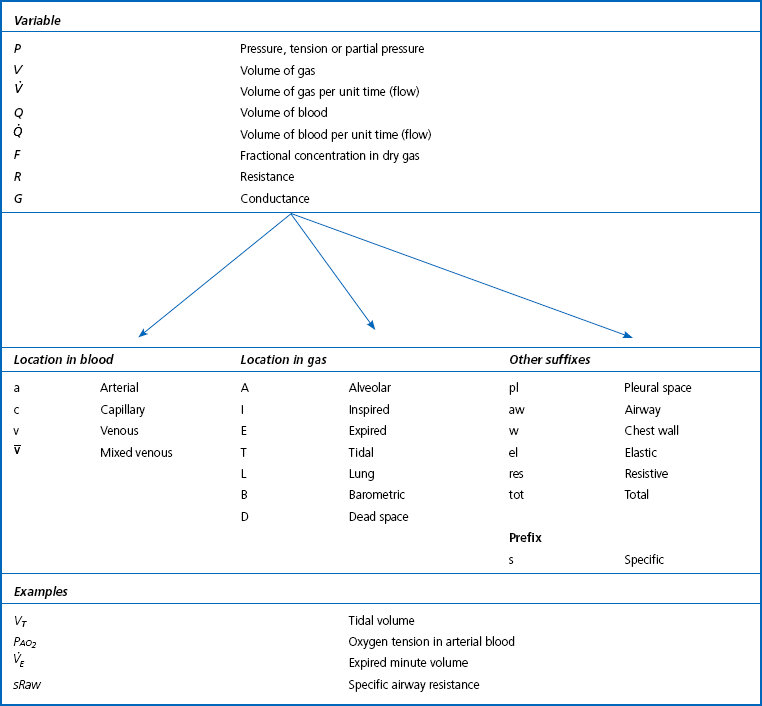
Locations in the gas phase are also given capital letters but smaller than the primary units:
Locations in blood are identified by lower-case letters:
The primary symbol is written first, followed by the qualifying symbol at a lower level.
Drugs
Drugs are chemicals which change the natural functions of the body. Most prescribed drugs have therapeutic properties. Just as Fig. 1.3 demonstrates where specific physical phenomena have particular importance in the respiratory system, Table 1.2 gives examples of conditions where specific types of drugs are used therapeutically in treatment of specific conditions or for specific procedures.
Table 1.2
Drugs and the respiratory system
| Drug name | Type | Condition treated |
| Oxymetazoline | α-agonist | Nasal congestion |
| Atropine | Muscarinic cholinergic antagonist | Excess mucus secretion |
| Prednisolone | Corticosteroid | Allergic rhinitis |
| Chlorpheniramine | Antihistamine | Rhinorrhea |
| Succinylcholine | Neuromuscular blocking | Facilitate tracheal intubation |
| Dextromethorphan | Synthetic narcotic analgesic | Non-productive cough (suppression) |
| Salbutamol (Isoproterenol, USA) | β2 agonist (bronchodilator) | Asthma |
| Cromoglicate | Inflammatory-cell stabilizer | Asthma |
| Beclometasone | Anti-inflammatory corticosteroid | Asthma |
| Azathioprine | Cytotoxic immunosuppressant | Diffuse connective tissue |
| Aminopenicillin etc. | Antibiotic | Pneumonia and other infections |
| Amphotericin B | Antifungal | Fungal infections |