CHAPTER 30 Intrasellar and Diaphragma Sellae Meningiomas 
INTRODUCTION
The first report of an intrasellar meningioma originating from the diaphragma sellae was published by Hardy and Robert in 1969;1 Cushing and Eisenhardt were the first to classify sellar and parasellar meningiomas.2 The suprasellar meningiomas as described by Cushing were further subdivided by Jefferson into diaphragma sella meningioma, tuberculum meningioma, and meningioma of the clinoid processes.3 Subsequently, Osama Al-Mefty proposed that diaphragma sellae meningioma had a clinical syndrome distinct from tuberculum sellae meningioma. He went on to classify the diaphragma sellae meningiomas into two supradiaphragmatic suprasellar types and one infradiaphragmatic intrasellar type.4 Diaphragma sellae meningiomas are rare, and intrasellar meningiomas originating from the dura of the sella turcica are even less commonly encountered.
REGIONAL ANATOMY
The surface area of the dura mater of the sella turcica is estimated to be greater than 6 cm2.5,6 Meningiomas can originate from the diaphragma sellae as well as any part of the dura mater of the sella turcica. Subdiaphragmatic intrasellar meningiomas are quite rare and only 18 operatively confirmed cases have been reported in the literature.6 The origins of 9 of the 18 reported cases of intrasellar meningiomas have been described. These include six meningiomas originating from the lower leaf of the diaphragma sellae, two from the floor of the sella turcica, and one from the anterior wall of the sella turcica.6 Meningiomas arising from the diaphragma sellae and the sellar dura must be distinguished from those arising from adjacent structures such as the planum sphenoidale, the tuberculum sellae, medial sphenoid wing, and cavernous sinus. In contrast to tuberculum sellae meningiomas that are most often fed by the posterior ethmoid arteries, diaphragma sellae meningiomas are supplied by branches of the internal carotid arteries. Intrasellar meningiomas are supplied by the dural branches of the external carotid artery, and branches of the internal maxillary artery as well as the internal carotid artery.6
CLASSIFICATION
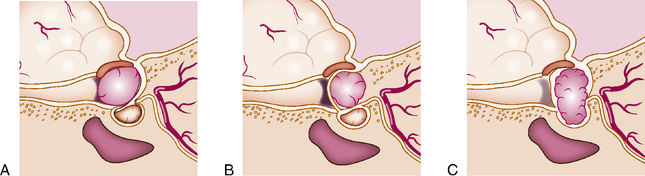
Al-Mefty and Ciric classified diaphragma sellae meningiomas into three types according to their site of origin4 (Fig. 30-1). Type A originates from the upper leaf of the diaphragma sellae anterior to the pituitary stalk. Type B arises from the upper leaf of the diaphragma sellae posterior to the pituitary stalk. Type C originates from the inferior leaf of the diaphragma sellae. Type A and B tumors are largely suprasellar, while type C diaphragma sellae meningiomas are largely intrasellar. Similar to type C, subdiaphragmatic meningiomas arising from the dura of the sella turcica are mostly intrasellar.
DIFFERENTIAL DIAGNOSIS
Pituitary adenoma; meningioma arising from adjacent structures such as the tuberculum, medial sphenoid wing, and cavernous sinus; craniopharyngioma; hemangiopericytoma; and metastasis should be considered in the differential diagnosis when evaluating patients with suspected diaphragma sellae or intrasellar meningiomas.7,8
CLINICAL FEATURES
Patients with diaphragma sellae and intrasellar meningiomas most commonly present with visual disturbance, visual field deficit, endocrine abnormalities, and headache. Al-Mefty and Ciric reported clinical symptoms and deficits in a series of 12 patients, 9 of whom had visual disturbance, 7 had visual field defects, 9 had headaches, and 2 had diabetes insipidus.4 The distinct clinical features of type A, B, and C diaphragma sellae meningiomas are presented in the text that follows.
DIAGNOSTIC IMAGING
Various imaging modalities can be utilized to evaluate sellar and parasellar lesions. Plain radiographs can show calcification as well as enlargement of the sella turcica. Computed tomography (CT) most often reveals a homogeneously enhancing intrasellar, suprasellar, or intra- and suprasellar mass. Magnetic resonance imaging (MRI) is better able to delineate anatomic details that can help establish the origin of a meningioma. A sella protocol MRI with contrast that includes thin cut axial, coronal, and sagittal sections through the sella is the best imaging modality for assessing intrasellar and suprasellar meningiomas. MRI characteristics include homogeneous and intense enhancement of the tumor. A dural tail and a displaced normal pituitary gland can sometimes be appreciated. Intrasellar meningioma is difficult to distinguish radiographically from pituitary adenoma.9 Similarly, at times diaphragma sellae meningioma cannot be differentiated from tuberculum sellae meningioma on preoperative diagnostic imaging. Finally, cerebral angiography may sometimes be useful in identifying the nature and origin of the tumor. Cerebral angiography often demonstrates a marked tumor blush in patients with sellar and parasellar meningiomas.6 Preoperative embolization of the external carotid feeders can occasionally be considered before proceeding to surgery.
SURGICAL MANAGEMENT
Approach
Type A and B diaphragma sellae meningiomas
Upper leaf diaphragma sellae meningiomas are primarily suprasellar and in most cases involve the optic apparatus. These have traditionally been approached via the transcranial route. Orbitozygomatic, pterional, and subfrontal approaches have been commonly utilized. Classically, the advantages of cranial approaches over the transsphenoidal (TS) approach are thought to be superior visualization of the optic apparatus and anterior cerebral arteries. Disadvantages of cranial approaches include poor visualization of pituitary stalk and the intrasellar component of the tumor, and higher morbidity compared to the transsphenoidal approach. New frontiers in TS surgery are beginning to explore the feasibility of using the extended TS approach for these tumors.10–15 Limited reports on outcomes of patients with suprasellar meningiomas after an extended TS approach have been published; however, these early reports have not differentiated tuberculum sellae meningiomas from diaphragma sellae meningiomas.16
Type C and other intrasellar meningiomas
The majority of meningiomas that are primarily intrasellar can be safely removed through the TS approach. These include tumors that arise from the dura of the hypophyseal fossa and/or the inferior leaf of the diaphragma sellae. The major disadvantage of the TS route is the limited lateral reach of this approach. Hence, tumors with lateral extension may require a combined or sequential TS and transcranial approach. The TS approach does not require brain retraction and hence does not have the morbidity related to this maneuver. Another advantage of TS approach is better visualization of the pituitary stalk. Nonetheless, some surgeons continue to prefer operating on tumors with suprasellar extension through the transcranial approach and give better visualization of the optic apparatus as the primary reason for this preference.4
COMPLICATIONS
The most common complications after resection of diaphragma sellae and intrasellar meningiomas include intraoperative bleeding, visual loss, diabetes insipidus (DI), syndrome of inappropriate secretion of antidiuretic hormone (SIADH), CSF rhinorrhea and hypopituitarism, Kinjo and colleagues4 reported 4 complications in 12 patients who underwent craniotomy for a diaphragma sellae meningioma, one of whom died secondary to a pulmonary embolus. The other complications included transient SIADH, transient DI, and transient Parkinsonism. Massive intraoperative bleeding has occasionally been reported and may be especially problematical with the TS approach.6
Couldwell and colleagues16 described 11 cases of diaphragma/tuberculum sella meningioma approached via the TS route and reported monocular blindness in one patient. Andrews and Wilson have reported worse postoperative visual outcomes in patients with diaphragma sellae meningiomas compared to meningiomas limited to the tuberculum sellae.17 They found postoperative visual deterioration in four of seven patients with diaphragma sellae meningioma treated by craniotomy and no patient in their series with diaphragma sellae meningioma showed postoperative improvement in vision.
PATIENT OUTCOMES
Type A and type B tumors are generally approached via the transcranial route. After review of 11 type A cases, Al-Mefty and Kinjo and colleagues4 reported good results in 10/11 patients. Outcomes of patients with type B tumors were worse than that of patients with type A tumors. Of the eight patients reviewed, only four had good outcomes. Two patients had a fair outcome with permanent DI and hypopituitarism and two patients died. Excessive bleeding was reported in 3 of 10 patients who underwent TS surgery for type C diaphragma sellae meningioma.4 Andrews and Wilson reported complete resection of only two of seven meningiomas involving the diaphragma sella and concluded these tumors are much more difficult to resect completely. Finally, Nozaki and colleagues6 reviewed 18 cases of intrasellar meningioma and reported complete resection in six cases, four via the TS approach and two via transcranial resection. Five cases in this review were reported to have had major intraoperative bleeding.
RADIATION THERAPY
Stereotactic radiosurgery can be utilized for management of residual tumor. Recently, multisession radiosurgery has been shown to safely manage perioptic tumors with minimal risk to the optic apparatus.18
[1] Hardy J., Robert F. A meningioma of the sella turcica, subdiaphragmatic variety. Exeresis through the transsphenoidal route. Neurochirurgie. 1969;15:535-543.
[2] Cushing H., Eisenhardt L. Meningiomas. New York: Hafner, 1969.
[3] Jefferson A., Azzam N. The suprasellar meningiomas: a review of 19 years’ experience. Acta Neurochir Suppl (Wien). 1979;28:381-384.
[4] Kinjo T., Al-Mefty O., Ciric I. Diaphragma sellae meningiomas. Neurosurgery. 1995;36:1082-1092.
[5] Grisoli F., Vincentelli F., Raybaud C., et al. Intrasellar meningioma. Surg Neurol. 1983;20:36-41.
[6] Nozaki K., Nagata I., Yoshida K., Kikuchi H. Intrasellar meningioma: case report and review of the literature. Surg Neurol. 1997;47:447-452. discussion 452–4
[7] Laws E.R., Thapar K. Unusual lesions in the sella turcica: Intrasellar craniopharyngioma, benign cysts and meningioma. In: Kaye A., Black P.M., editors. Operative Neurosurgery. London: Churchill Livingstone; 2000:723-740.
[8] Thapar K., Kohata T., Laws E.R. Parasellar lesions other than pituitary adenomas. In: Powell M.P., Lightman S.L., Laws E.R., editors. Management of Pituitary Tumors: The Clinician’s Practical Guide. ed 2. Totowa, NJ: Humana Press; 2003:231-286.
[9] Slavin M.J., Weintraub J. Suprasellar meningioma with intrasellar extension simulating pituitary adenoma. Case report. Arch Ophthalmol. 1987;105:1488-1489.
[10] Cook S.W., Smith Z., Kelly D.F. Endonasal transsphenoidal removal of tuberculum sellae meningiomas: technical note. Neurosurgery. 2004;55:239-244. discussion 244–6
[11] Dumont A.S., Jane J.A.J., Laws E.R. Extended transsphenoidal approach. In: Sheehan J.P., Laws E.R., editors. Frontiers of Hormone Research Pituitary Surgery: A Modern Approach. New York: Springer; 2006:29-45.
[12] Jane J.A., Dumont A., Vance M.L., Laws E.R. The transsphenoidal transtuberculum sellae approach for suprasellar meningiomas. Semin Neurosurg. 2003;13:211-218.
[13] Jane J.A., Thapar K., Kaptain G.J., Laws E.R. Transsphenoidal transtuberculum sellae approach for suprasellar and midline anterior cranial fossa tumors. Oper Tech Neurosurg. 2002;5:226-230.
[14] Kaptain G.J., Vincent D.A., Sheehan J.P., Laws E.R. Transsphenoidal approaches for the extracapsular resection of midline suprasellar and anterior cranial base lesions. Neurosurgery. 2001;49:94-100. discussion 100–1
[15] Laurent J.J., Jane J.A.J., Laws E.R. A case of midline suprasellar tumor removal by an extended transsphenoidal skull base technique. In: Kobayashi S., editor. Neurosurgery of Complex Vascular Lesions and Tumors. New York: Theime; 2005:174-177.
[16] Couldwell W.T., Weiss M.H., Rabb C., et al. Variations on the standard transsphenoidal approach to the sellar region, with emphasis on the extended approaches and parasellar approaches: surgical experience in 105 cases. Neurosurgery. 2004;55:539-547. discussion 547–50
[17] Andrews B.T., Wilson C.B. Suprasellar meningiomas: the effect of tumor location on postoperative visual outcome. J Neurosurg. 1988;69:523-528.
[18] Adler J.R., Gibbs I.C., Puataweepong P., Chang S.D. Visual field preservation after multisession cyberknife radiosurgery for perioptic lesions. Neurosurgery. 2006;59:244-254. discussion 244–54