Proceedings of the IV International Giardia and Cryptosporidium Conference, 31 January–03 February 2012, Wellington, New Zealand. Infect Genet Evol. 2013; 15:1–94.
Lakshmi, SP, et al. Ascariasis: challenges in the diagnosis of single worm disease. J Indian Med Assoc. 2013; 111(9):621–622.
Moonah, SN, et al. Host immune response to intestinal amebiasis. PLoS Pathog. 2013; 9(8):e1003489.
Kao, S, et al. Education and imaging. Gastrointestinal: Amebic colitis. J Gastroenterol Hepatol. 2009; 24(1):167.
Ghonge, NP. Gastric migration of intestinal ascariasis: B-mode sonographic depiction. J Ultrasound Med. 2008; 27(12):1799–1801.
Lim, JH. Parasitic diseases in the abdomen: imaging findings. Abdom Imaging. 2008; 33(2):130–132.
Njemanze, PC, et al. High-frequency ultrasound imaging of the duodenum and colon in patients with symptomatic giardiasis in comparison to amebiasis and healthy subjects. J Gastroenterol Hepatol. 2008; 23(7 Pt 2):e34–e42.
Suzuki, A, et al. Education and imaging. Gastrointestinal: ascariasis. J Gastroenterol Hepatol. 2008; 23(11):1770.
Das, CJ, et al. Imaging of ascariasis. Australas Radiol. 2007; 51(6):500–506.
Rana, SS, et al. Parasitic infestations of the biliary tract. Curr Gastroenterol Rep. 2007; 9(2):156–164.
Ali, SA, et al. Giardia intestinalis. Curr Opin Infect Dis. 2003; 16(5):453–460.
McDonald, V. Parasites in the gastrointestinal tract. Parasite Immunol. 2003; 25(5):231–234.
 in the proximal small bowel. These defects represent the roundworm Ascaris lumbricoides.
in the proximal small bowel. These defects represent the roundworm Ascaris lumbricoides.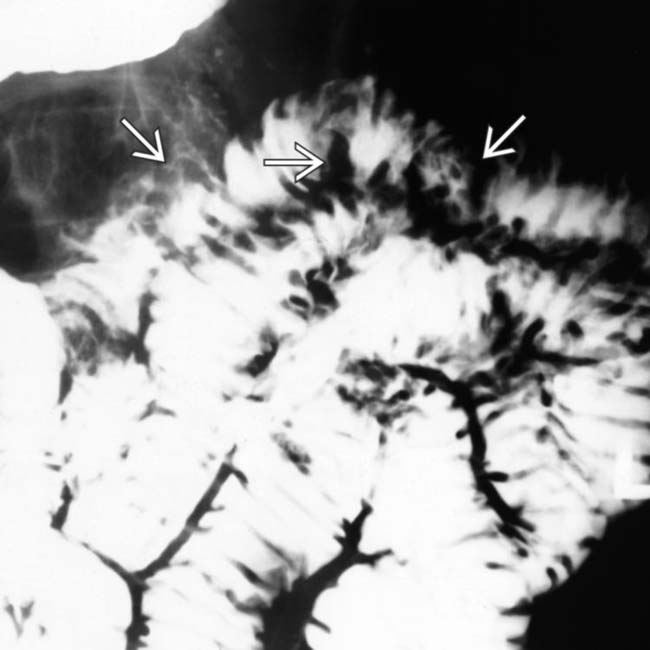
 from giardiasis.
from giardiasis.
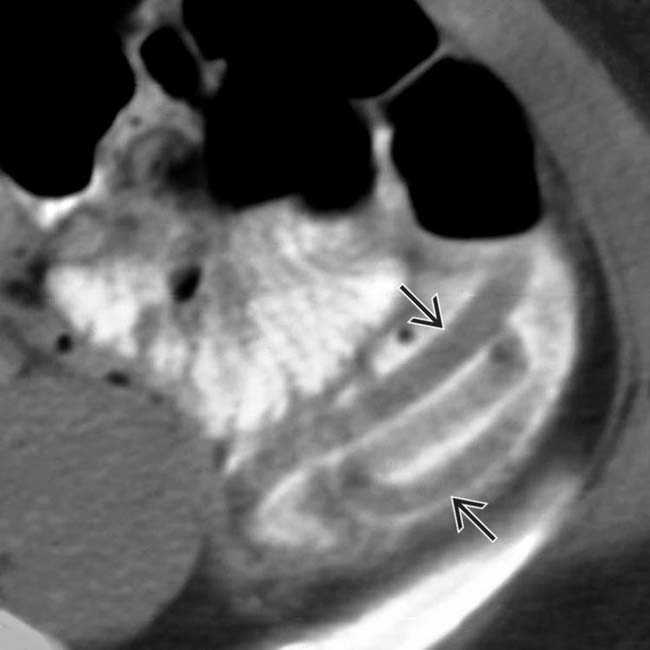
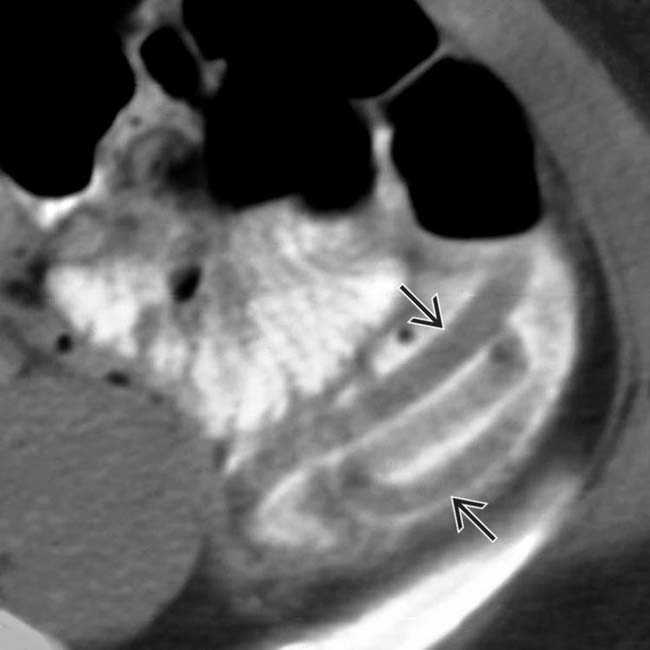
 within the small bowel, essentially diagnostic of Ascaris infestation.
within the small bowel, essentially diagnostic of Ascaris infestation.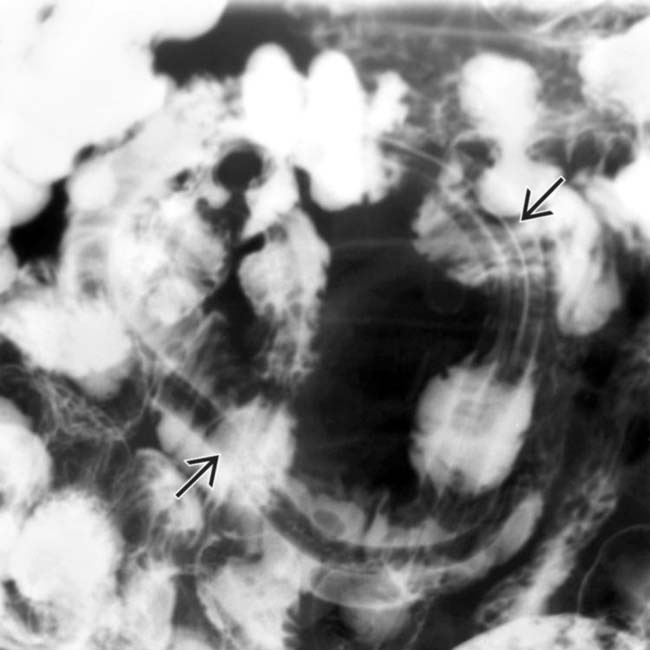
 .
.
 in the proximal small bowel. These defects represent the roundworm Ascaris lumbricoides.
in the proximal small bowel. These defects represent the roundworm Ascaris lumbricoides.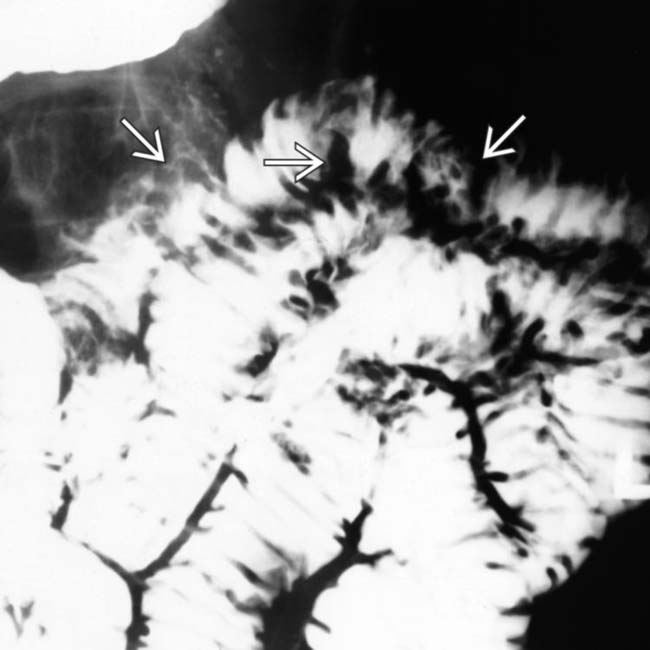
 from giardiasis.
from giardiasis.
 within the small bowel, essentially diagnostic of Ascaris infestation.
within the small bowel, essentially diagnostic of Ascaris infestation.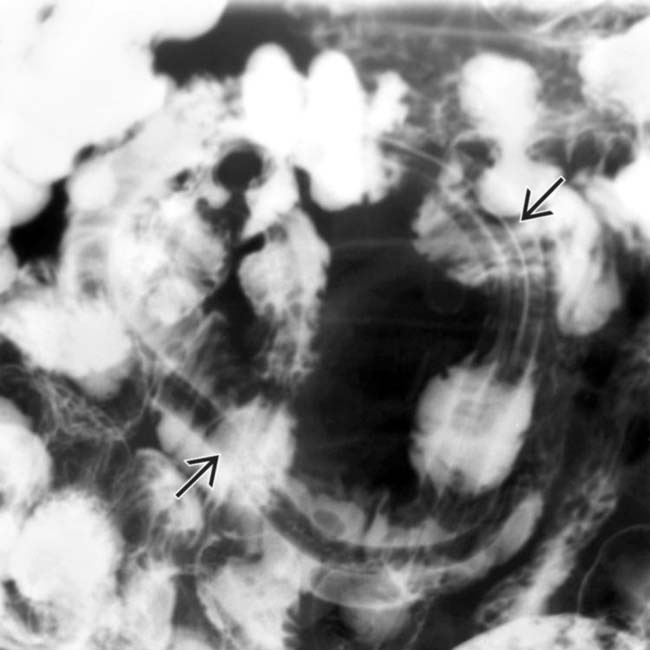
 .
.