Chapter 323 Intestinal Duplications, Meckel Diverticulum, and Other Remnants of the Omphalomesenteric Duct
323.2 Meckel Diverticulum and Other Remnants of the Omphalomesenteric Duct
Melissa Kennedy and Chris A. Liacouras
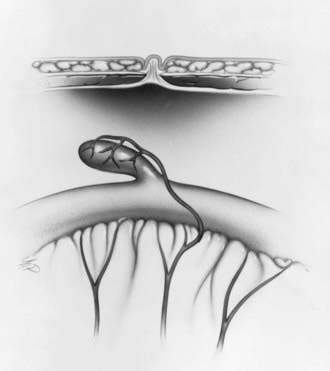
A Meckel diverticulum is a remnant of the embryonic yolk sac, which is also referred to as the omphalomesenteric duct or vitelline duct. The omphalomesenteric duct connects the yolk sac to the gut in a developing embryo and provides nutrition until the placenta is established. Between the 5th and 7th wk of gestation, the duct attenuates and separates from the intestine. Just before this involution, the epithelium of the yolk sac develops a lining similar to that of the stomach. Partial or complete failure of involution of the omphalomesenteric duct results in various residual structures. Meckel diverticulum is the most common of these structures and is the most common congenital GI anomaly, occurring in 2-3% of all infants. A typical Meckel diverticulum is a 3-6 cm outpouching of the ileum along the antimesenteric border 50-75 cm from the ileocecal valve (Fig. 323-1). The distance from the ileocecal valve depends on the age of the patient. Other omphalomesenteric duct remnants occur infrequently, including a persistently patent duct, a solid cord, or a cord with a central cyst or a diverticulum associated with a persistent cord between the diverticulum and the umbilicus.
Diagnosis
Confirmation of a Meckel diverticulum can be difficult. Plain abdominal radiographs are of no value, and routine barium studies rarely fill the diverticulum. The most sensitive study is a Meckel radionuclide scan, which is performed after intravenous infusion of technetium-99m pertechnetate. The mucus-secreting cells of the ectopic gastric mucosa take up pertechnetate, permitting visualization of the Meckel diverticulum (Fig. 323-2). The uptake can be enhanced with various agents, including cimetidine, ranitidine, glucagon, and pentagastrin. The sensitivity of the enhanced scan is approximately 85%, with a specificity of approximately 95%. A false-negative scan may be seen in anemic patients; although false-positive results are uncommon, they have been reported with intussusception, appendicitis, duplication cysts, arteriovenous malformations, and tumors. Other methods of detection include radio-labeled tagged red blood cell scan (the patient must be actively bleeding), abdominal ultrasound, superior mesenteric angiography, abdominal CT scan, or exploratory laparoscopy. In patients who present with intestinal obstruction or a picture of appendicitis with omphalomesenteric duct remnants, the diagnosis is rarely made before surgery.
The treatment of a symptomatic Meckel diverticulum is surgical excision.
Baldisserotto M, Maffazzoni DR, Dora MD. Sonographic findings of Meckel’s diverticulitis in children. AJR Am J Roentgenol. 2003;80:425-428.
Emamian SA, Shalaby-Rana E, Majd M. The spectrum of heterotopic gastric mucosa in children detected by Tc-99m pertechnetate scintigraphy. Clin Nucl Med. 2001;26:529-535.
Fenton LZ, Buonomo C, Share JC, et al. Small intestinal obstruction by remnants of the omphalomesenteric duct: findings on contrast enema. Pediatr Radiol. 2000;30:165-167.
Lee KH, Yeung CK, Tam YH, et al. Laparascopy for definitive diagnosis and treatment of gastrointestinal bleeding of obscure origin in children. J Pediatr Surg. 2000;35:1291-1293.
Rerksuppaphol S, Hutson JM, Oliver MR. Ranitidine-enhanced 99mtechnetium pertechnetate imaging in children improves the sensitivity of identifying heterotopic gastric mucosa in Meckel’s diverticulum. Pediatr Surg Int. 2004 May;20(5):323-325.
Swaniker F, Soldes O, Hirschl RB. The utility of technetium-99m pertechnetate scintigraphy in the evaluation of patients with Meckel’s diverticulum. J Pediatr Surg. 1999;34:760-764.