34 Interpleural Anesthesia
Placement
Anatomy
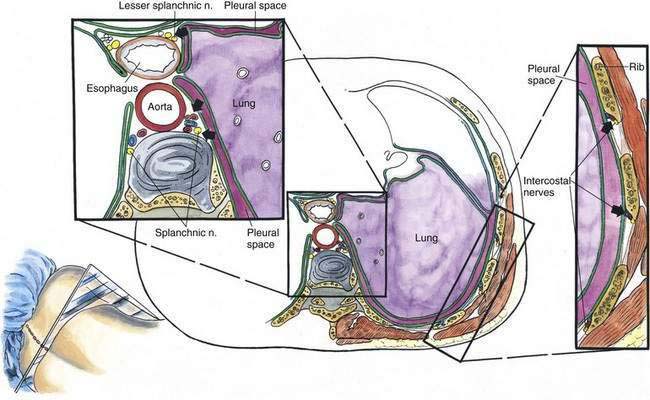
The pleural space extends from the apex of the lung to the inferior reflection of the pleura at approximately L1. The pleural space also relates to the posterior and anterior mediastinal structures, as illustrated in Figure 34-1.
Position
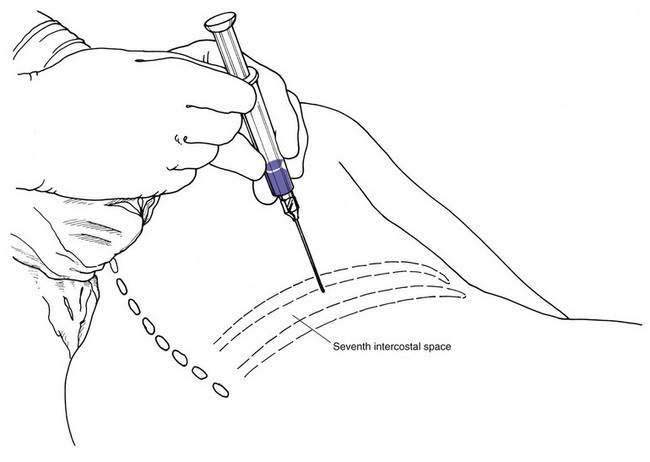
The patient is most often turned to an oblique position with the side to be blocked uppermost, as illustrated in Figure 34-2. The anesthesiologist stands facing the patient’s back.
Needle Puncture
Conversely, some clinicians are proponents of a modified hanging-drop technique to identify entry into the pleural space. These anesthesiologists suggest a new term, falling column, to describe this technique. If the syringe plunger shown in Figure 34-2 is removed and the column of solution in the syringe barrel is observed, entry of the needle tip into the pleural space is identified by a falling column of saline solution. The needle is then secured and the procedure continues as it does with the loss-of-resistance method.
Pearls
The mechanism behind interpleural anesthesia remains uncertain. As illustrated in Figure 34-1, one mechanism proposed is that the local anesthetic diffuses from the pleural space through the intercostal membrane to reach the intercostal nerves along the chest wall. A second mechanism is that the local anesthetic is distributed through the pleura and into the region of the posterior mediastinum, at which point the local anesthetic provides visceral analgesia by contacting the greater, lesser, and least splanchnic nerves. When more data are available, we will probably find that interpleural anesthesia results from a combination of these two mechanisms, plus the absorption of enough local anesthetic from the pleural space to produce blood levels that promote systemic analgesia.