33 Intercostal Block
Placement
Anatomy
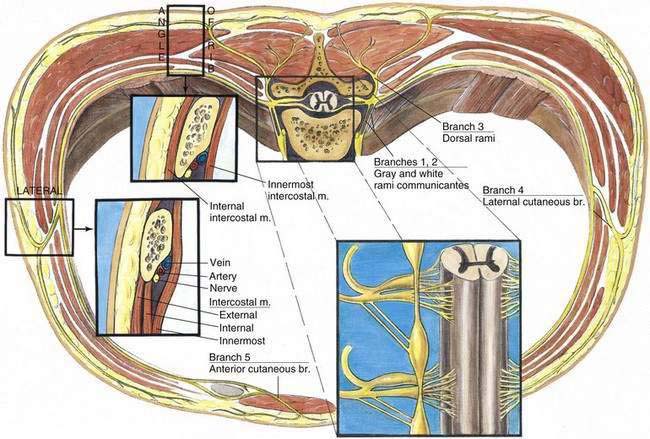
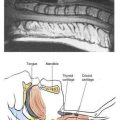
Examination of an individual intercostal nerve shows that there are five principal branches (Fig. 33-1). The intercostal nerve contributes preganglionic sympathetic fibers to the sympathetic chain through the white rami communicantes (branch 1) and receives postganglionic neurons from the sympathetic chain ganglion through the gray rami communicantes (branch 2). These rami are joined to the spinal nerves near their exit from the intervertebral foramina. Also, shortly after exiting from the intervertebral foramina, the dorsal rami carrying posterior cutaneous and motor fibers (branch 3) supply skin and muscles in the paravertebral region. The lateral cutaneous branch of the intercostal nerve arises just anterior to the mid-axillary line before sending subcutaneous fibers posteriorly and anteriorly (branch 4). The termination of the intercostal nerve is known as the anterior cutaneous branch (branch 5). Medial to the angle of the rib, the intercostal nerve lies between the pleura and the internal intercostal fascia. In the paravertebral region, there is loose areolar and fatty tissue between the nerve and the pleura. At the rib’s posterior angle, the area most commonly used during intercostal nerve block, the nerve lies between the internal intercostal muscles and the intercostalis intimus muscle. Throughout the intercostal nerve’s course, it traverses the intercostal spaces inferior to the intercostal artery and vein of the same space.
Needle Puncture
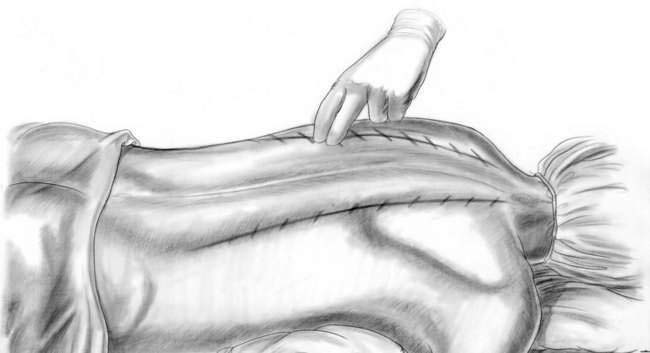
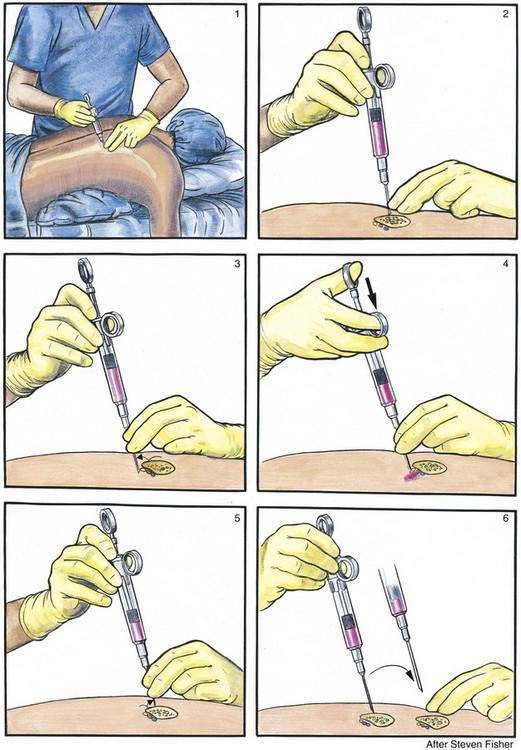
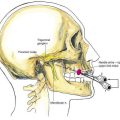
It is advisable to use a marking pen to outline the pertinent anatomy for most regional blocks, and in no block is this more important than in the intercostal nerve block. The midline should be marked from T1 to L5, then two paramedian lines should be drawn at the posterior angle of the ribs. These lines should angle medially in the upper thoracic region so that they parallel the medial edge of the scapula. By successfully palpating and marking the inferior edge of each rib along these two paramedian lines, a diagram like that shown in Figure 33-2 is created. Before needle puncture, appropriate intravenous sedation should be administered to produce amnesia and analgesia during the multiple injections needed for the block. Barbiturates, benzodiazepines, ketamine, or short-acting opioids can be combined. Skin wheals are raised with a 30-gauge needle at each of the previously marked sites of injection, and then intercostal block is carried out bilaterally. As illustrated in Figure 33-3, a 22-gauge, short-beveled, 3- to 4-cm needle is attached to a 10-mL control syringe. It is important that the anesthesiologist adhere to the hand and finger positions illustrated in Figure 33-3 and incorporate them into his or her systematic technique.
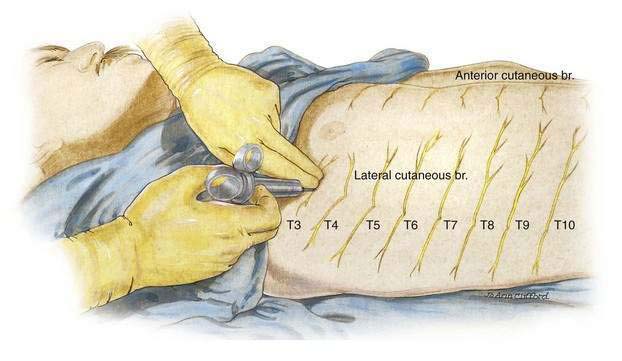
Intercostal block at the posterior angle of the rib is not the only method applicable to clinical regional anesthesia. As outlined in Chapter 32, Breast Block, intercostal block also can be effectively carried out at the mid-axillary line while the patient is in a supine position (Fig. 33-4). This position is clinically more convenient in many situations and probably underused. Some anesthesiologists are concerned that the lateral approach to the intercostal nerve may miss the lateral cutaneous branch of the intercostal nerve. This does not seem to be the case clinically, and computed tomographic studies show that injected solutions spread readily along the subcostal groove for a distance of many centimeters. Therefore, even when lateral intercostal block is carried out, the lateral branch should most often be bathed with local anesthetic solution.