36 Inguinal Block
Perspective
Inguinal block is primarily a technique of peripheral block for inguinal herniorrhaphy.
Placement
Anatomy
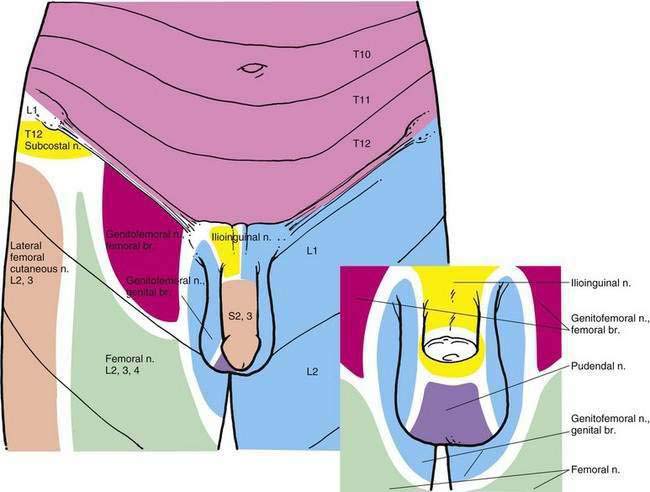
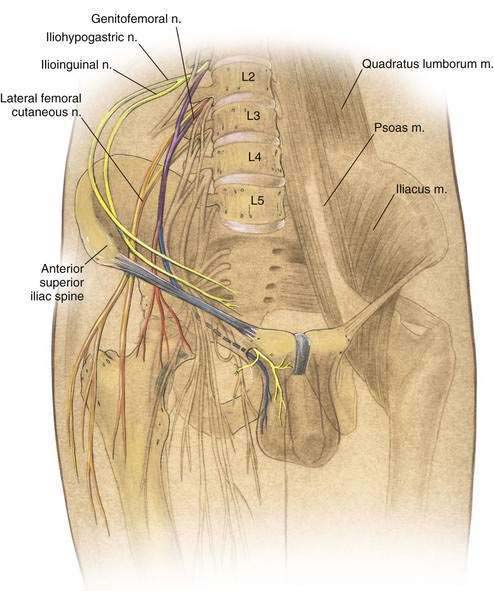
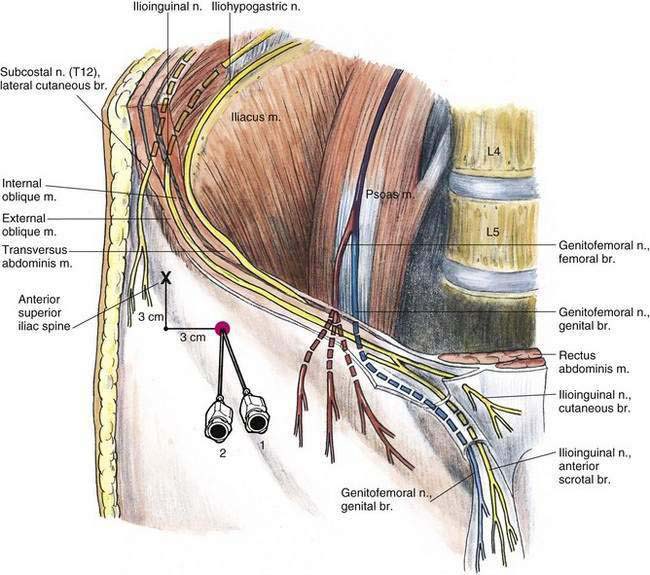
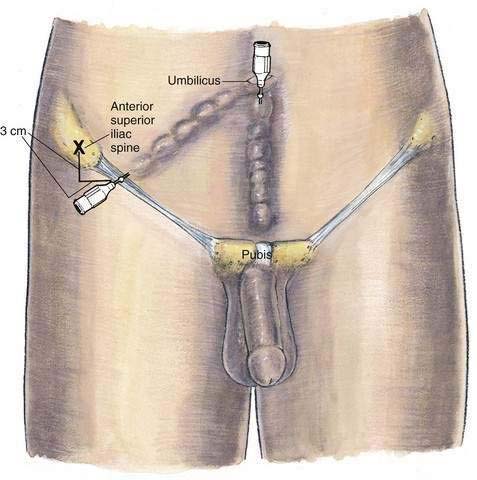
Innervation of the inguinal region arises from the distal extensions of the more cephalad lumbar plexus nerves: the iliohypogastric and ilioinguinal nerves, which have their origin from the first lumbar nerve, and the genitofemoral nerve, which has its origin from the first and second lumbar nerves (Fig. 36-1). These peripheral extensions of the lumbar plexus and the 12th thoracic nerve follow a circular course that is influenced by the bowl-like shape of the ilium. As these nerves course anteriorly, as illustrated in Figure 36-2, they pass near an important landmark for the block, the anterior superior iliac spine. Near the anterior superior iliac spine, the 12th thoracic and iliohypogastric nerves lie between the internal and the external oblique muscles. The ilioinguinal nerve lies between the transversus abdominis muscle and the internal oblique muscle initially and then penetrates the internal oblique muscle some distance medial to the anterior superior iliac spine. All these nerves continue anteriorly in a medial orientation and become superficial as they terminate in the skin and muscles of the inguinal region (Fig. 36-3). As also shown in Figure 36-3, the genitofemoral nerve follows a different course, and it is this nerve that must often be supplemented intraoperatively to make this regional block effective for inguinal herniorrhaphy.
Needle Puncture
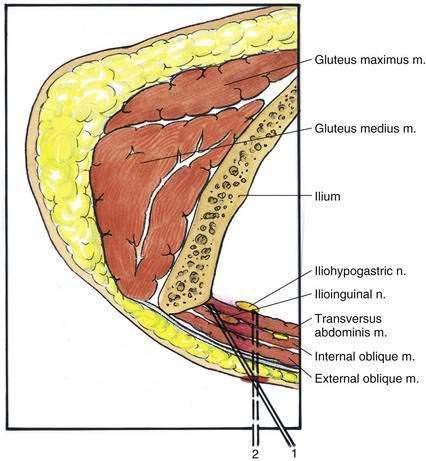
The anterior superior iliac spine should be marked while the patient is supine. Another mark should be made approximately 3 cm medial and inferior to the anterior superior iliac spine (see Fig. 36-3). A skin wheal is created, and an 8-cm, 22-gauge needle is inserted in a cephalolateral direction (needle position 1) to contact the inner surface of the ilium, as illustrated in Figure 36-4. Ten milliliters of local anesthetic solution is injected as the needle is slowly withdrawn through the layers of the abdominal wall. The needle should then be reinserted at a steeper angle to ensure penetration of all three abdominal muscle layers (needle position 2). Again, the injection is repeated as the needle is withdrawn. In patients who are heavily muscled or obese, a third injection may be necessary at an even steeper angle. From the previously placed skin wheal, the injection is extended toward the umbilicus, creating a subcutaneous field block. This process is repeated from umbilicus to pubis (Fig. 36-5). Because the surgeon may need to inject additional local anesthetic into the cord, the anesthesiologist should allow for it to be added intraoperatively without concern over local anesthetic systemic toxicity.