6 Infraclavicular Block
Traditional Block Technique
Placement
Anatomy
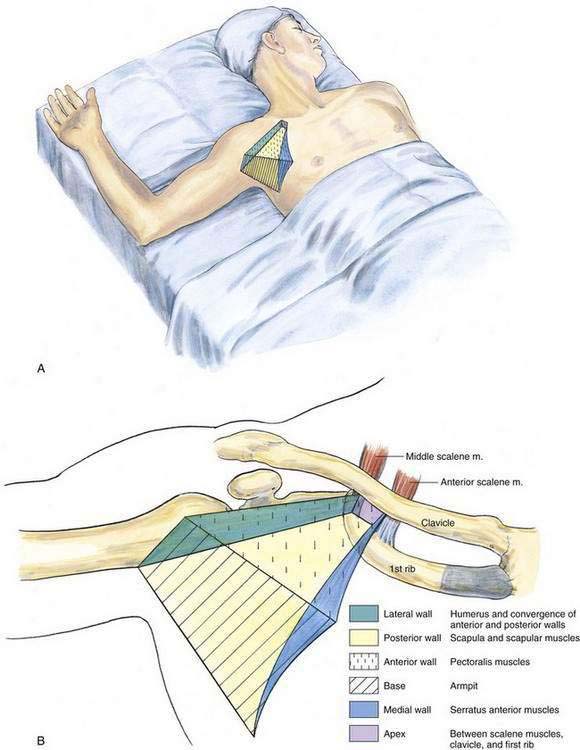
At the level of the proximal axilla, where infraclavicular block is performed, the axilla is a pyramid-shaped space with an apex, a base, and four sides (Fig. 6-1A). The base is the concave armpit, and the anterior wall is composed of the pectoralis major and minor muscles and their accompanying fasciae. The posterior wall of the axilla is formed by the scapula and the scapular musculature, the subscapularis and the teres major. The latissimus dorsi muscle abuts the teres major muscle to form the inferior aspect of the posterior wall of the axilla (Fig. 6-1B). The medial wall of the axilla is composed of the serratus anterior muscle and its fascia, and the lateral wall is formed by the converging muscle and tendons of the anterior and posterior walls as they insert into the humerus (see Fig. 6-1B). The apex of the axilla is triangular and is formed by the convergence of the clavicle, the scapula, and the first rib. The neurovascular structures of the limb pass into the pyramid-shaped axilla through its apex (Fig. 6-2A).
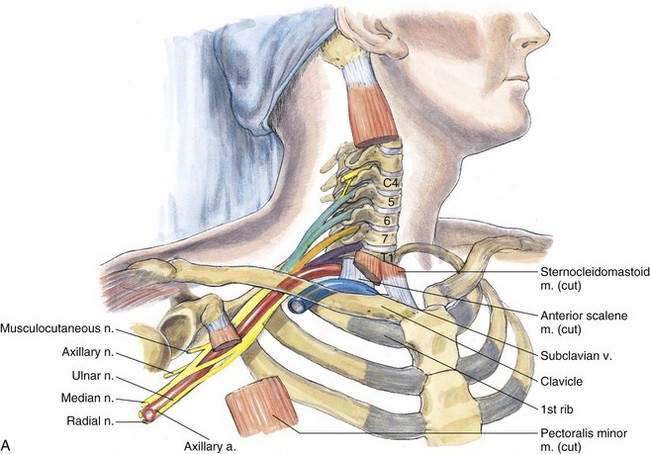
The contents of the axilla are blood vessels and nerves—the axillary artery and vein and the brachial plexus, respectively—and lymph nodes and loose areolar tissue. The neurovascular elements are enclosed within the anatomically variable, multipartitioned axillary sheath, a fascial extension of the prevertebral layer of cervical fascia covering the scalene muscles. The axillary sheath adheres to the clavipectoral fascia behind the pectoralis minor muscle and continues along the neurovascular structures until it enters the medial intramuscular septum of the arm (Fig. 6-2B).
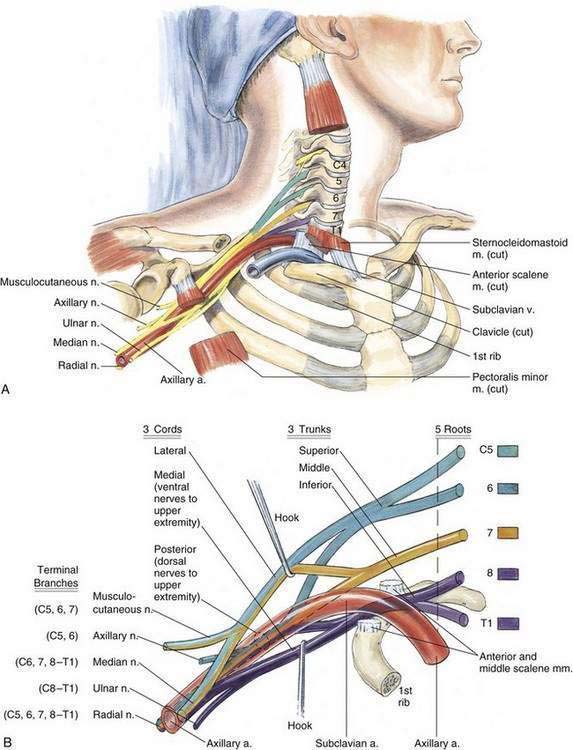
The brachial plexus divisions become cords as they enter the axilla. The posterior divisions of all three trunks unite to form the posterior cord; the anterior divisions of the superior and middle trunks form the lateral cord; and the nonunited anterior division of the inferior trunk forms the medial cord. These cords are named according to their relationship to the second part of the axillary artery (Fig. 6-3). From these cords, nerves to the subscapularis, pectoralis major and minor, and latissimus dorsi muscles leave the brachial plexus. The medial brachial cutaneous, medial antebrachial cutaneous, and axillary nerves also leave the brachial plexus from the level of the cords.
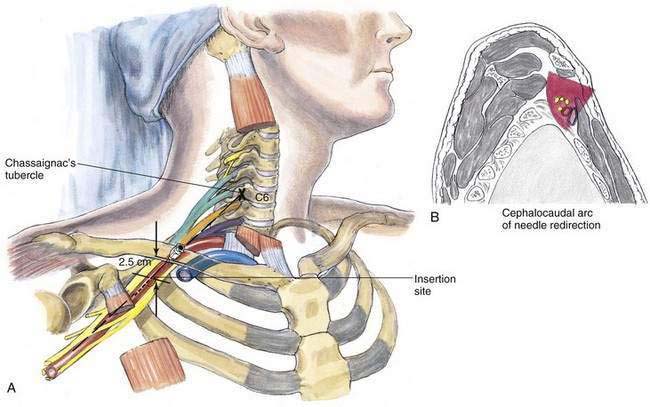
Needle Puncture
With the arm abducted at the shoulder, the coracoid process is identified by palpation and a skin mark placed at its most prominent portion. The skin entry mark is then made at a point 2 cm medial and 2 cm caudad to the previously marked coracoid process (Fig. 6-4A). Deeper infiltration is then performed with a 25-gauge, 5-cm needle while the needle is directed from the insertion site in a vertical parasagittal plane. Then a 6- to 9.5-cm, 20- to 22-gauge needle is inserted in a direction similar to that taken by the infiltration needle. If a paresthesia technique is used, a distal upper extremity paresthesia is sought; if a nerve stimulator technique is used, a distal upper extremity motor response is sought. If needle redirection is needed to achieve either a paresthesia or a motor response, the needle should be redirected in a cephalocaudad arc (Fig. 6-4B). The depth of contact with the brachial plexus depends on body habitus and needle angulation; it ranges from 2.5 to 3 cm in slender patients and from 8 to 10 cm in larger individuals.
Ultrasonography-Guided Technique
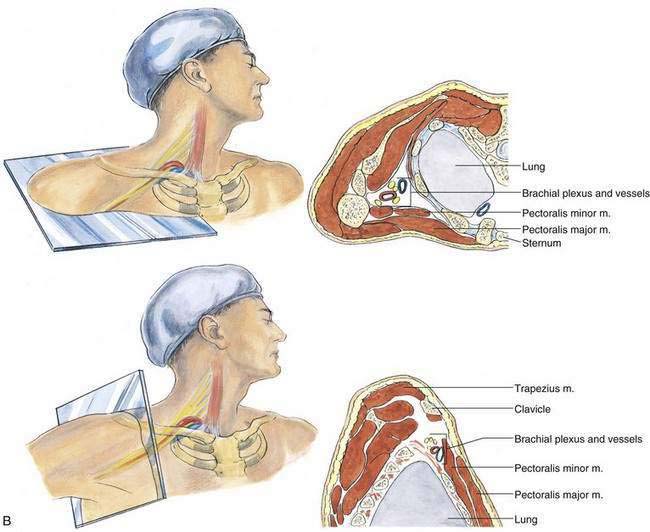
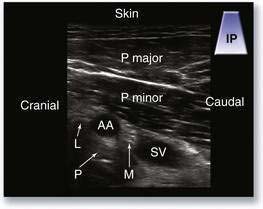
To start, the operator should place the transducer inferior to the clavicle, such that a sagittal image slice of the patient is created on the image screen (Fig. 6-5). The subclavian artery and vein should appear in short axis and as circular hypoechoic structures posterior to the pectoralis major and minor muscles. If there is difficulty locating the vessels, the operator should slide the transducer laterally and increase the depth settings. Next, the medial edge of the transducer should be rotated caudad to optimize the short-axis view of the vessels. The three cords of the brachial plexus should be identified around the subclavian artery as hyperechoic circles or ovals with hypoechoic fascicles (Fig. 6-6). The operator should be aware of the amount of pressure being applied to the transducer because it is possible to compress the subclavian vein unintentionally despite the transducer’s distance from the vessel.
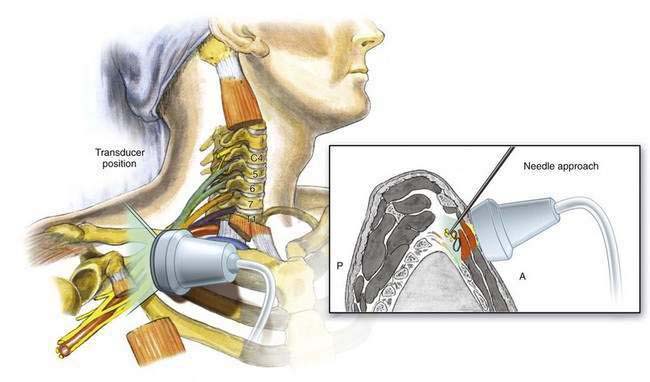
Figure 6-5. Parasagittal section of infraclavicular block with anatomic correlates. A, anterior; P, posterior.
Pearls
To produce an effective infraclavicular block, the operator must be able to visualize the three-dimensional anatomy of the pyramid-shaped axilla and be able to move the needle tip effectively through a cephalocaudad arc to locate the plexus (see Fig. 6-4B). In addition, when placing the needle the operator should strive to obtain a distal upper extremity motor response through nerve stimulation—or obtain a definite distal paresthesia, if that approach is taken—to produce optimal needle position. Once the infraclavicular catheter is placed and secured, it is much more effective than any other brachial plexus continuous catheter technique. This reason alone makes the infraclavicular block my preferred site for continuous catheter brachial plexus analgesia. Because this technique crosses two pectoral muscle fascial planes, it is often more painful than other brachial plexus techniques. I therefore prefer to use a nerve stimulator or ultrasonography for plexus localization combined with heavier sedation than that used with other brachial techniques. The location of the stimulating needle or catheter can be ascertained by observing the motor response of the fifth digit to stimulation with this technique while the arm is in anatomic position. If the fifth digit moves laterally (pronation of the forearm), the lateral cord is being stimulated. If the fifth digit moves posteriorly (extension of the wrist), the posterior cord is being stimulated. Finally, if the fifth digit moves medially (flexion of the wrist), the medial cord is being stimulated.