Chapter 17 Infertility
Infertility
Causes of female factor infertility
| Unexplained infertility | 28% |
| Male factor infertility | 21% |
| Ovulatory disorders | 18% |
| Tubal disease | 14% |
| Endometriosis | 6% |
| Coital problems | 5% |
| Cervical factors | 3% |
Investigations
Investigations in the primary setting
| Female partner | Cervical smear test. |
| Urine test for Chlamydia (this can cause blockages of the fallopian tube). | |
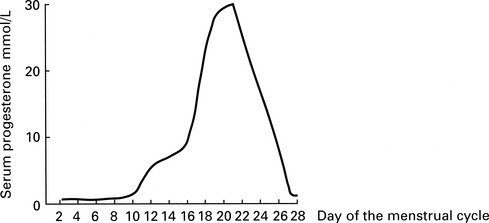
| Serum progesterone level to check ovulation. This is taken 1 week prior to menstruation, hence day 21 for a 28-day cycle or day 28 for a 35-day cycle (see below). | |
| Rubella immunity – if rubella is contracted during the first 3 months of pregnancy it can seriously harm the developing fetus Women who are not immune to rubella should be vaccinated, and advised to avoid pregnancy for 3 months. | |
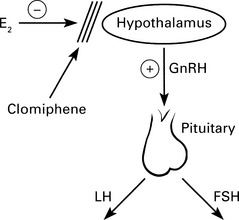
| Measuring serum FSH (follicle stimulating hormone), LH (luteinising hormone) and oestradiol to identify hormone imbalances or possible early menopause. | |
| Male partner | Semenalysis to check for abnormalities of the sperm such as number, motility, and morphology (see below). |
| Urine test for Chlamydia, which, in addition to being a known cause of infertility in women, can also affect sperm function and male fertility. |
Investigations in the secondary setting
| Female partner | Measuring serum FSH, LH and oestradiol to identify hormone imbalances or possible early menopause. |
| Serum progesterone level to check ovulation. This is taken 1 week prior to menstruation, hence day 21 for a 28-day cycle or day 28 for a 35-day cycle. | |
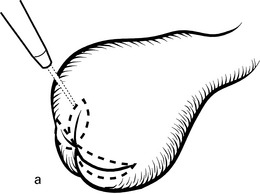
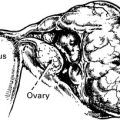
| A pelvic ultrasound scan to look at uterine and ovarian anatomy. | |
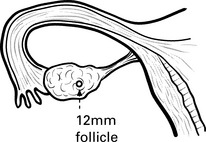
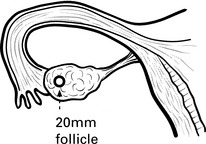
| Serial ultrasound tracking of the ovaries for looking at developing follicles (see below). | |
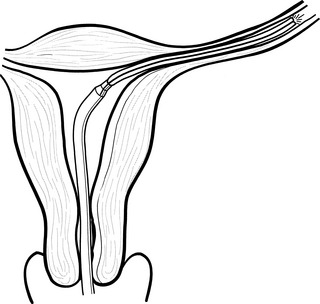
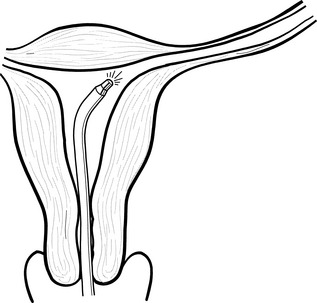
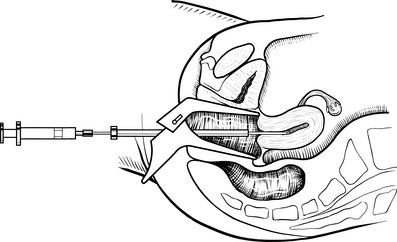
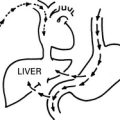
| Checking of tubal patency – either by hysterosalpingogram, hysteron-contrast sonography or laparoscopic hydrotubation. | |
| Diagnostic laparoscopy – to check for problems with tubal and uterine anatomy. | |
| Hysteroscopy – to check for uterine conditions such as fibroids or polyps | |
| Endometrial biopsy (in rare cases) see below. | |
| Male partner | Semenalysis to check for abnormalities of the sperm such as number, motility and morphology (see below). |
| Sperm antibody test to check for protein molecules that may prevent sperm from fertilising an egg. |
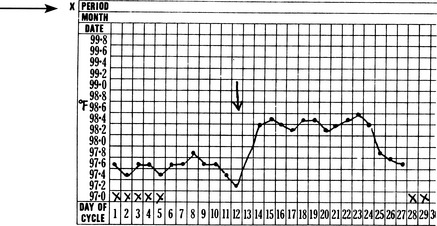
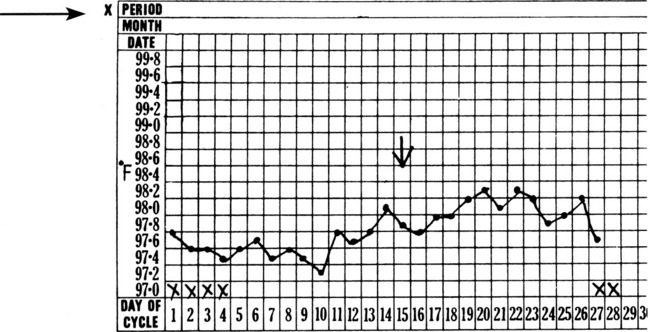
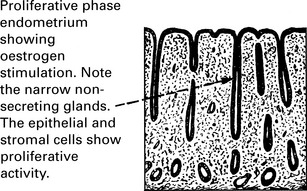
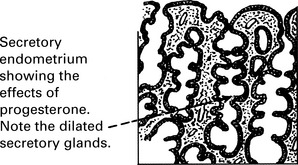
Evidence of ovulation
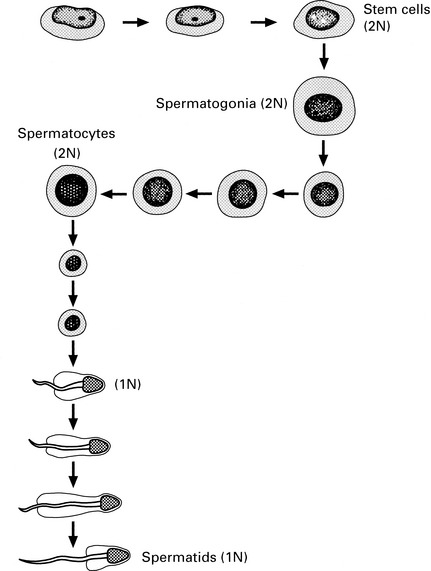
Abnormalities in sperm production
The causes of abnormalities in sperm production include:
1. Acute and chronic infection of the male genital tract. Gonococcal and coliform infections respond to antibiotics but chronic prostatitis can be difficult to treat. Spermatozoa are reduced in number and tend to be malformed and non-motile.
Viral infections can be important, especially mumps. Testicular atrophy may follow this infection.
2. Immunological reactions in the form of auto-antibodies occur in a variable number of men (3–12%). Formation of these antisperm antibodies may be stimulated by infection or by injury, but in most cases the cause is obscure. Steroids in short courses may be helpful.
These include social habits such as smoking, alcohol and drugs.
The list of occupations involving substances that are toxic to sperm count is remarkably long:
A large number of therapeutic agents also affect spermatogenesis.
1. Chemotherapeutic agents – these depress sperm production and cause germinal epithelial aplasia. Rising FSH levels are an indication of these changes.
2. Sulfasalazine reduces sperm motility and number. These effects are reversed if treatment is stopped.
3. Cimetidine, spironolactone and ketoconazole interfere with androgen action and may affect spermatogenesis.
4. Anabolic steroids profoundly depress spermatogenesis, but the effect is reversible when the drug is withdrawn.
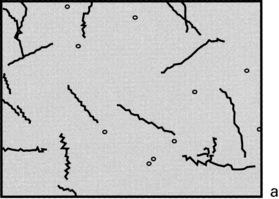
Sperm function tests
Assisted conception
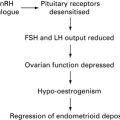
Fertility drugs
Assisted conception techniques
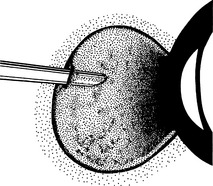
In vitro fertilisation
Indications for in vitro Fertilisation
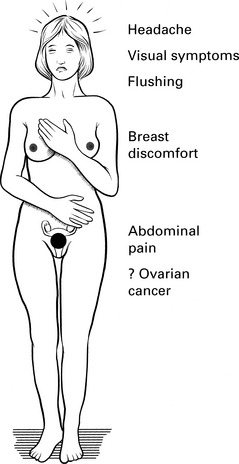
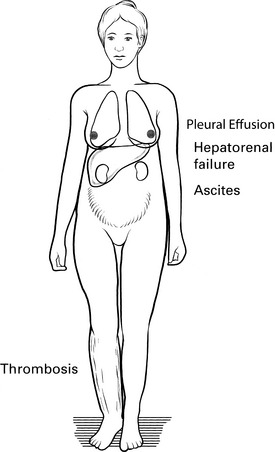
Risks of IVF Treatment
(2) Multiple births (twins, triplets or more) – this is the single greatest health risk associated with fertility treatment. The Human Fertilisation and Embryology Authority (HFEA) has imposed restrictions on the number of embryos that can be transferred during IVF in order to reduce the number of multiple births. Multiple births carry risks for both the mother and fetuses. The babies are more likely to be premature and tend to have below-normal birth weight. The perinatal mortality rate has been shown to be four times greater in twins compared to singletons, and for triplets, the risk is seven times greater than for singletons. In addition, the risk of cerebral palsy is five times higher for twins and 18 times higher for triplets, compared to singletons.