Infections of the nervous system II
Spinal infections
Poliomyelitis is now extremely rare. It can lead to a myelitis and leave significant neurological deficit (p. 109).
Pyogenic infection in the vertebral body or in the epidural space can lead to an epidural abscess (Fig. 1), producing back pain often associated with fever. This is followed by radicular pain and then symptoms and signs of spinal cord or cauda equina involvement. If this diagnosis is suspected then urgent investigation with spinal MRI is needed, as early drainage of the abscess and high-dose antibiotics is the only hope of reversing this process. A similar, if slower, onset is associated with tuberculous epidural abscess. Treatment of this is primarily antituberculous therapy, though in some patients surgery is needed.
Syphilis
Tropical neurology
Infections play a larger part in neurology in tropical countries. For example, cysticercosis, schistosomiasis and paragonimiasis (oriental liver fluke) are common causes of seizures in different parts of the world. Cerebral malaria is a common cause of coma and death in parts of Africa. All these conditions are seen in people who have travelled in tropical countries, so a travel history is an important clue in the diagnosis of these conditions.
HIV infections and AIDS
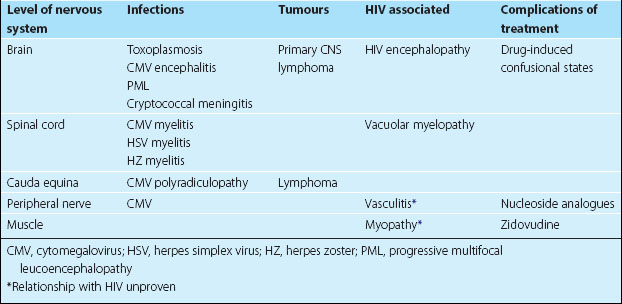
Most neurological problems in HIV infection occur as the patient develops significant immunosuppression. Opportunistic infections, tumours, specific neurological problems associated with HIV and neurological complications of the treatment of HIV infection then occur. Different levels of the nervous system are affected and are summarized in Table 1.
Toxoplasmosis
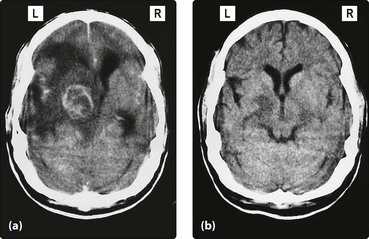
This presents with a focal neurological deficit, headache or seizures, usually developing over a few weeks (Fig. 2). Brain scanning reveals single or multiple ring-enhancing masses with oedema. As this is the most likely diagnosis in this setting, a trial of anti-toxoplasma treatment is given. Further investigation is considered if this fails. The most common differential diagnosis is primary CNS lymphoma. This can be treated with radiotherapy but the response and prognosis are poor.