Infections of the Nervous System and Senses
After reading this chapter, the student will be able to:
• Describe how microorganisms can gain access to the nervous system
• Describe the symptoms of meningitis; discuss the different causes and the different treatment approaches for each type of the illness
• Discuss the different forms of bacterial meningitis; include the cause, symptoms, and treatments
• Describe the four different types of tetanus and the causes, prevention, and treatment
• Discuss botulism and the different types of toxins produced by the different strains
• Explain the causes, symptoms, and treatment of leprosy
• Describe the causes, symptoms, and treatment of conjunctivitis
• Describe the causes, symptoms, prevention, and treatments of poliomyelitis, rabies, and arboviral encephalitis
• Describe the typical fungal infections of the human nervous system
• Differentiate between African and American trypanosomiasis
• Describe prions and the human diseases associated with them
Introduction
The nervous system is divided into two components: the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS consists of the brain and spinal cord, and the PNS consists of 12 pairs of cranial nerves, 31 pairs of spinal nerves, ganglia, and associated sensory receptors (Figure 13.1). The brain and the spinal cord are covered by three protective membranes, collectively called meninges (Figure 13.2). The outermost membrane is the dura mater, the middle layer is the arachnoid, and the innermost membrane is the pia mater. The space between the pia mater and the arachnoid, referred to as the subarachnoid space, contains cerebrospinal fluid (CSF), which circulates through the brain ventricles, the central canal of the spinal cord, and the subarachnoid space. The CSF has a low level of complement proteins, circulating antibodies, and some phagocytotic cells; if bacteria get access to the CSF they can multiply with little immune reaction by the body.
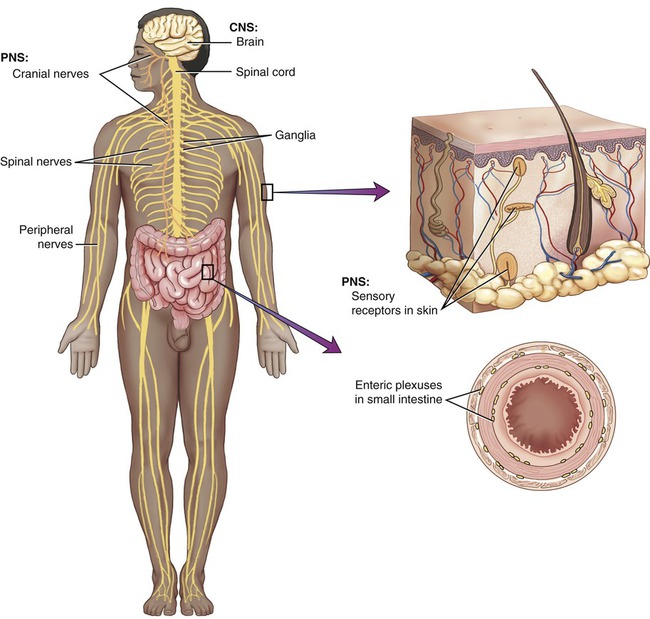
The nervous system is divided into two components: the central nervous system composed of the brain and the spinal cord, and the peripheral nervous system containing the cranial and spinal nerves, ganglia, and sensory receptors.
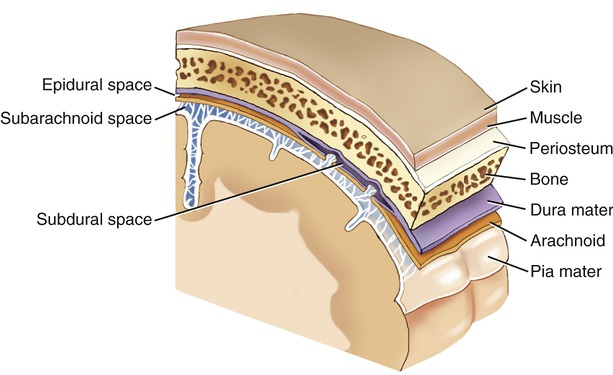
The brain and the spinal cord are covered by three protective membranes, collectively called meninges. The outermost membrane is the dura mater, the middle layer is the arachnoid, and the innermost membrane is the pia mater.
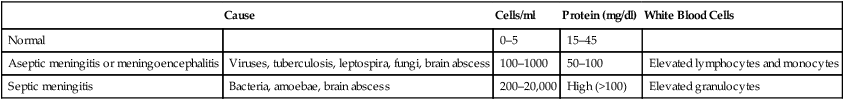
During a CNS infection specific changes occur within the CSF. The response in the CSF to a viral infection is generally reflected by an increase in lymphocytes, monocytes, and a slight increase in proteins, and the CSF remains clear. This condition is called aseptic meningitis. In the case of a bacterial infection a rapid increase in granulocytes and proteins occurs and the CSF becomes visibly turbid. This condition is called septic meningitis (Table 13.1).
TABLE 13.1
Cerebrospinal Fluid (CSF) Changes During CSF Infections
| Cause | Cells/ml | Protein (mg/dl) | White Blood Cells | |
| Normal | 0–5 | 15–45 | ||
| Aseptic meningitis or meningoencephalitis | Viruses, tuberculosis, leptospira, fungi, brain abscess | 100–1000 | 50–100 | Elevated lymphocytes and monocytes |
| Septic meningitis | Bacteria, amoebae, brain abscess | 200–20,000 | High (>100) | Elevated granulocytes |
The CNS is remarkably resistant to infection, largely because of a barrier between the blood circulation and the nervous tissue, referred to as the blood–brain barrier. The capillaries of the blood–brain barrier permit only selected substances to pass from the blood into the brain, with all others being restricted. In essence, only lipid-soluble substances can cross the barrier; the exception is glucose and certain amino acids, none of which are lipid soluble, but that have specific carrier mechanisms transporting them across the barrier. Unless they are lipid soluble, drugs cannot cross the blood–brain barrier. For example, chloramphenicol, a lipid-soluble antibiotic (see Chapter 22, Antimicrobial Drugs), can readily enter the brain whereas penicillin, only slightly lipid soluble, is effective only if taken in large doses.
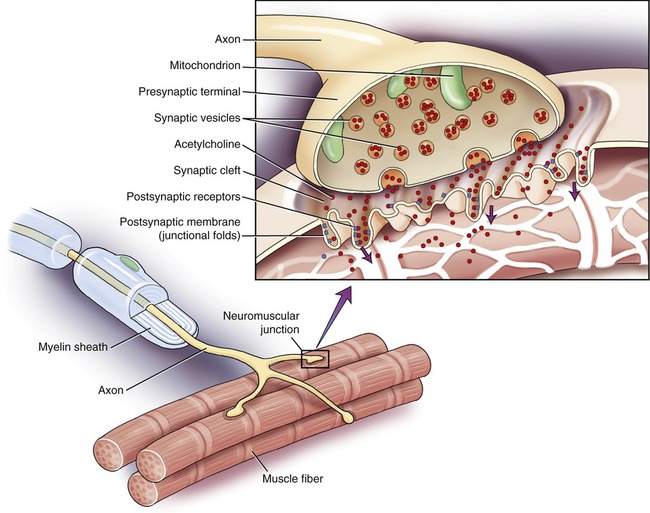
Another structure that can be affected by microorganisms or their toxins is the neuromuscular junction. The neuromuscular junction (Figure 13.3) is the connection between the synaptic end bulb (axon terminal) of a motor neuron, located in the spinal cord, and a muscle fiber. This junction is essential for muscle contraction. The two cells do not touch each other but are separated by a small space called the synaptic cleft. The electrical message from the motor neuron is translated into a chemical message via the neurotransmitter (acetylcholine) located in the presynaptic terminal. Once the neurotransmitter is released into the synaptic cleft it diffuses to the receptors on the muscle fiber and generates another electrical event that leads to muscle contraction. Any interference with this delicate structure will lead to problems with muscle contraction.
Bacterial Infections
Bacterial Meningitis
Bacterial meningitis is less common than viral meningitis but is more severe in nature, because of the production of toxins by the bacteria. The mortality rate for bacterial meningitis varies with the causative agent, and vaccination is available for some. Early diagnosis and treatment of bacterial meningitis are essential to prevent permanent neurological damage. Antibacterial drugs used to treat bacterial meningitis include penicillin G, ampicillin or amoxicillin, chloramphenicol, cefotaxime, vancomycin, and ceftriaxone (see Chapter 22, Antimicrobial Drugs).
Meningococcal Meningitis
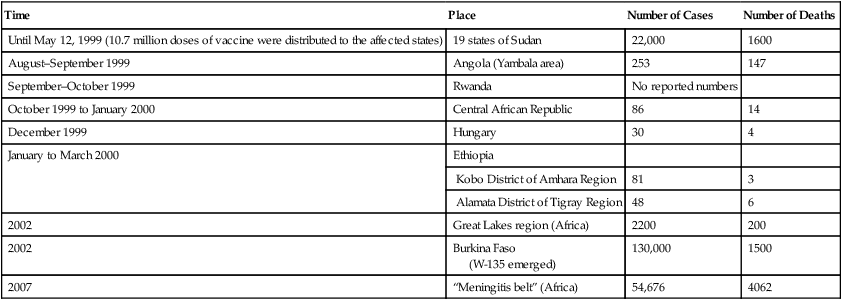
Outbreaks of meningococcal meningitis occur globally. It is endemic in temperate climates, with sporadic cases or small clusters of cases exhibiting seasonal increases in winter and spring. In the United States sporadic outbreaks occur among college students who live in dormitories. Epidemics of meningococcal meningitis have occurred in Africa in periodic waves. In 2002 outbreaks occurred in the Great Lakes region of Central Africa in villages and refugee camps. More than 2200 cases were reported, including 200 deaths (Table 13.2). More recently, during 2007, 54,676 suspected cases of meningitis and 4062 deaths were reported from the “meningitis belt” region in Africa. This region covers 21 sub-Saharan African countries with a population of about 350 million people.
TABLE 13.2
Recent Outbreaks of Meningococcal Meningitis Worldwide
| Time | Place | Number of Cases | Number of Deaths |
| Until May 12, 1999 (10.7 million doses of vaccine were distributed to the affected states) | 19 states of Sudan | 22,000 | 1600 |
| August–September 1999 | Angola (Yambala area) | 253 | 147 |
| September–October 1999 | Rwanda | No reported numbers | |
| October 1999 to January 2000 | Central African Republic | 86 | 14 |
| December 1999 | Hungary | 30 | 4 |
| January to March 2000 | Ethiopia | ||
| Kobo District of Amhara Region | 81 | 3 | |
| Alamata District of Tigray Region | 48 | 6 | |
| 2002 | Great Lakes region (Africa) | 2200 | 200 |
| 2002 | Burkina Faso (W-135 emerged) |
130,000 | 1500 |
| 2007 | “Meningitis belt” (Africa) | 54,676 | 4062 |
Haemophilus influenzae Meningitis
Prevention can be provided by several types of Hib vaccines available for children 2 months of age or older. Immunization is recommended for infants and children by the American Academy of Pediatrics, the National Institutes of Health, and other health agencies. Ideally, the first dose of the vaccine should be administered at the age of 2 months, followed by three or four booster vaccinations (see Chapter 20, The Immune System), depending on the brand of vaccine used.
Pneumococcal Meningitis
Pneumococci are also the cause of millions of cases of acute otitis media (middle ear infection) annually (Figure 13.4), and approximately 500,000 cases of pneumonia per year in the United States (see Chapter 11, Infections of the Respiratory System). Middle ear infections are one of the most common reasons for physician’s office visits in the United States, resulting in more than 20 million visits annually. In general, by the age of 12 months 60% of children have had at least one episode of acute otitis media. Complications of pneumococcal otitis media include mastoiditis and meningitis.
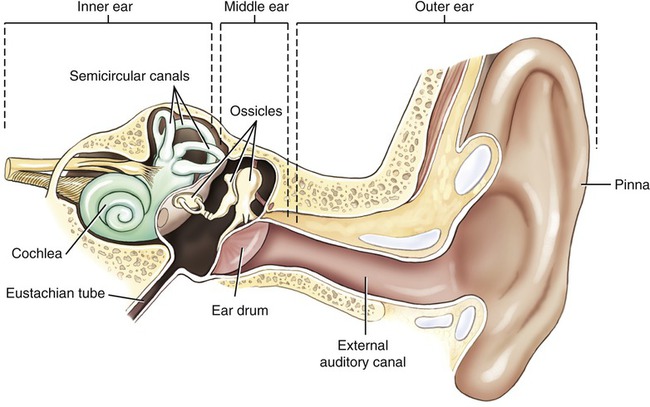
The human ear consists of the outer ear, middle ear, and inner ear.
• High-risk persons age 2 years and over
• Everyone age 65 years and older
• Patients with sickle cell anemia
• Patients with chronic organ failure
• Residents of nursing homes and other long-term care facilities
• People who live in institutions with residents who have chronic health problems
• People with a compromised immune system such as patients with HIV, patients with cancer, or patients who have received an organ transplant
• Persons who receive long-term immunosuppressive drugs, including steroids
• Alaskan natives and certain Native American populations who are genetically predisposed
A serious problem with pneumococcal diseases including meningitis is the increasing emergence of antibiotic-resistant strains of S. pneumoniae (also see Chapter 11, Infections of the Respiratory System). Antibiotic-resistant strains are most likely to emerge in settings where antibiotics are commonly prescribed such as in hospitals, nursing homes, and day care centers. At present between 10% and 40% of all infections caused by S. pneumoniae are resistant to at least one antibiotic, but more and more multidrug-resistant strains are emerging in the United States. Therefore, vaccination of at-risk groups will play an even more important role in preventing pneumococcal disease in the near future.
HEALTHCARE APPLICATION
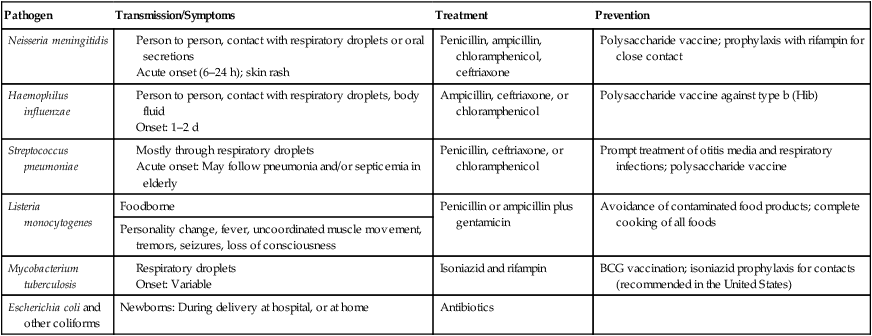
Bacterial Meningitis
| Pathogen | Transmission/Symptoms | Treatment | Prevention |
| Neisseria meningitidis |
Listeria Meningitis
Listeria monocytogenes is a gram-positive coccobacillus and is the causative agent of listeriosis (see Chapter 12, Infections of the Gastrointestinal System), a foodborne illness. This organism can spread from the bloodstream to the central nervous system, causing meningitis, especially in the elderly and in immunocompromised patients, especially patients with cancer. Listeria meningitis is often fatal, and occurs in approximately half the cases of adult listeriosis. The more serious symptoms appear about 4 days after the initial symptoms of slight fever, headache, nausea, vomiting, diarrhea, and tiredness. The symptoms of Listeria meningitis include the following:
• Early-onset disease refers to a serious illness that is present at birth and usually causes the baby to be born prematurely. Approximately 50% of the newborns infected with Listeria will die of the illness.
• Late-onset disease occurs when a full-term baby becomes infected with Listeria during childbirth, and symptoms generally appear about 2 weeks after birth. These babies typically have meningitis, but have a better chance of survival than those with early-onset disease.
Tetanus
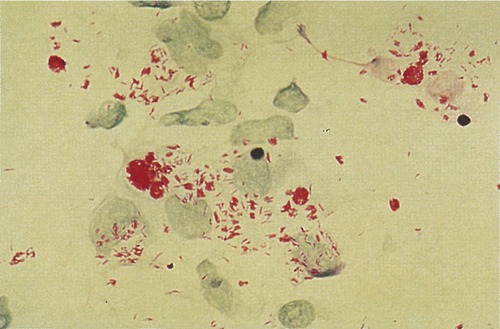
Tetanus is an acute, often fatal illness, characterized by prolonged contraction of skeletal muscle fibers, resulting in generalized rigidity and convulsive spasms of the skeletal muscles. The symptoms are caused by tetanospasmin, a neurotoxin (exotoxin) produced by Clostridium tetani, a gram-positive, anaerobic rod that may develop a terminal spore, giving it a drumstick-like appearance (Figure 13.5). Whereas the vegetative organism is sensitive to heat and cannot survive the presence of oxygen, the spores are extremely resistant to heat as well as to the usual antiseptics. The spores are also relatively resistant to phenol and other chemical antimicrobial agents.
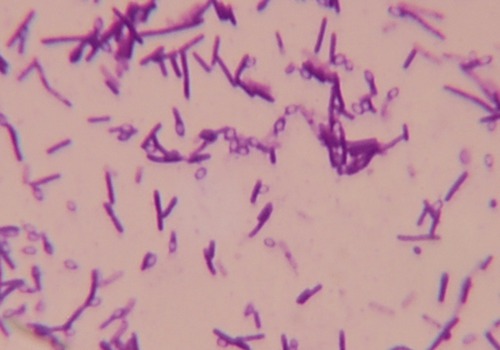
Clostridium tetani, the causative agent of tetanus, is a gram-positive anaerobic rod that may develop a terminal spore, giving it a drumstick-like appearance.
• Local tetanus occurs when patients have persistent contractions of muscles at the site of injury. This is an uncommon form of the illness and may persist for many weeks before gradually subsiding. Local tetanus is generally a milder condition and only about 1% of cases are fatal; however, the condition may precede the onset of generalized tetanus.
• Cephalic tetanus is a rare form of the disease, which can occur when C. tetani is present in the flora of the middle ear or following head injuries. This condition involves the cranial nerves, especially those innervating the facial area.
• Generalized tetanus is the most common type of tetanus, responsible for about 80% of reported cases. The first sign of this condition is trismus or lockjaw, followed by stiffness of the neck, difficulty in swallowing, and rigidity of the pectoral and calf muscles. Spasms may occur frequently and last for several minutes. These spasms may continue for 3 to 4 weeks and approximately 11% of reported cases have been fatal.
• Neonatal tetanus is a form of tetanus that occurs in newborns who have not acquired the necessary passive immunity from the mother, because she has never been immunized. The condition can occur through infections of an unhealed umbilical stump. This type of tetanus most commonly occurs in developing countries and is responsible for approximately 14% of all neonatal deaths. Neonatal tetanus is rare in the United States and other developed countries.
Botulism
Botulism is a rare, serious illness caused by Clostridium botulinum, an anaerobic, gram-positive, spore-forming rod that produces a potent neurotoxin (see also Chapter 12, Infections of the Gastrointestinal System). The organism and its spores are widely distributed in nature. They are present in cultivated and forest soils; the bottom sediment of streams, lakes, and coastal waters; and also in the intestinal tract of fish and mammals and in the gills and viscera of crabs and other shellfish. Seven serotypes of botulism are documented (A, B, C, D, E, F, and G), based on the antigenic specificity of the toxin produced by each strain. Only types A, B, E, and F cause human botulism; types C and D are the cause of most cases of botulism in animals. The toxins produced by the different strains vary considerably in their virulence factors.
• Type A toxin is probably the most virulent of all the botulinum toxins, with lethality occurring at 10–9 g levels of exposure. Death can occur when contaminated food is only tasted, not even swallowed. Lethal doses can also be absorbed by small breaks in the skin. If untreated, intoxication with type A toxins results in a 60% to 70% mortality rate. In the United States the strain producing type A toxin is found predominantly in California, Washington, Colorado, Oregon, and New Mexico.
• Type B toxin is responsible for most European outbreaks of botulism and also is the most common type in the eastern United States. The mortality rate is about 25% if left untreated.
• Type E toxin is produced by a Clostridium species commonly found in marine or lake sediments, and therefore outbreaks are usually associated with seafood, especially in the Pacific Northwest, Alaska, and the Great Lakes area of the United States.
• Type F toxin is also produced by C. baratii and has been shown to cause infant botulism. Type F toxin is also used in the treatment of spasmodic torticollis, a painful and debilitating neurological movement disorder.
Four types of botulism are recognized (also see Chapter 12, Infections of the Gastrointestinal System):
Leprosy
• The skin (see Chapter 10, Infections of the Integumentary System, Soft Tissue, and Muscle)
• The peripheral nerves, primarily those in the hands and feet
• The mucous membranes of the nose, throat, and eyes (Figure 13.6).
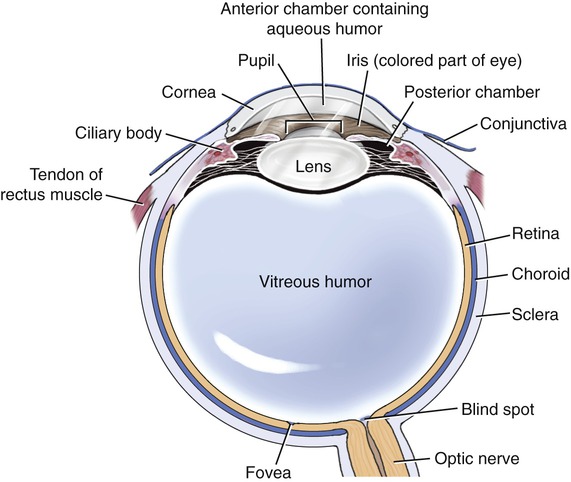
Conjunctivitis
Conjunctivitis (pink eye) can be caused by bacteria, viruses, allergies, chemicals, or a foreign object. Both the bacterial and viral forms of conjunctivitis are contagious. Because bacterial conjunctivitis is the most common type of ocular infections it is discussed in this section. Conjunctivitis is the inflammation or infection of the conjunctiva, the transparent membrane that lines the eyelid and part of the eyeball (Figure 13.7). The inflammation causes small blood vessels to become more prominent, causing the pink or red appearance of the eye. The most common symptoms of conjunctivitis include the following:
Viral Infections
Viral Meningitis
Viral meningitis is relatively common but, in contrast to bacterial meningitis, is usually not serious. Viral meningitis is called aseptic meningitis (see Table 13.1) and can be caused by any number of viruses, most of which are associated with another disease. Most often it is spread by direct contact with infected feces or nose and throat secretions. Moreover, mosquitoes can be a vector and transmit viral meningitis, usually in the summer and fall. Viral meningitis in the winter months is usually due to another underlying disease. It spreads most rapidly among young children and also in group living environments where running water is in short supply. Although anyone can get the illness, most people over 40 years of age seem to be immune.
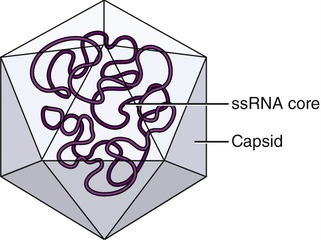
Poliomyelitis
The causative agent of poliomyelitis is the poliovirus, a small, nonenveloped, single-stranded RNA (ssRNA) virus, a human enterovirus of the family Picornaviridae (Figure 13.8). Usually poliovirus replicates within the gastrointestinal tract and is shed with the feces, and therefore it is spread from person to person via the fecal–oral route. The incubation period varies from 6 to 20 days. Approximately 95% of all infections are asymptomatic and about 4% to 8% of the infections result in a minor, nonspecific illness without clinical or laboratory evidence of central nervous system invasion. This condition is referred to as abortive poliomyelitis and complete recovery occurs in less than 1 week.
Maternal antibodies to the poliovirus do cross the placenta and provide passive immunity (see Chapter 20, The Immune System) to the infant during the first few months of life.
Rabies
Rabies is a preventable zoonotic disease caused by the rabies virus, which belongs to the order Mononegavirales, family Rhabdoviridae, and genus Lyssavirus. It is a nonsegmented, negative-sense ssRNA virus with a distinct “bullet” shape (Figure 13.9), and is capable of causing acute encephalitis in all warm-blooded hosts. Although all species of mammals are susceptible to the rabies virus, only a few species are the reservoir of distinct rabies virus variants of the disease in the United States. These variants can be detected in raccoons, skunks, foxes, and coyotes, as well as in some insectivorous bats. Rabies can also spread to domestic farm animals, groundhogs, weasels, dogs, and cats. Most animals that can be infected by the virus can also transmit the disease to humans.
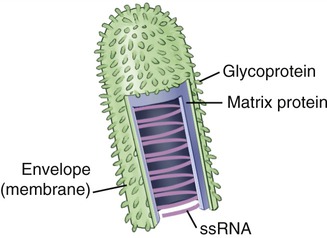
The rabies virus is a nonsegmented, negative-sense ssRNA virus with a distinct “bullet” shape.
Symptoms of rabies are usually vague but they include the following:
To prevent the spread of rabies, pet owners should do the following:
• Keep vaccinations up-to-date for all dogs, cats, ferrets, and other pets
• Keep pets under direct supervision so that they do not come in contact with wild animals
• Inform the local animal control agency to remove any stray animals from the neighborhood
• Spay or neuter pets to help reduce the number of unwanted pets, which may not be properly cared for or vaccinated on a regular basis
Arboviral Encephalitis
Arthropod-borne viruses, or arboviruses, are transmitted and maintained through biological transmission between a susceptible vertebrate host and mosquitoes, psychodids, ceratopogonids, and ticks. Vertebrate infection occurs due to arthropods that take a blood meal. Encephalitis caused by these arthropods is fairly common in the United States. Arboviruses that cause human encephalitis belong to the families Togaviridae, Flaviviridae, and Bunyaviridae (see Chapter 7, Viruses).
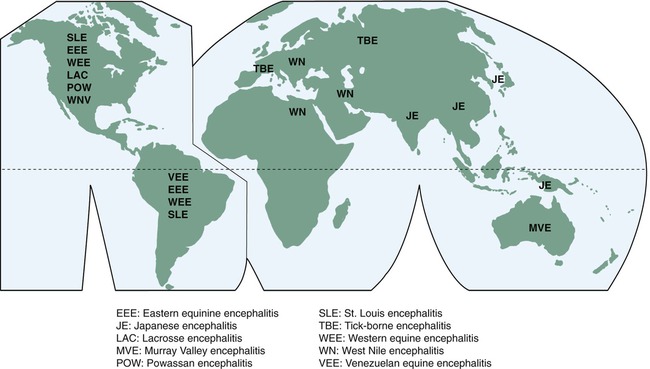
Arboviral encephalitides have a global distribution (Figure 13.10), but the viral agents currently present in the United States include the following: eastern equine encephalitis (EEE), western equine encephalitis (WEE), St. Louis encephalitis (SLE), La Crosse (LAC) encephalitis, and more recently West Nile virus (WNV) encephalitis, all transmitted via mosquitoes. WNV infects a large number of bird species such as crows and blue jays and has now spread throughout the United States.
• Eastern equine encephalitis (EEE): EEE virus is a member of the family Togaviridae, genus Alphavirus and causes illness in humans, horses, and some bird species. Transmission of the virus to humans occurs via an infected mosquito and symptoms develop 3 to 10 days after the bite occurred.
• Western equine encephalitis (WEE) is caused by an Alphavirus species, transmitted by mosquitoes. The infection can cause a range of illnesses from no symptoms to a fatal condition. Mild illness manifests itself as a headache and fever, whereas more severe disease can show the following:
• St. Louis encephalitis (SLE): The St. Louis encephalitis virus is mosquito borne, a Flavivirus species that can cause aseptic meningitis or encephalitis. The fatality rate ranges from 3% to 30%, mostly in the at-risk groups including the elderly and people with an outdoor occupation. However, the majority of infections are subclinical or a mild illness, including fever and headache. The majority of cases in the United States occur in the late summer or early fall, but in milder climates the illness can occur year round. At present no treatment or vaccine is available for the St. Louis encephalitis virus.
• La Crosse (LAC) encephalitis is a rare viral infection spread by mosquitoes and usually affects children. The infection is found primarily in the upper Midwestern United States and in the Appalachian region. The majority of infections are subclinical or result in mild illness; symptoms include nausea, headache, and vomiting and severe cases can cause seizures, coma, paralysis, and brain damage. At present no therapy is available and management of the condition is limited to treatment of the symptoms.
• West Nile virus (WNV) encephalitis is another arbovirus transmitted by mosquitoes and is common in areas such as Africa, western Asia, and the Middle East. Symptoms of infection include the following:
Protozoan Infections
Cerebral Toxoplasmosis
A pregnant woman who contracts toxoplasmosis has a more than 30% chance of passing the infection to her fetus (see Congenital Toxoplasmosis in Chapter 23, Human Age and Microorganisms). Typical symptoms are speech difficulties, seizures, confusion, and lethargy, usually over a period of days to weeks. Treatment includes the use of corticosteroids to reduce cerebral edema and a regimen of trimethoprim-sulfamethoxazole.
Prion-associated Diseases
Prion diseases or transmissible spongiform encephalopathies (TSEs) are a related group of rare, infectious, fatal, and progressive neurodegenerative diseases that affect various animals and humans. The causative agents for these diseases are believed to be prions, molecules that begin as a normal protein in animal tissue but abnormally fold and become infectious particles (see Chapter 7, Viruses). Prion diseases have a long incubation time, usually years; however, once the disease process starts they are usually rapidly progressive and always fatal. In humans, prion diseases impair brain function, causing memory changes, personality changes, dementia, and movement disorders that worsen with time. At present, there are no known ways to cure TSE diseases. Prion diseases identified to date include the following:
• Creutzfeldt-Jakob disease (CJD) is a rare, degenerative, fatal brain disorder. Symptoms generally occur around age 60 years. The only confirmed diagnosis of CJD is biopsy or autopsy. Three major categories of CJD are currently known: sporadic CJD, hereditary CJD, and acquired CJD. There is no treatment to cure or control CJD. Current treatment is to alleviate symptoms of pain and to relieve involuntary muscle movements.
• Variant Creutzfeldt-Jakob disease (vCJD) is also a rare and fatal human neurodegenerative condition and a new disease that was first described in 1996. In contrast to the traditional forms of CJD, vCJD affects younger persons with the average age of 29 years and has a longer duration of illness. It is strongly linked to exposure, and is most likely foodborne through TSE of cattle (bovine spongiform encephalopathy).
• Gerstmann-Sträussler-Scheinker syndrome (GSSS) is a particularly rare form of human TSE due to a defective gene encoding the prion protein (PRNP gene) and is identified by particular multicentric amyloid plaques (predominantly in the frontal lobe) in the brain. There is currently no treatment of the underlying pathological mechanisms of the disease.
• Fatal familial insomnia is also a rare prion disease that interferes with sleep and leads to the deterioration of mental and motor functions; death occurs within a few months to a few years. Fatal insomnia is usually inherited (autosomal dominant) or can also occur sporadically without genetic mutation. No treatment is available at this time.
• Kuru is an endemic, fatal disease among the Fore tribe of Papua New Guinea, caused by the practice of cannibalism, specifically the eating of brain tissue. As with other TSEs, kuru has a long incubation period and it might even take decades before an infected individual shows symptoms. Symptoms include headaches, joint pains, slurred speech, and shaking of the limbs, because the disease affects mainly the cerebellum (responsible for coordination).
Summary
• The nervous system is divided into the central and peripheral nervous systems and is generally protected from microbial invasion by the meninges and the blood–brain barrier. Infection of the protective CNS membranes (meninges) is referred to as meningitis; if the brain tissue itself becomes inflamed the condition is call encephalitis. A variety of microorganisms can cause one or both of these conditions.
• Meningitis manifests itself as fever, headache, and a stiff neck, followed by nausea, vomiting, confusion, sleepiness, and light sensitivity. If untreated, meningitis can lead to convulsions and coma. Bacterial meningitis is less common than viral meningitis but is generally much more severe in nature.
• Tetanus, an acute and often fatal illness, is caused by Clostridium tetani, a bacterium that produces a neurotoxin responsible for the symptoms of tetanus. On the basis of clinical findings, four different forms of tetanus are known: local tetanus, cephalic tetanus, generalized tetanus, and neonatal tetanus.
• Botulism is a rare but serious illness caused by various strains of Clostridium botulinum, which is capable of producing neurotoxins of different degrees of virulence. Botulinum toxin is one of the most poisonous naturally occurring substances known.
• Leprosy is a chronic, slowly progressive disease that affects the skin and peripheral nerves, primarily in the hands and feet. It is less communicable than most other infectious diseases.
• Poliomyelitis is an acute viral infectious disease spread from person to person, usually by the fecal–oral route. Most infections are asymptomatic but if the virus enters the central nervous system it infects and destroys motor neurons.
• Rabies is a preventable zoonotic disease capable of causing acute encephalitis in all warm-blooded hosts. Transmission begins when infected saliva enters the host, usually through a bite or scratch by an infected animal.
• Fungal infections of the nervous system are less common than bacterial or viral infections. Most fungal infections are opportunistic, capable of causing severe problems for immunocompromised persons.
• Protozoan and helminthic infections of the nervous system are acquired via bites of an arthropod, a break in the skin, or by ingestion or inhalation of contaminated materials from animal or human wastes. These infections include cerebral toxoplasmosis and trypanosomiasis.
• Prion diseases or transmissible spongiform encephalopathies (TSEs) are a related group neurodegenerative disorders caused by abnormally folded proteins, called prions.
Review Questions
1. An inflammation of the brain is called:
2. Routine vaccination against meningitis in the United States is provided against:
3. Meningococcal meningitis is caused by:
4. Otitis media is commonly caused by which microorganism?
5. The most virulent of all botulinum toxins is considered to be:
6. Hansen’s disease is also called:
7. Poliomyelitis is caused by a virus belonging to the family:
8. Which of the following is the causative agent for fungal meningitis, mostly in immunocompromised patients?
9. The organism causing West Nile encephalitis belongs to which of the following?
10. “Sleeping sickness” is caused by which type of microorganism?
11. When both the brain and the meninges are inflamed the condition is referred to as __________.
12. Pneumococcal meningitis is caused by __________.
13. African trypanosomiasis is caused by __________.
14. American trypanosomiasis is also referred to as __________ disease.
15. Chemically, prions are __________.
16. Compare and contrast bacterial and viral meningitis.
17. Elaborate on the four clinically different types of tetanus.
18. Describe the steps a pet owner should take to prevent the spread of rabies.
19. Discuss botulism, the different types of toxins, and the geographic prevalence.