Chapter 16 Indications for Endotracheal Intubation
I Introduction
Endotracheal intubation is placement of an endotracheal tube (ETT) into the trachea as a conduit for ventilation or other lung therapy. The benefits of endotracheal intubation are shown in Box 16-1. Historically, endotracheal ventilation arose as a means of resuscitation by a tracheostomy and progressed with the development of the ETT, which provided protection of the lungs from aspiration. The eventual discovery of inhalation anesthesia facilitated surgical applications requiring a secure airway, controlled ventilation, and lung therapy. This chapter reviews these primary indications for endotracheal intubation in the context of resuscitation, prehospital airway management, emergency medicine, intensive care, and anesthesiology.
II Endotracheal Intubation for Resuscitation
In 1543, Andreas Vesalius, a Belgian anatomist, was probably the first to perform endotracheal intubation by inserting a cane tube through a tracheostomy into the trachea of a pig. This landmark development allowed controlled ventilation and laid the foundation for subsequent advances in resuscitation. Endotracheal intubation for human resuscitation was first performed in 1754 by an English surgeon, Benjamin Pugh, who orally intubated an asphyxiated neonate with his air pipe. This was followed in 1788 by Charles Kite, another English surgeon, who reported the use of his curved metal cannula, which he introduced blindly into the trachea of several drowning victims from the river Thames.1
Endotracheal intubation remains the gold standard for maintaining an airway and providing ventilation in patients requiring cardiopulmonary resuscitation (CPR).2 Although alternative ventilation techniques have been successfully used, including bag-mask ventilation and supralaryngeal airway (SLA) devices, and there is no evidence to support any specific technique for airway maintenance and ventilation during CPR,2 there are many advantages of endotracheal intubation during resuscitation. Endotracheal intubation provides ventilation during continuous chest compressions without interruption,3 protection against aspiration, minimal gastric inflation, and a clear airway for effective ventilation (particularly in the presence of low lung compliance and high resistance). Disadvantages include unrecognized esophageal or endobronchial intubation,4 prolonged intubation attempts, ETT dislodgement, and hyperventilation. These problems are particularly prevalent among inexperienced practitioners.
The best airway technique for resuscitation depends on the patient’s needs and clinical circumstances, the availability of appropriate equipment, and the skill of the rescuer.2,5 Solutions to these problems involve training in airway management, appropriate selection of airway devices, and patient monitoring.
Endotracheal intubation for resuscitation of the newborn is indicated if bag-mask ventilation has been prolonged or is ineffective or if chest compressions are indicated. Care and experience is required to avoid trauma and esophageal intubation. Endotracheal intubation may also be indicated for tracheal obstruction due to meconium or other causes in nonvigorous infants when suction is required; however, routine intubation and suctioning of vigorous infants born through meconium liquor are not recommended.6,7
Drowning victims who suffer cardiopulmonary arrest require early reversal of hypoxemia and airway protection, ideally with a cuffed ETT.8 A range of ventilation techniques has been suggested for victims of drowning. Endotracheal intubation has the advantage of providing a clear secure airway with positive-pressure ventilation (PPV) in the presence of low lung compliance and high airway resistance.
Airway management for electrocution may require early endotracheal intubation if there are electric burns around the face and neck causing soft tissue edema and airway obstruction.8 Chapter 44 provides further details.
III Endotracheal Intubation for Prehospital Care
Emergency endotracheal intubation in the prehospital environment often occurs in unfavorable conditions on patients who can be critically ill with shock, cardiopulmonary arrest, traumatic brain injury (TBI), airway trauma, or uncorrected respiratory failure. There are no prospective, controlled trials comparing basic and advanced prehospital management of adult trauma patients, but the benefit of endotracheal intubation has been described in several studies.9–11 Some evidence suggests that clinical outcomes of children who have had prehospital endotracheal intubation by paramedics are no better than outcomes of children who have only received bag-mask ventilation.12 Another study of children, however, indicates that prehospital endotracheal intubation performed by a helicopter-transport medical team is safe and effective, but complications of this procedure performed by emergency medical service paramedics was unacceptably high.13
Prehospital endotracheal intubation is recommended by the international Brain Trauma Foundation guidelines for all patients with a Glasgow Coma Scale (GCS) score of 8 or less.14 Early treatment of hypoxia, normoventilation, and prevention of aspiration are associated with improved outcomes in this group of patients.10 Despite these recommendations, compliance is low, and some clinical data have shown an association between early intubation and increased mortality.15–17
The increased mortality associated with prehospital intubation may be caused by suboptimal intubation performance and hyperventilation.18 Endotracheal intubation is significantly more difficult to manage in the prehospital setting. In a study of 1106 prehospital endotracheal intubations by anesthesia-trained emergency physicians, trauma patients were more often associated with difficult airway management and failed intubation than nontrauma patients.19 In this study, the difficult airway occurred in 14.8% of prehospital intubations compared with an estimated incidence of 1% to 4% in the operating room.20 This has prompted some to suggest techniques such as SLAs or alternatives to direct laryngoscopy should be used for prehospital airway management, particularly by less experienced personnel.5,21
Controlled ventilation improves the outcome of TBI, but prehospital control of PACO2 is inconsistent. In a randomized, controlled trial of prehospital ventilated TBI patients, normoventilation occurred in only 12.9% when capnography was not used, compared with 57.5% for the monitored group.22 Although capnography is commonly used and recommended to confirm correct ETT placement and monitor mechanical ventilation, the PETCO2 is not a reliable indicator of PACO2. Arterial blood gas monitoring may improve the quality of prehospital mechanical ventilation, particularly for patients who require tight control of PACO2 or patients needing lengthy transportation.23
IV Endotracheal Intubation for Emergency Medicine
Management of the airway in the emergency department (ED) is often a fine balance between urgency and risk. The time to evaluate the patient, examine the airway, and prepare an airway plan can be limited because the patient is deteriorating or in extremis. The patient is often physiologically unstable, at risk for aspiration, uncooperative, or unconscious but in need of urgent attention. Managing the airway in the presence of a potentially unstable cervical spine is common. Medical history is often incomplete or unobtainable. Preoperative airway assessment may not be possible in the ED.24 Such risks must be tempered by the urgency of the clinical situation.
In the ED, the urgency of many clinical situations means that the benefits of endotracheal intubation outweigh the risks. The benefits of endotracheal intubation for emergency medicine patients are the same as those for elective surgical patients: provision of a secure airway, controlled ventilation, airway protection, and removal of secretions. The risks of endotracheal intubation in critically ill patients include hemodynamic instability, esophageal intubation, pneumothorax, and pulmonary aspiration.25 These risks make it essential that medical personnel, skilled in airway management and using suitable airway equipment, are available to attend the patient. Risks are heightened when airway management is required away from the operating room and when multiple endotracheal intubation attempts are made.26,27 In a study observing more than 2500 endotracheal intubation attempts outside the operating room, Mort calculated the increased relative risk for more than two intubation attempts for hypoxemia, regurgitation of gastric contents, aspiration of gastric contents, bradycardia, and cardiac arrest and showed a significant increase in these complications with repeated laryngoscopic attempts.
Urgent endotracheal intubation is indicated for a range of situations involving the trauma patient, when the airway may be at immediate or potential risk, or the patient’s medical condition requires urgent airway management. These patients may be managed with a rapid sequence induction (RSI) and endotracheal intubation. RSI with preoxygenation followed by induction of anesthesia with a potent anesthetic agent (etomidate, propofol, ketamine, or thiopentone) and a rapid- and short-acting muscle relaxant (succinylcholine) is the gold standard technique for oral endotracheal intubation in the ER. RSI has a high success rate and is the main back-up procedure when other oral or nasal intubation techniques fail and require rescue, which occurs in up to 2.7% of emergency intubations.28 The use of cricoid pressure for RSI is debatable and may compromise airway management.29,30 Urgency may be assessed clinically from signs of respiratory distress and impending fatigue (Box 16-2).
Box 16-2
Signs of Respiratory Distress and Impending Fatigue
2. Signs of sympathetic overactivity (dilated pupils, forehead sweat)
3. Dyspnea (decreased talking)
4. Use of accessory muscles (holds head off pillow)
5. Mouth opens during inspiration (licking of dry lips)
RSI is contraindicated if the patient has a mouth opening that is impossible or severely limited and in patients with intrinsic pathology of the larynx, trachea, or distal airway. This includes patients presenting with stridor after a penetrating neck injury and patients in respiratory distress with a mediastinal mass. Restricted mouth opening can result from angioedema, Ludwig’s angina, an immobile mandible, cervical spine pathology, a wired jaw, or airway distortion.31 These patients may require alternative intubation techniques and may benefit from a collaborative multidisciplinary approach to airway management.32
Awake intubation with a flexible fiberoptic bronchoscope is promoted for cooperative, stable patients with a known or suspected difficult airway.33 This technique is inappropriate in the ED for the rapidly deteriorating patient, especially when performed by inexperienced practitioners. Endotracheal intubation may also be warranted for the unstable emergency patient requiring a secure and safe airway during transfer for computed tomography or magnetic resonance imaging in the radiology department or to the intensive care unit (ICU).
V Endotracheal Intubation for Intensive Care
The most common indications for endotracheal intubation in the ICU are acute respiratory failure, shock, and neurologic disorders.34 Endotracheal intubation is indicated for controlled ventilation of a patient with refractory hypoxemia, often in the presence of multiple organ failure. Predictors of hypoxemic respiratory failure appear in Box 16-3.
Box 16-3
Predictors of Hypoxemic Respiratory Failure
1. No or minimal rise in the ratio of PaO2 to FIO2 after 1 to 2 hours
2. Patients older than 40 years
3. High acuity illness at admission (simplified acute physiology score > 35)65
4. Presence of acute respiratory distress syndrome (ARDS)
Adapted from Nava S, Hill N: Non-invasive ventilation in acute respiratory failure. Lancet 374:250–259, 2009.
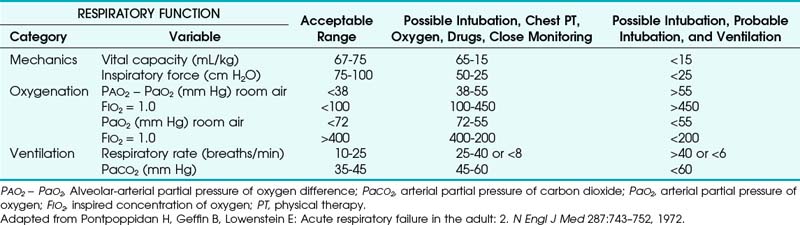
The decision to intubate is usually made on clinical grounds and based on the expected prognosis of the patient’s condition. Clinical signs (see Box 16-2) or evolving deterioration in objective criteria (Table 16-1) may support this decision.
RSI, commonly used in the ED, may not be as applicable for the unstable ICU patient. Preoxygenation of the patient with limited respiratory reserve is compromised by decreased functional residual capacity (FRC) and increased dead space.35 Commonly used induction agents can adversely affect the unstable patient. In these situations, a non-RSI technique with sedation and local anesthetic may be used.
Noninvasive ventilation techniques have become increasingly popular over the past 20 years, with development of clear indications and a range of masks and interfaces. Indications include patients with cardiogenic pulmonary edema and exacerbations of chronic obstructive pulmonary disease (COPD). Noninvasive ventilation is contraindicated for respiratory arrest or patients who are unable to be mask ventilated.36 Relative contraindications for noninvasive ventilation that favor endotracheal intubation are listed in Box 16-4.
Box 16-4
Relative Contraindications to Noninvasive Ventilation and Indications for Endotracheal Intubation
3. Unable to protect the airway
5. Excessive secretions that are not being adequately managed
6. Multiple organ failure (two or more organs)
Adapted from Nava S, Hill N: Non-invasive ventilation in acute respiratory failure. Lancet 374:250–259, 2009.
The incidence of airway mishaps in the ICU involving endotracheal intubation is relatively low. In a study of 5046 intubated ICU patients, the airway accident rate was 0.7%. Accidents were less common with ETTs than with tracheostomies.37 Self-extubation is the most common ETT accident, with rates of up to 16%. With strict clinical monitoring and in-service education, this rate can be reduced to 0.3%. After unplanned extubation, reintubation rates range from 14% to 65%.38
In addition to mechanical ventilation, endotracheal intubation facilitates other types of respiratory therapy. Patients with moderate to severe carbon monoxide poisoning benefit from 100% oxygen. This concentration of oxygen in normobaric conditions is most reliably achieved through an ETT. Other therapy through an ETT includes synthetic surfactant for premature newborns with established respiratory distress syndrome (RDS). Nitric oxide is administered to adults, infants, and neonates receiving mechanical ventilation to treat acute lung injury, acute respiratory distress syndrome (ARDS), and RDS. Heliox is a blend of oxygen and helium gas used to improve gas flow to patients with airway narrowing such as in asthma. Use of the ETT as a route for emergency drug administration during CPR is no longer recommended due to unpredictable plasma concentrations and the reliability of the intraosseous route.2
Clearing secretions by suctioning through the ETT is important to maintain ventilation by avoiding atelectasis and consolidation. Suctioning is associated with a number of complications such as hypoxemia, cardiovascular instability, elevated intracranial pressure, atelectasis, infection, and trauma to the airway. Evidence-based recommendations for endotracheal suctioning of adult intubated intensive care patients are provided in Box 16-5.39
Box 16-5
Recommendations for Endotracheal Suctioning of Intubated Adult Patients in Intensive Care
1. Suction no longer than 15 seconds.
2. Perform continuous rather than intermittent suctioning.
4. Provide hyperoxygenation before and after suctioning.
5. Provide hyperinflation combined with hyperoxygenation routinely.
Adapted from Pedersen CM, Rosendahl-Nielsen M, Hjermind J, et al: Review. Endotracheal suctioning of the adult intubated patient—What is the evidence? Intensive Crit Care Nurs 25:21–30, 2009.
VI Endotracheal Intubation for Anesthesia
Significant improvements to the design of the ETT have been historically precipitated by evolving surgical techniques. Upper airway surgery performed in the early 19th century led to an increase in postoperative pneumonia cases caused by aspiration of surgical debris. In 1878, William Macewen first used an ETT in anesthesia for a patient with a tumor of the base of the tongue.40 Macewen was also concerned with preventing aspiration, and in 1880, he developed a metal ETT with a sponge collar that he introduced blindly through the mouth for endotracheal intubation. In 1888, O’Dwyer designed a curved metal cannula with a conical end to provide a laryngeal seal. This device helped raise intratracheal pressure to avoid pulmonary collapse during thoracic surgery. In 1895, Alfred Kirstein performed awake direct laryngoscopy with the autoscope.41 This primitive instrument was the precursor of other laryngoscopes developed by Jackson and others, aiding application of the ETT. World War I precipitated a demand for plastic surgery of the head and neck, which led to oral and nasal ETT designs with pharyngeal or tracheal cuffs by Rowbotham and Magill. Anesthetic management for thoracic surgery led to the next advance in ETT design with the introduction of the first endobronchial tubes in 1932 by Gale and Waters.1 By this time, the technique of endotracheal intubation was established, prompting the statement by Macintosh that “the ability to pass an ETT under direct vision was the hallmark of a successful anesthesiology.”42
SLAs rival the oral ETT for routine airway management in the fasted elective patient. Limitations of the SLA include the inability to provide a nasal airway, the volume of the SLA in the oral cavity, and inadequate PPV due to a disrupted airway, low lung compliance, or high airway resistance. These are important considerations when choosing a suitable airway device. Second generation laryngeal masks with improved cuff seal and gastric drainage tubes have extended the application of the SLA.43 Procedures that previously were only considered suitable for endotracheal intubation such as laparoscopic surgery,44 prone position,45,46 surgery in obese patients,47,48 prolonged surgery,49 tonsillectomy,50 and craniotomy in sedated patients can now be managed with an SLA in experienced hands with close monitoring of airway quality.51 Selection of an SLA as a ventilation device should be based on case selection with careful individual patient assessment.
Safe airway management should always include a plan B for failed mask or SLA ventilation. Conversion of the airway to endotracheal intubation may occur as plan B after inadequate mask or SLA ventilation. Impossible mask ventilation during anesthesia has an incidence of 0.15% and is associated with neck changes from irradiation, male gender, sleep apnea, a Mallampati III or IV score, and the presence of a beard.52 In a study by Kheterpal of 53,041 operations that included an attempt at mask ventilation, 77 patients proved impossible to ventilate (0.15%). Of those 77 patients, 19 (25%) were also difficult to intubate, but 15 of the patients were intubated. Ultimately, 74 of the 77 impossible mask ventilation cases were intubated,52 reinforcing the value of endotracheal intubation for failed ventilation.
The American Society of Anesthesiologists (ASA) Practice Guidelines for Management of the Difficult Airway recommend awake intubation for the patient with a known difficult airway.33 This usually involves endotracheal intubation with a flexible fiberoptic bronchoscope, but other techniques have been described, including retrograde awake intubation,53 submental awake intubation,54 awake intubating LMA,55 and awake lightwand intubation.56 The outcome of each technique is a secure airway with an ETT.
Endotracheal intubation is regarded as the gold standard for protection against aspiration of gastric contents in anesthetized patients.57 However, evaluation of the cuff seal is important because of the risk of fluid draining past the cuff. This particularly applies to high-pressure, low-volume cuffs.58 Evidence evaluating the relative risk of an ETT or SLA for pulmonary aspiration is limited. An analysis of the relative risk in 65,712 procedures found that the use of an LMA was not associated with an increased risk of pulmonary aspiration compared with an ETT.59
VIII Clinical Pearls
• The best airway technique for resuscitation depends on the patient’s needs and clinical circumstances, the availability of appropriate equipment, and the skill of the rescuer.2,5
• Prehospital endotracheal intubation improves outcome for all patients with a GCS score of 8 or less, with early treatment of hypoxia, normoventilation, and prevention of aspiration, and it is recommended by the international Brain Trauma Foundation guidelines.10
• The increased mortality associated with prehospital intubation may be caused by suboptimal intubation performance and hyperventilation.18
• Elective endotracheal intubation is indicated for patients requiring anesthesia for major surgery when controlled ventilation, resuscitation, airway access, patient positioning, and duration of surgery are factors in the overall airway plan.
• SLAs rival the oral ETT for routine airway management in the fasted elective patient, but limitations of the SLA include inadequate PPV (particularly in the presence of a disrupted airway, low lung compliance, or high airway resistance), the volume of the SLA in the oral cavity, and the inability to provide a nasal airway.
• Endotracheal intubation protects against aspiration of gastric contents in anesthetized patients57; however, the use of a LMA is not associated with an increased risk of pulmonary aspiration compared with an ETT.59
• Endotracheal intubation facilitates various types of respiratory therapy, including mechanical ventilation, 100% O2 for carbon monoxide poisoning, nitric oxide, surfactant, Heliox, and suctioning.
• Risks of endotracheal intubation are heightened when airway management is required away from the operating room and when multiple endotracheal intubation attempts are made.26,27,60
• The limiting factors for the safe application of endotracheal intubation are the skill of the practitioner, the use of patient monitoring, and an understanding of the indications for endotracheal intubation. The ability to safely perform endotracheal intubation remains one of the most important skills for the airway specialist.
All references can be found online at expertconsult.com.
1 White GM. Evolution of endotracheal and endobronchial intubation. Br J Anaesth. 1960;32:235–246.
4 Timmermann A, Russo SG, Eich C, et al. The out-of-hospital esophageal and endobronchial intubations performed by emergency physicians. Anesth Analg. 2007;104:619–623.
10 Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Trauma Research and Education Foundation of San Diego. Arch Surg. 1997;132:592–597.
15 Franschman G, Peerdeman SM, Greuters S, et al. Prehospital endotracheal intubation in patients with severe traumatic brain injury: Guidelines versus reality. Resuscitation. 2009;80:1147–1151.
25 Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367–376.
34 Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Crit Care Med. 2006;34:2355–2361.
36 Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–259.
39 Pedersen CM, Rosendahl-Nielsen M, Hjermind J, et al. Endotracheal suctioning of the adult intubated patient—What is the evidence? Intensive Crit Care Nurs. 2009;25:21–30.
52 Kheterpal S, Martin L, Shanks AM, et al. Prediction and outcomes of impossible mask ventilation: A review of 50,000 anesthetics. Anesthesiology. 2009;110:891–897.
59 Bernardini A, Natalini G. Risk of pulmonary aspiration with laryngeal mask airway and tracheal tube: Analysis on 65,712 procedures with positive pressure ventilation. Anaesthesia. 2009;64:1289–1294.
1 White GM. Evolution of endotracheal and endobronchial intubation. Br J Anaesth. 1960;32:235–246.
2 Deakin CD, Nolan JP, Soar J, et al. European Resuscitation Council guidelines for resuscitation 2010: Section 4. Adult advanced life support. Resuscitation. 2010;81:1305–1352.
3 Kramer-Johansen J, Wik L, Steen PA. Advanced cardiac life support before and after tracheal intubation—Direct measurements of quality. Resuscitation. 2006;68:61–69.
4 Timmermann A, Russo SG, Eich C, et al. The out-of-hospital esophageal and endobronchial intubations performed by emergency physicians. Anesth Analg. 2007;104:619–623.
5 Timmermann A, Russo SG. Which airway should I use? Curr Opin Anaesthesiol. 2007;20:595–599.
6 Richmond S, Wyllie J. European Resuscitation Council guidelines for resuscitation 2010: Section 7. Resuscitation of babies at birth. Resuscitation. 2010;81:1389–1399.
7 Wiswell TE, Gannon CM, Jacob J, et al. Delivery room management of the apparently vigorous meconium-stained neonate: Results of the multicenter, international collaborative trial. Pediatrics. 2000;105:1–7.
8 Soar J, Perkins GD, Abbas G, et al. European Resuscitation Council guidelines for resuscitation 2010: Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation. 2010;81:1400–1433.
9 Garner A, Rashford S, Lee A, et al. Addition of physicians to paramedic helicopter services decreases blunt trauma mortality. Aust N Z J Surg. 1999;69:97–701.
10 Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Trauma Research and Education Foundation of San Diego. Arch Surg. 1997;132:592–597.
11 Davis DP, Peay J, Sise MJ, et al. Prehospital airway and ventilation management: A trauma score and injury severity score-based analysis. J Trauma. 2010;69:294–301.
12 Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA. 2000;283:783–790.
13 Gerritse BM, Draaisma JM, Schalkwijk A, et al. Should EMS-paramedics perform paediatric tracheal intubation in the field? Resuscitation. 2008;79:225–229.
14 Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24(Suppl 1):S1–S106.
15 Franschman G, Peerdeman SM, Greuters S, et al. Prehospital endotracheal intubation in patients with severe traumatic brain injury: Guidelines versus reality. Resuscitation. 2009;80:1147–1151.
16 Hesdorffer DC, Ghajar J. Marked improvement in adherence to traumatic brain injury guidelines in United States trauma centers. J Trauma. 2007;63:841–847. discussion 847–848
17 Eckstein M, Chan L, Schneir A, et al. Effect of prehospital advanced life support on outcomes of major trauma patients. J Trauma. 2000;48:643–648.
18 Davis DP. Early ventilation in traumatic brain injury. Resuscitation. 2008;76:333–340.
19 Timmermann A, Eich C, Russo SG, et al. Prehospital airway management: A prospective evaluation of anaesthesia trained emergency physicians. Resuscitation. 2006;70:179–185.
20 Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology. 1991;75:1087–1110.
21 Timmermann A, Russo SG, Crozier TA, et al. Novices ventilate and intubate quicker and safer via intubating laryngeal mask than by conventional bag-mask ventilation and laryngoscopy. Anesthesiology. 2007;107:570–576.
22 Helm M, Hauke J, Lampl L. A prospective study of the quality of pre-hospital emergency ventilation in patients with severe head injury. Br J Anaesth. 2002;88:345–349.
23 Belpomme V, Ricard-Hibon A, Devoir C, et al. Correlation of arterial PCO2 and PETCO2 in prehospital controlled ventilation. Am J Emerg Med. 2005;23:852–859.
24 Levitan RM, Everett WW, Ochroch EA. Limitations of difficult airway prediction in patients intubated in the emergency department. Ann Emerg Med. 2004;44:307–313.
25 Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367–376.
26 Mort TC. Complications of emergency tracheal intubation: immediate airway-related consequences: Part II. J Intensive Care Med. 2007;22:208–215.
27 Mort TC. Complications of emergency tracheal intubation: hemodynamic alterations: Part I. J Intensive Care Med. 2007;22:157–165.
28 Bair AE, Filbin MR, Kulkarni RG, et al. The failed intubation attempt in the emergency department: analysis of prevalence, rescue techniques, and personnel. J Emerg Med. 2002;23:131–140.
29 Brimacombe JR, Berry AM. Cricoid pressure. Can J Anaesth. 1997;44:414–425.
30 Ovassapian A, Salem MR. Sellick’s maneuver: To do or not do. Anesth Analg. 2009;109:1360–1362.
31 Levitan RM. Patient safety in emergency airway management and rapid sequence intubation: Metaphorical lessons from skydiving. Ann Emerg Med. 2003;42:81–87.
32 Mort TC. Anesthesia practice in the emergency department: overview, with a focus on airway management. Curr Opin Anaesthesiol. 2007;20:373–378.
33 American Society of Anesthesiologists. Practise guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–1277.
34 Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Crit Care Med. 2006;34:2355–2361.
35 Mort TC, Waberski BH, Clive J. Extending the preoxygenation period from 4 to 8 mins in critically ill patients undergoing emergency intubation. Crit Care Med. 2009;37:68–71.
36 Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–259.
37 Kapadia FN, Bajan KB, Raje KV. Airway accidents in intubated intensive care unit patients: An epidemiological study. Crit Care Med. 2000;28:659–664.
38 Lucas da Silva PS, de Carvalho WB. Unplanned extubation in pediatric critically ill patients: A systematic review and best practice recommendations. Pediatr Crit Care Med. 2010;11:287–294.
39 Pedersen CM, Rosendahl-Nielsen M, Hjermind J, et al. Endotracheal suctioning of the adult intubated patient—What is the evidence? Intensive Crit Care Nurs. 2009;25:21–30.
40 Macewen W. Clinical observations on the introduction of tracheal tubes by the mouth, instead of performing tracheotomy or laryngotomy. Br Med J. 1880;2:163–165.
41 Kirstein A. Autoskopie des larynx un der trachea. Berlin: Klinische Wochenschrift; 1895. pp 476–478
42 Jephcott A. The Macintosh laryngoscope. A historical note on its clinical and commercial development. Anaesthesia. 1984;39:474–479.
43 Cook TM, Lee G, Nolan JP. The ProSeal laryngeal mask airway: A review of the literature. Can J Anaesth. 2005;52:739–760.
44 Maltby JR, Beriault MT, Watson NC, et al. LMA-Classic and LMA-ProSeal are effective alternatives to endotracheal intubation for gynecologic laparoscopy. Can J Anaesth. 2003;50:71–77.
45 Abrishami A, Zilberman P, Chung F. Brief review: Airway rescue with insertion of laryngeal mask airway devices with patients in the prone position. Can J Anaesth. 2010;57:1014–1020.
46 Sharma V, Verghese C, McKenna PJ. Prospective audit on the use of the LMA-Supreme for airway management of adult patients undergoing elective orthopaedic surgery in prone position. Br J Anaesth. 2010;105:228–232.
47 Doyle DJ, Zura A, Ramachandran M, et al. Airway management in a 980-lb patient: Use of the Aintree intubation catheter. J Clin Anesth. 2007;19:367–369.
48 Zoremba M, Aust H, Eberhart L, et al. Comparison between intubation and the laryngeal mask airway in moderately obese adults. Acta Anaesthesiol Scand. 2009;53:436–442.
49 Fabregat-Lopez J, Garcia-Rojo B, Sanchez-Ferragut E, et al. Use of a ProSeal laryngeal mask airway for eight hours of unplanned abdominal surgery. Can J Anaesth. 2009;56:625–626.
50 Hatcher IS, Stack CG. Postal survey of the anaesthetic techniques used for paediatric tonsillectomy surgery. Paediatr Anaesth. 1999;9:311–315.
51 Hagberg CA, Gollas A, Berry JM. The laryngeal mask airway for awake craniotomy in the pediatric patient: report of three cases. J Clin Anesth. 2004;16:43–47.
52 Kheterpal S, Martin L, Shanks AM, et al. Prediction and outcomes of impossible mask ventilation: A review of 50,000 anesthetics. Anesthesiology. 2009;110:891–897.
53 Dhara SS. Retrograde tracheal intubation. Anaesthesia. 2009;64:1094–1104.
54 Ramsey CA, Dhaliwal SS. Retrograde and submental intubation. Atlas Oral Maxillofac Surg Clin North Am. 2010;18:61–68.
55 Ferson DZ, Rosenblatt WH, Johansen MJ, et al. Use of the intubating LMA-Fastrach in 254 patients with difficult-to-manage airways. Anesthesiology. 2001;95:1175–1181.
56 Xue FS, Yang QY, Liao X. Topical anaesthesia of the airway using Trachlight and MADgic atomizer in patients with predicted difficult tracheal intubation. Br J Anaesth. 2007;99:920–921.
57 Ng A, Smith G. Gastroesophageal reflux and aspiration of gastric contents in anesthetic practice. Anesth Analg. 2001;93:494–513.
58 Young PJ, Ridley SA. Ventilator-associated pneumonia. Diagnosis, pathogenesis and prevention. Anaesthesia. 1999;54:1183–1197.
59 Bernardini A, Natalini G. Risk of pulmonary aspiration with laryngeal mask airway and tracheal tube: Analysis on 65,712 procedures with positive pressure ventilation. Anaesthesia. 2009;64:1289–1294.
60 Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–613.
61 Cohen BM. The interrelationship of the respiratory functions of the nasal and lower airways. Bull Physiopathol Respir (Nancy). 1971;7:895–911.
62 Knelson JH, Howatt WF, DeMuth GR. The physiologic significance of grunting respiration. Pediatrics. 1969;44:393–400.
63 Mueller RE, Petty TL, Filley GF. Ventilation and arterial blood gas changes induced by pursed lips breathing. J Appl Physiol. 1970;28:784–789.
64 Schmidt RW, Wasserman K, Lillington GA. The effect of air flow and oral pressure on the mechanics of breathing in patients with asthma and emphysema. Am Rev Respir Dis. 1964;90:564–571.
65 Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–2963.