Impotence
A more descriptive term for impotence is erectile dysfunction (ED). Classically, ED has been defined as the inability to attain and maintain an erection of sufficient rigidity for sexual intercourse in at least 50% of attempts. This definition is important to consider because any normal man can have occasional ED, and treating men with only occasional symptoms is not without risk.
2. Do men with ED have disturbances in other sexual functions?
Most men with ED are able to ejaculate. Premature ejaculation may precede the development of impotence and is sometimes associated with drug therapy. Sexual desire (libido) is also usually preserved; loss of libido is suggestive of hypogonadism or severe systemic or psychiatric illness.
At least 10 million American men and perhaps as many as 20 million are impotent. Another 10 million may suffer from partial ED. The prevalence of impotence increases with age; about 2% of 40-year-old, 20% of 55-year-old, and 50% to 75% of 80-year-old men are impotent. There is a libido-potency gap in that many elderly men continue to have active libidos, but only 15% of them engage in sexual activity.
4. How does a normal erection occur?
Erection is primarily a vascular event that results from the complex interplay of the hormonal, vascular, and peripheral and central nervous systems. There is considerable psychiatric interplay in that underlying psychiatric conditions or medications can cause decreased erectile function. Conversely, undesired sexual symptoms can also adversely affect mood and self-perception.
5. Explain the role of the nervous system in achieving erection.
Erection is usually initiated by various psychological and/or physiologic stimuli in the cerebral cortex. The stimuli are modulated in the limbic system and other areas of the brain, integrated in the hypothalamus, transmitted down the spinal cord, and carried to the penis via both autonomic and sacral spinal nerves. (For the few remaining Latin scholars, these are the nervi erigentes derived from the verb erigo, erigere, erexi, erectus.) Sensory nerves from the glans of the penis enhance the message and help to maintain erection during sexual activity via a reflex arc.
6. Explain the hormonal aspects of erection.
Nervous system stimuli release neurotransmitters that reverse the tonic smooth muscle constriction maintained by norepinephrine, endothelin, and other vasoconstrictive factors. The most important of these are the potent vasodilators nitric oxide (NO) and prostaglandin E1 (PGE1). In addition to neural sources, NO is derived from endothelial cells, and this may explain why endothelial integrity may be necessary for maintenance of an erection. NO works by increasing cyclic guanosine monophosphate (cGMP) and causing a decrease in intracellular calcium. This results in relaxation of vascular smooth muscle cells secondary to dissociation of actin-myosin. The role of testosterone in erectile function remains complex and controversial. Testosterone has a critical role in stabilizing intracavernosal NO synthase, and for fully satisfactory sexual function, a “normal” quotient of testosterone must be present. Testosterone is also the main hormonal mediator of male libido; this means that deficiency can have a psychologic impact on erectile function. Regardless, some men with testosterone levels below the reference limit still have normal erections. Testosterone replacement is therefore not guaranteed to cure ED in hypogonadal men, nor is it indicated in men with normal testosterone levels but impaired sexual function.
7. What vascular changes in the penis result in erection?
Within the two spongy corpora cavernosa of the penis are millions of tiny spaces called lacunae, each lined by a wall of trabecular smooth muscle. As neurotransmitters dilate cavernosal and helicine arteries to the penis and relax the trabecular smooth muscle, the lacunar spaces in the penis become engorged with blood. This results in entrapment of outflow vessels between the expanding trabecular walls and the rigid tunica albuginea that surrounds the corpora cavernosa, thereby greatly reducing venous outflow from the penis. This venoocclusive mechanism accounts for both rigidity and tumescence. Failure of venous occlusion (venous leak) is one of the intractable causes of impotence.
8. What types of nerves and neurotransmitters play a role in penile erection?
At least three neuroeffector systems play a role in penile erection. Adrenergic nerves generally inhibit erection; cholinergic nerves and nonadrenergic, noncholinergic (NANC) substances enhance erection as follows:
 Sympathetic nerves (via beta-adrenergic receptors) constrict cavernosal and helicine arteries and contract trabecular smooth muscle.
Sympathetic nerves (via beta-adrenergic receptors) constrict cavernosal and helicine arteries and contract trabecular smooth muscle.
 Parasympathetic nerves (via cholinergic receptors) inhibit adrenergic fibers and stimulate NANC fibers.
Parasympathetic nerves (via cholinergic receptors) inhibit adrenergic fibers and stimulate NANC fibers.
 NANC messengers (NO, vasoactive intestinal polypeptide, and prostaglandins or other endothelium-derived factors) dilate cavernosal and helicine arteries and relax trabecular smooth muscle.
NANC messengers (NO, vasoactive intestinal polypeptide, and prostaglandins or other endothelium-derived factors) dilate cavernosal and helicine arteries and relax trabecular smooth muscle.
9. How does detumescence occur?
Phosphodiesterase 5 (PD5), by causing a decrease in cGMP, allows for reversal of the process (i.e., detumescence), thus making PD5 inhibitors, such as sildenafil, vardenafil, and tadalafil, important therapeutic agents for the treatment of impotence (see the following).
10. What are the common causes of impotence?
The frequency of the various causes of impotence is difficult to assess because of the large number of patients who do not report the problem, confusion regarding the diagnosis, and variability in the sophistication of the initial evaluation. Primary causes of impotence in men presenting to a medical outpatient clinic are approximated as follows:
 Endocrine factors (including hyperthyroidism and hypothyroidism): 30%
Endocrine factors (including hyperthyroidism and hypothyroidism): 30%
 Diabetes mellitus and metabolic syndrome: 15%
Diabetes mellitus and metabolic syndrome: 15%
 Systemic disease and alcoholism: 10%
Systemic disease and alcoholism: 10%
 Primary vascular causes: 5% (Alterations of blood flow are thought to play a role in many causes of impotence, but specific lesions amenable to therapy are relatively rare.)
Primary vascular causes: 5% (Alterations of blood flow are thought to play a role in many causes of impotence, but specific lesions amenable to therapy are relatively rare.)
11. What lifestyles are associated with impotence?
12. Besides diabetes mellitus, what are the three most common endocrine causes of impotence?
 Primary (hypergonadotropic) hypogonadism (increased luteinizing hormone [LH] and decreased testosterone)
Primary (hypergonadotropic) hypogonadism (increased luteinizing hormone [LH] and decreased testosterone)
 Secondary (hypogonadotropic) hypogonadism (“inappropriately” normal or actually decreased LH combined with decreased testosterone)
Secondary (hypogonadotropic) hypogonadism (“inappropriately” normal or actually decreased LH combined with decreased testosterone)
Less common causes include hyperthyroidism, hypothyroidism, adrenal insufficiency, and Cushing’s syndrome.
13. Describe the most common drugs known to induce impotence.
Nonprescription drugs, such as alcohol (as the porter says to Macduff in Act II, Scene 3 of Macbeth, “It provokes the desire but takes away the performance”), and illicit drugs, such as cocaine, methadone, and heroin, can cause impotence. The prescription drugs most commonly associated with impotence include the following:
14. Which antihypertensive agents should be used in patients with impotence?
Virtually every blood pressure medication has been associated with impotence. Although there is little overall difference in the rate of erectile problems among the commonly prescribed antihypertensive agents, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and calcium channel blockers are the agents least likely to affect erectile ability. When beta-blockade is required, selective beta-antagonists, such as atenolol or acebutolol, are preferred because they have minimal impact on sexual function.
15. What is “stuttering” impotence? What is its significance?
Impotence alternating with periods of entirely normal sexual function is termed stuttering impotence. Multiple sclerosis (MS) is the most significant organic cause of stuttering impotence. It may be the initial manifestation of MS and may be present in up to 50% of men with the disease.
16. What historical information helps to separate organic from psychogenic impotence?
True psychogenic impotence is uncommon and should be a diagnosis of exclusion. Questions that may help to separate psychogenic from organic impotence are listed in Table 45-1. A detailed history assessing for contributing physical and psychiatric conditions can also help with this distinction. These include obesity, hypertension, hyperlipidemia, atherosclerosis, diabetes mellitus or other endocrinopathy, neurologic disease, prior pelvic surgery or irradiation, trauma, Peyronie’s disease, substance abuse, depression, or the aforementioned medications. A detailed social history is also important and includes assessment of stressors and the patient’s coping mechanisms, concomitant psychosexual problems such as premature ejaculation, and relationship dynamics with partners.
TABLE 45-1.
ORGANIC VERSUS PSYCHOGENIC IMPOTENCE
| ORGANIC | PSYCHOGENIC | |
| Was onset abrupt? | No | Yes |
| Is impotence stress dependent? | No | Yes |
| Is libido preserved?* | Yes | No |
| Do you have morning erections? | No | Yes |
| Do you have orgasms? | Yes | No |
| Can you masturbate? | No | Yes |
| Does impotence occur with all partners? | Yes | No |
*There is a general relationship of libido with hypogonadal levels of testosterone in populations, but on an individual basis, libido may not be a reliable discriminator.
17. Name the essential components of a physical examination in a man complaining of impotence.
 Secondary sexual characteristics, such as muscle development, hair pattern, and presence of breast tissue
Secondary sexual characteristics, such as muscle development, hair pattern, and presence of breast tissue
 Vascular examination, especially of the femoral and lower extremity pulses and the presence of bruits
Vascular examination, especially of the femoral and lower extremity pulses and the presence of bruits
 Focused neurologic examination, including assessing the presence of peripheral neuropathy with vibratory and light touch sensation and of autonomic neuropathy using the cremasteric reflex, anal sphincter tone and/or the bulbocavernosus reflex, evaluation of standing and supine blood pressure, and measurement of the heart rate response to deep breathing and Valsalva maneuver (diabetic patients rarely have autonomic neuropathy as a cause of impotence in the absence of peripheral neuropathy)
Focused neurologic examination, including assessing the presence of peripheral neuropathy with vibratory and light touch sensation and of autonomic neuropathy using the cremasteric reflex, anal sphincter tone and/or the bulbocavernosus reflex, evaluation of standing and supine blood pressure, and measurement of the heart rate response to deep breathing and Valsalva maneuver (diabetic patients rarely have autonomic neuropathy as a cause of impotence in the absence of peripheral neuropathy)
 Examination of the genitalia to determine penile size, shape, presence of plaque or fibrous tissue (Peyronie’s disease); size and consistency of the testes; prostate examination; normal testis size is more than 5 × 3 cm or 20 mL (by orchidometer)
Examination of the genitalia to determine penile size, shape, presence of plaque or fibrous tissue (Peyronie’s disease); size and consistency of the testes; prostate examination; normal testis size is more than 5 × 3 cm or 20 mL (by orchidometer)
 Thyroid-relevant examination including size, the presence of nodularity, and abnormal reflexes
Thyroid-relevant examination including size, the presence of nodularity, and abnormal reflexes
18. What is the appropriate laboratory assessment for men with impotence?
Laboratory assessment should be based on history and physical examination findings. It can discover previously unknown disease in 6% of men. Generally, it should include the following:
19. Should prolactin levels be measured in all impotent men?
Whether serum prolactin should be measured in all men with impotence is somewhat controversial. In general, patients with normal levels of testosterone and LH and a normal neurologic examination do not require measurement of prolactin. However, if testosterone is low and associated with low or low-normal LH or if history or examination suggests a pituitary lesion, prolactin should be measured. Because prolactin interferes with the action of testosterone, prolactin status should be assessed in hypogonadal men unresponsive to testosterone replacement therapy. Hypothyroidism and renal failure also may elevate prolactin.
20. What is a penile brachial index?
Comparison of the penile and brachial systolic blood pressure allows a general assessment of the vascular integrity of the penis. This technique is not highly sensitive, but it is noninvasive and easy to perform and may help to identify men who require more extensive vascular studies. Penile systolic blood pressure obtained with Doppler ultrasound should be the same as brachial systolic pressure (i.e., ratio approximately 1.0). An index lower than 0.7 is highly suggestive of vasculogenic impotence. Diagnostic yield is increased if the penile brachial index is repeated after exercising the lower extremities for several minutes. This maneuver may uncover a pelvic steal syndrome (loss of erection resulting from pelvic thrusting) that is characterized by a difference of more than 0.15 between the resting and exercise ratios.
21. What is nocturnal penile tumescence monitoring?
Most men experience three to six erections during the night that are entrained to rapid eye movement (REM) sleep. By monitoring such events, one can assess the frequency, duration, and, with some instruments, even the rigidity of erection. This procedure helps to distinguish organic from psychogenic impotence. This can be done at home either semiquantitatively (using a Snap-Gauge) or more quantitatively (using the RigiScan).
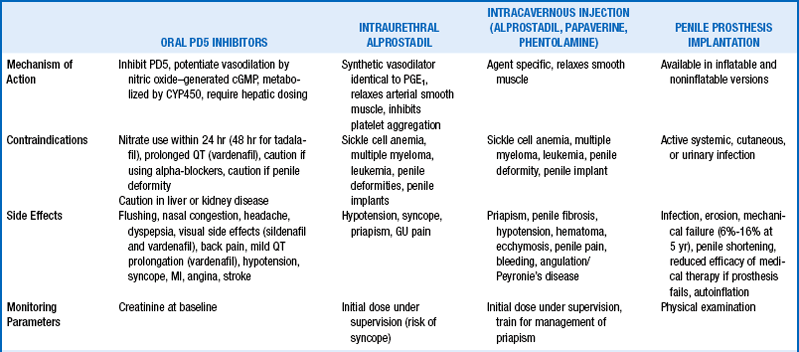
22. What are the therapeutic options in the treatment of impotence?
Once drugs with a high likelihood of causing impotence are discontinued and other underlying conditions are aggressively treated (e.g., diabetes mellitus, hypercholesterolemia), specific therapy is instituted. The broad categories of available medical and surgical therapy are summarized in Table 45-2. Important adjuncts include the following:
23. What options are available for medical treatment?
 Testosterone replacement in hypogonadal men with a goal of achieving a midnormal level of serum testosterone (see Chapter 44)
Testosterone replacement in hypogonadal men with a goal of achieving a midnormal level of serum testosterone (see Chapter 44)
 Dopamine agonists (bromocriptine or cabergoline) to reduce hyperprolactinemia in men with normal testosterone unresponsive to testosterone treatment
Dopamine agonists (bromocriptine or cabergoline) to reduce hyperprolactinemia in men with normal testosterone unresponsive to testosterone treatment
 PD5 inhibitors, such as sildenafil citrate (Viagra), vardenafil (Levitra), or tadalafil (Cialis) (Table 45-3)
PD5 inhibitors, such as sildenafil citrate (Viagra), vardenafil (Levitra), or tadalafil (Cialis) (Table 45-3)
TABLE 45-3.
COMPARISON OF PHOSPHODIESTERASE 5 INHIBITORS*
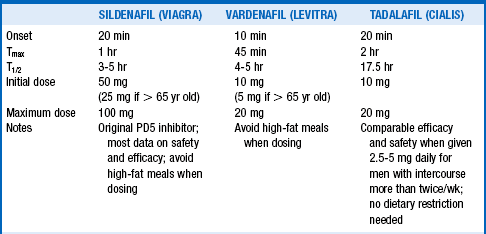
PD5, Phosphodiesterase 5; Tmax, time to maximum plasma concentration, T1/2, half-life.
*Comparative efficacy data on the three available agents are lacking. Failure of one agent is not a contraindication to trial of a different PD5 inhibitor.
 Adrenergic receptor blockers (e.g., yohimbine, 5-10 mg three times daily)
Adrenergic receptor blockers (e.g., yohimbine, 5-10 mg three times daily)
 Herbal remedies (e.g., Korean red ginseng)
Herbal remedies (e.g., Korean red ginseng)
 Selective serotonin reuptake inhibitor (SSRI) for premature ejaculation
Selective serotonin reuptake inhibitor (SSRI) for premature ejaculation
24. Summarize the role of intracavernosal injections.
Intracavernosal injection of vasoactive substances (PGE, papaverine, and phentolamine) individually or in combination (Trimix) may be effective for men in whom PD5 inhibitors have failed or are contraindicated.
25. List the surgical procedures used to treat impotence.
26. How effective are PD5 inhibitors?
The introduction of the selective PD5 inhibitors sildenafil citrate (Viagra), vardenafil (Levitra), and tadalafil (Cialis) produced a paradigm shift in the approach to the treatment of impotence by reducing the relevance of finding a specific cause of the problem. There appears to be no tachyphylaxis to their effect for at least 5 years. Given 1 hour before anticipated sexual activity (and for sildenafil and vardenafil avoiding a fatty meal, which inhibits absorption by one third), they are successful in up to 80% of men with organic impotence (although only in about 50% to 70% of diabetic men and 50% of elderly men). Newer studies indicate that once daily tadalafil may have efficacy and safety equivalent to those of “as needed” dosing. Unfortunately, well-performed comparisons of the available treatments for ED are not available. The literature on PD5 inhibitors, in particular, is limited by inconsistencies in study designs, inclusion and exclusion criteria, dosages, treatment durations, randomization, and crossover. When assessing “success” of ED therapy, it is important to consider more than the quality of the erection or the frequency of vaginal penetration because effective but invasive interventions (i.e., intracavernosal injections) are not uniformly preferred by patients. In terms of PD5 inhibitors, maximum doses are generally preferred to submaximum doses, and longer treatment durations are generally preferred to shorter durations. Younger men with a psychogenic origin of ED tend to prefer tadalafil for its greater duration of action, whereas older men with moderate or severe organic ED tend to prefer sildenafil or vardenafil for better efficacy and side effect profiles. Switching from one PD5 inhibitor to another is sometimes beneficial for nonresponders. There may also be a place for testosterone “rescue” in patients who do not respond to PD5 inhibitors and who also have low testosterone levels.
27. Discuss the side effects of PD5 inhibitors.
The few immediate side effects associated with PD5 inhibitors (headache, flushing, dyspepsia, and a blue haze in vision) rarely cause discontinuation of their use. Tadalafil causes less crossover inhibition of retinal PD6 and therefore is associated with fewer visual side effects. Because PD5 inhibitors cause vasodilatation similar to that of nitrates, they are contraindicated in men taking any form of nitrates. The long half-life of tadalafil (the so-called “weekend pill”) may prove to be particularly troublesome if a patient develops angina within 72 to 96 hours of taking the drug. Priapism may occur as a result of using PD5 inhibitors.
28. What drug interactions are associated with PD5 inhibitors?
Because PD5 inhibitors are metabolized via CYP3A4, any drugs that block that enzyme (e.g., erythromycin and other macrolide antibiotics; ketoconazole and other antifungal drugs; human immunodeficiency virus [HIV] protease inhibitors, such as saquinavir and ritonavir; and cimetidine) increase the plasma concentrations of PD5 inhibitors. In such cases, PD5 inhibitors should be started at one fourth to one half of the usual dose. Because PD5 inhibitors may potentiate the hypotensive effect of beta-adrenergic blocking agents, they should be given in lower doses (sildenafil) or not at all (vardenafil) in men taking alpha-blockers for control of blood pressure or for benign prostatic hypertrophy.
29. When are intracavernosal or intraurethral injections recommended?
Injection of vasodilatory substances directly into the corpora cavernosa of the penis should be reserved for men in whom PD5 inhibitors are ineffective, contraindicated, or limited by intolerable adverse effects. Such “PD5 salvage” therapy results in erection satisfactory for intercourse in some men with impotence. PGE1 (Caverject), papaverine, and phentolamine may be used alone or in combination (Trimix).
30. Discuss the side effects of intracavernosal and intraurethral injections.
Side effects, which depend on the types and quantities of substances injected, include hypotension, elevation of liver enzymes, and headache. Local complications include hematoma, swelling, inadvertent injection into the urethra, and local fibrosis with long-term use. The most serious local complication is priapism (a sustained erection) for more than 4 hours, which may necessitate injection of alpha-adrenergic agonists or corpora cavernosal aspiration. PGE1 is also available as an intraurethral suppository (medicated urethral system for erection [MUSE]) and, because it is less invasive and easier to use, may be a more appropriate second-line agent than intracavernosal injection. No controlled studies have evaluated the success of either approach in PD5 inhibitor failures.
31. Does the onset of impotence have other health implications?
The development of impotence is associated with a 45% increased risk of cardiovascular events. This is in the same range as other well-known risk factors such as current smoking and a family history of a myocardial infarction (MI). This association has implications on management because treatment of ED carries a 2.5-fold risk of nonfatal MI. This is comparable to having had a prior MI, after which the risk of a subsequent MI is increased 2.9-fold. The risk increase in ED treatment is probably the result of the increased level of exertion (approximately 3–4 METS) associated with intercourse. Despite these observations, the absolute risk of MI while receiving ED treatment is still extremely low (20 cases per million per hour of use) in patients with a prior MI, and so known cardiac disease is not a strict contraindication to treatment. High-risk patients, however, should be stabilized before treatment of ED:
32. What other modalities are available to treat impotent men?
Vacuum erection devices provide a noninvasive, mechanical solution for impotence. They are somewhat cumbersome to use and require the placement of an occlusive ring at the base of the penis to prevent venous outflow. They may be particularly effective in those men who have a “venous leak” as the cause of their impotence. The constrictive ring prevents antegrade ejaculation because of the urethral constriction. Surgical revascularization has a limited place in the treatment of impotent men because of its invasiveness and limited success rate. Similarly, penile prosthesis insertion is rarely done because of the availability of several effective and noninvasive alternatives. In men in whom premature ejaculation is the major problem, intermittent use of topical anesthetic agents or SSRI use has been efficacious in delaying time to ejaculation.
33. What future treatments may be forthcoming?
Newer PD5 inhibitors are in trials. In particular, avanafil is shorter acting and thus may permit use more than once a day. Taking another approach is the use of centrally acting melanocortin receptor agonists. These drugs can be administered by nasal spray and are in clinical trials. They appear to be effective alone or in combination with PD5 inhibitors. Finally, a novel use of metformin as an adjunct to sildenafil may improve ED in patients without diabetes but who have insulin resistance.
Adams, MA, Banting, BD, Maurice, DH, et al, Vascular control mechanism in penile erection. phylogeny and the inevitability of multiple overlapping systems. Int J Impotence Res 1997;9:85–95.
Andersson, K-E. Erectile physiological and pathophysiological pathways involved in erectile dysfunction. J Urol. 2003;170:S6–S14.
Bhasin, S, Cunningham, GR, Hayes, FJ, et al, Testosterone therapy in adult men with androgen deficiency syndromes. an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2006;91:1995–2010.
Bagatell, CJ, Bremner, WJ, Androgens in men. use and abuses. N Engl J Med 1997;334:707–714.
Cohan P, Korenman SG: Erectile dysfunction, J Clin Endocrinol Metab 86:2391–2394
Cookson, MS, Nadig, PW. Long-term results with vacuum constriction device. J Urol. 1993;149:290–294.
Esposito, K, Giugliano, F, Di Palo, C, et al, Effect of lifestyle changes on erectile dysfunction in obese men. a randomized controlled trial. JAMA 2004;291:2978–2984.
Esposito, K, Giugliano, F, Martedi, E, et al. High proportions of erectile dysfunction in men with the metabolic syndrome. Diabetes Care. 2005;28:1201–1203.
Feldman, HA, Goldstein, I, Hatzichristou, DJ, et al, Impotence and its medical and psychosocial correlates. results of the Massachusetts male aging study. J Urol 1994;151:54–61.
Goldstein, I, Lue, TF, Padma-Nathan, H, et al. Oral sildenafil in the treatment of erectile dysfunction. N Engl J Med. 1998;338:1397–1404.
Goldstein, I, Young, JM, Fischer, J, et al, Vardenafil, a new phosphodiesterase type 5 inhibitor, in the treatment of erectile dysfunction in men with diabetes. a multicenter double-blind placebo-controlled fixed-dose study. Diabetes Care 2003;26:777–783.
Grimm, RH, Jr., Grandits, GA, Prineas, RJ, et al, (for the TOHMS Research Group). Long-term effects on sexual function of five antihypertensive drugs and nutritional hygienic treatment in hypertensive men and women: Treatment of Mild Hypertension Study (TOHMS). Hypertension 1997;29:8–14.
Guay, A, et al, American Association of Clinical Endocrinologists medical guidelines for clinical practice for the evaluation and treatment of male sexual dysfunction. a couple’s problem–2003 update. Endocr Pract 2003;9:77–95.
Hanash, KA. Comparative results of goal oriented therapy for erectile dysfunction. J Urol. 1997;157:2135–2139.
Herrmann, HC, Chang, G, Klugherz, BD, Mahoney, PD. Hemodynamic effects of sildenafil in men with severe coronary artery disease. N Engl J Med. 2000;342:1622–1626.
Hong, G, Ji, YH, Hong, JH, et al, A double-blind crossover study evaluating the efficacy of Korean red ginseng in patients with erectile dysfunction. a preliminary report. J Urol 2002;168:2070–2073.
Krane, RJ, Goldstein, I, DeTejada, JS. Impotence. N Engl J Med. 1989;321:1648–1659.
Krassas, GE, Tziomalos, K, Papadopoulou, F, et al, Erectile dysfunction in patients with hyper- and hypothyroidism. how common and should we treat. J Clin Endocrinol Metab 2008;93:1815–1819.
Lerner, SF, Melman, A, Christ, GJ, A review of erectile dysfunction. new insights and more questions. J Urol 1993;149:1246–1252.
Linet, OI, Ogring, FG, and the Alprostadil Study Group. Efficacy and safety of intracavernosal prostaglandin in men with erectile dysfunction. N Engl J Med 1996;334:873–878.
Melman, A. Gene therapy for male erectile dysfunction. Urol Clin North Am. 2007;34:619–630.
McMahon, C. Comparison of the safety, efficacy, and tolerability of on-demand tadalafil and daily dosed tadalafil for the treatment of erectile dysfunction. J Sex Med. 2005;2:415–427.
McMahon, C, Touma, K, Treatment of premature ejaculation with paroxetine hydrochloride as needed. two single-blind placebo controlled crossover studies. J Urol 1999;161:1826–1830.
McNamara, ER, Donatucci, CF, Newer phosphodiesterase inhibitors. comparison with established agents. Urol Clin North Am 2011;38:155–163.
Montague, D, et al, The management of erectile dysfunction. an AUA update. J Urol 2005;174:230–239.
Morley, JE, Kaiser, FE, Impotence. the internists’ approach to diagnosis and treatment. Adv Intern Med 1993;38:151–168.
Mulhall, J, et al. Evaluating preference trials of oral phosphodiesterase 5 inhibitors for erectile dysfunction. Eur Urol. 2006;49:30–37.
Neisler, AW, Carey, NP. A critical reevaluation of nocturnal penile tumescence monitoring in a diagnosis of erectile dysfunction. J Nerv Ment Dis. 1990;178:78–79.
, NIH Consensus Conference. Impotence. JAMA 1993;270:83–90.
Padma-Nathan, H, Hellstrom, WSG, Kaiser, FE, [for the Medicated Urethral System for Erection (MUSE) Study Group]. Treatment of men with erectile dysfunction with transurethral alprostadil. N Engl J Med 1997;336:1–7.
Park, K, Ku, JH, Kim, SW, Paick, J-S. Risk factors in predicting a poor response to sildenafil citrate in elderly men with erectile dysfunction. BJU Int. 2005;95:366–370.
Porst, H, Padma-Nathan, H, Giuliano, F, et al, Efficacy of tadalafil for the treatment of erectile dysfunction at 24 and 36 hours after dosing. a randomized controlled trial. Urology 2003;62:121–125.
Rajfer, J, Aronson, WJ, Bush, PA, et al. Nitric oxide as a mediator of relaxation of the corpus cavernosum in response to nonadrenergic, noncholinergic neurotransmission. N Engl J Med. 1992;326:90–94.
Rendell, MS, Rajfer, J, Wicker, PA, et al, Sildenafil for treatment of erectile dysfunction in men with diabetes. a randomized controlled trial. JAMA 1999;281:421–426.
Rey Valzacchi, GR, Costanzo, PR, Finger, LA, et al, Addition of metformin to sildenafil treatment for erectile dysfunction in eugonadal non-diabetic men with insulin resistance. a prospective, randomized, double blind pilot study. J Androl 2012;19:268–272.
Rosenthal, BD, May, NR, Metro, MJ, et al. Adjunctive use of Androgel (testosterone gel) with sildenafil to treat erectile dysfunction in men with acquired androgen deficiency syndrome after failure using sildenafil alone. Urology. 2006;67:571–574.
Sidi, AA. Vasoactive intracavernous pharmacotherapy. Urol Clin North Am. 1988;15:95–101.
Thompason, IM, Tangen, CM, Goodman, PJ, et al. Erectile dysfunction and subsequent cardiovascular disease. JAMA. 2005;294:2996–3002.
Witherington, R. Mechanical aids for treatment of impotence. Clin Diabetes. 1989;7:1–22.