Chapter 171 Imaging
Trauma
Techniques for Imaging Spine Trauma
Radiographs
Alignment is well assessed with plain films. Soft tissue injury can be inferred from prevertebral soft tissue swelling in the cervical spine. In the lumbar and thoracic spine, paraspinous swelling on the AP view is a sign of acute injury. Otherwise, however, radiographs are insensitive to the detection of significant soft tissue. The sensitivity of plain films to fracture varies depending on the location of the fracture. Vertebral body fractures are usually well visualized on radiographs, but fractures in the dorsal elements can be difficult. Sensitivity of radiographs to dorsal element fractures in the cervical spine has been found to be as low as 50%.1–3 Fractures of the larger vertebrae of the thoracic and lumbar spine are usually well visualized on plain films.
Computed Tomography
CT has assumed a major role in imaging spine trauma because of the technological advances of the multidetector helical technique. It is possible to screen very rapidly for cervical spine trauma with the initial imaging evaluation of a patient with major trauma using a high-resolution technique that permits multiplanar reconstruction. Although not completely eliminated, the limitations of earlier CT technique, such as patient motion, lower resolution in reconstructed images, and relative insensitivity of CT for axially oriented fractures, are greatly diminished. Reformatted CT views in sagittal, coronal, or other planes are essential in such cases, as well as for viewing alignment. As CT increases in speed and technical capability, it has become feasible to incorporate it in a routine manner in the evaluation of major trauma, especially in cervical spine evaluation.4–7
Magnetic Resonance Imaging
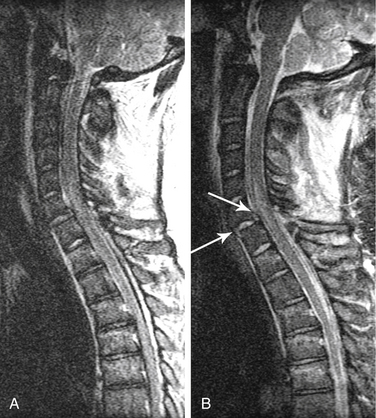
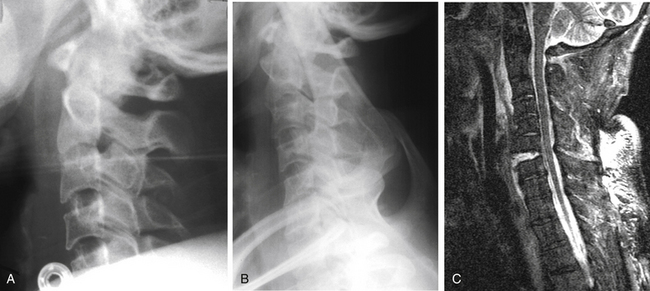
MRI is highly sensitive to soft tissues, especially for edema.8–10 MRI is the best method for visualizing the spinal cord. Compression or deformity of the spinal cord, edema, and hemorrhage are visualized well with MRI. It is also excellent for evaluating the intervertebral discs (Fig. 171-1). For example, detection of an acute disc disruption may alter plans for the surgical approach.11 Cases have been reported in which the reduction of a dislocation worsened symptoms because of further herniation or displacement of disc material. MRI permits detection of such herniation before surgery. Ligament disruption can occasionally be directly visualized with MRI, especially the anterior and posterior longitudinal ligaments. Some evidence suggests that the extent of ligament disruption may correlate with the risk of instability in cervical spine dorsal element fractures.
The soft tissues around the vertebra are also visualized with MRI. Extensive edema can serve as a marker for acute injury and the need for further evaluation. Deep, interspinous edema in the setting of acute trauma may be an indication of high risk of instability due to flexion injury. Tears or stretching of the anterior and posterior longitudinal ligaments are especially concerning for instability. MRI can be helpful in a variety of clinical situations in which the combination of clinical and initial imaging findings is ambiguous or nondefinitive. For example, degenerative changes are very common in the cervical spine and can make detection of acute fractures difficult. Although CT can help to identify fractures, subluxation or chronic deformity can still be a challenge. A negative MRI in such situations, showing no evidence of any significant nearby soft tissue edema, makes acute injury unlikely as a cause of subluxation. MRI can be especially helpful when clinical assessment is limited, such as in the obtunded or intubated patient.12
Although it is impossible to specify MRI parameters that should be used because of the great variety of manufacturers, machines, and software available, some broad principles apply. A T2-weighted sequence is important for detecting edema. Fast-spin echo imaging, in which multiple echoes are acquired during each pulse sequence, is nearly always used in standard spine imaging. Such sequences are much faster than spin echo sequences and produce excellent signal-to-noise and high-quality images. Fast-spin echo sequences can be excellent for visualizing the spinal cord, for example. However, it is important to note that fat remains very bright on such sequences, even with T2-weighting. Therefore, if adjacent soft tissue edema is to be demonstrated, different sequences must be used that suppress the signal from fat (Fig. 171-2). A fat saturation pulse can be added to fast-spin echo imaging sequences. Alternatively, inversion recovery sequences (short-tau inversion recovery [STIR]) accomplish the same effect of heavy T2 weighting and fat suppression.
Motion Radiography Studies
Radiographs of the spine in different positions (i.e., flexion and extension views in a lateral position) are excellent for evaluating the stability of the spine in a delayed or chronic setting (Fig. 171-3). Such studies have significant limitations in the acute setting, however. Most importantly, they pose major risks if the spine is in fact unstable. Complications of flexion-extension radiographs are rare but well known. If motion studies are to be undertaken, it is highly desirable that the patient be fully alert, cooperative, and capable of controlling or stopping the motion. If flexion and extension are performed on an obtunded or comatose patient, performing the study under fluoroscopy should improve the safety. The motion can be immediately stopped as soon as subluxation or abnormal movement is visualized. However, data on the safety and accuracy of performing motion radiography on an obtunded patient in the setting of acute injury are very limited. Such studies are often time-consuming, and visualization of the cervicothoracic junction is frequently difficult.
A second limitation in the acute setting is a high incidence of muscle spasm or guarding. From one quarter to one third of patients with acute cervical spine injury may have nondiagnostic results because there is inadequate movement of the neck to assess stability.13 Delayed studies, several weeks after trauma and after muscle spasm has subsided, with the patient cooperative and in control of neck motion, remain the gold standard for evaluating the stability of the cervical spine.
Imaging Findings
Cervicocranial Junction and Upper Cervical Spine
Upper cervical spine injuries can be multiple, complex, and difficult to identify on imaging.
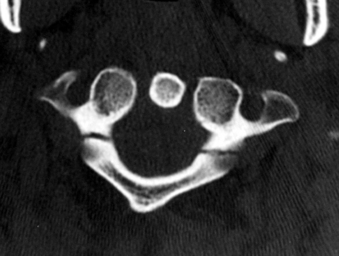
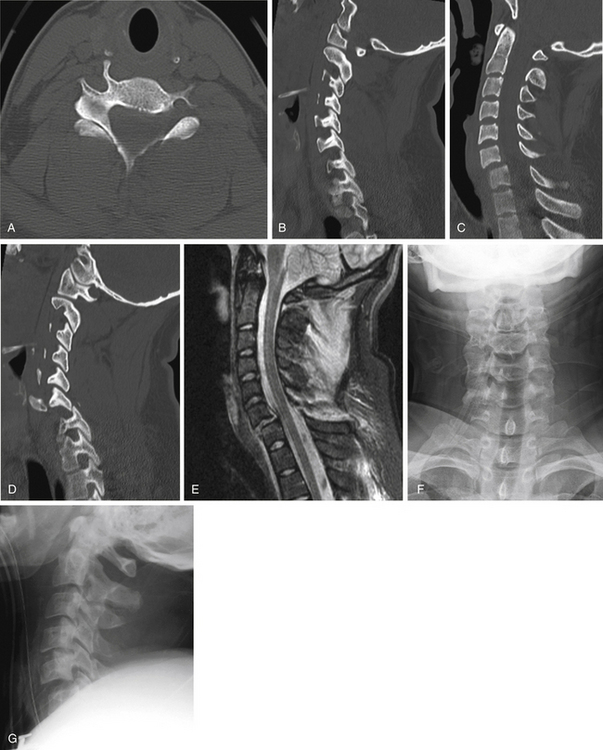
C1 Fractures
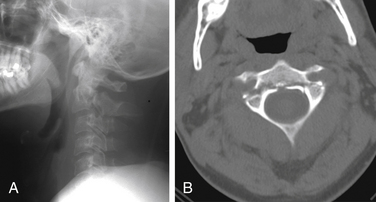
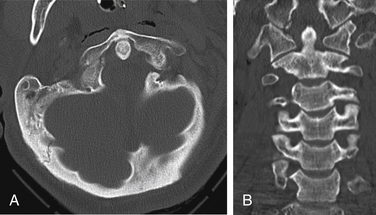
The Jefferson burst fracture of C1 is a relatively common injury. CT can demonstrate the multiple fractures of the ring of C1 and the extent of displacement (Fig. 171-4). Plain films usually show prevertebral soft tissue swelling. Some components of the fractures can be visible on plain radiographs, more so if the fractures are displaced. The lateral masses of C1 are likely to be displaced laterally if the transverse ligament is disrupted. Total displacement of greater than 7 mm as seen on an odontoid view has been suggested as a guideline to the presence of transverse ligament rupture.14 The transverse ligament can be visualized directly on MRI, and fluid signal in place of the expected low signal intensity of the ligament is evidence of rupture.15
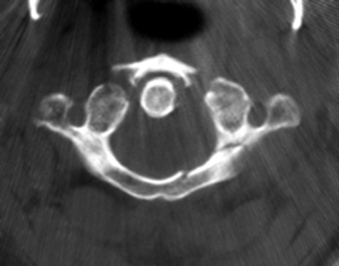
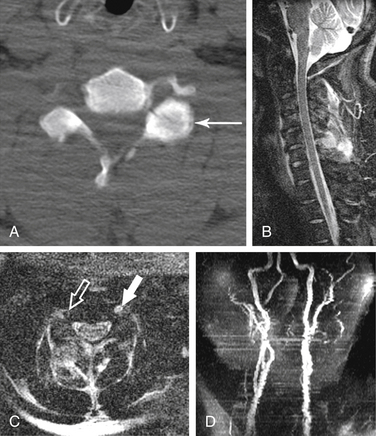
FIGURE 171-4 Jefferson fracture. Patient fell from a ladder onto the head. CT shows multiple fractures of the ring of C1.
The imaging findings just described apply to adults. In at least the first 4 years of life, the lateral masses of C1 often project lateral to the lateral margins of C2 on an AP view.16 Because Jefferson fractures are uncommon in children, CT may be necessary to demonstrate such fractures in children.
Isolated fractures of the dorsal arch of C1 can occur with hyperextension injuries (Fig. 171-5). In such cases, prevertebral soft tissue swelling would likely be absent, and the dorsal arch fracture can be seen on a lateral radiograph. Another type of hyperextension injury at C1 is an avulsion at the ventral caudal portion of the ventral arch, at the attachment of the atlantoaxial ligament. In this case, the fracture is visible on the lateral view, and focal prevertebral soft tissue swelling is usually present.
Transverse Ligament Injury
Transverse ligament rupture can be seen in association with a variety of upper cervical spine fractures, and this possibility should be considered in any such injury. In addition, transverse ligament injury uncommonly may occur without other fractures. Loss of integrity of the transverse ligament can result either from rupture in the midportion of the ligament or from avulsion of the ligament at one of the attachments to the lateral mass of C1. In the latter case, a small fracture is often visible at the tubercle where the ligament attaches (see Fig. 171-26). If the ventral atlantodental space is widened, transverse ligament rupture should be suspected. The ligament itself can be seen directly using MRI. In the case of rupture, fluid signal intensity (bright on T2-weighted images) can be seen in the expected location of the ligament, and fluid is also likely to be present between the dens and ventral arch of C1.
C2 Fractures
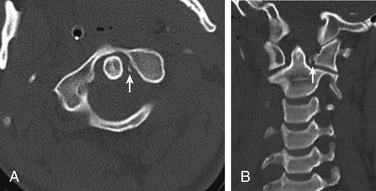
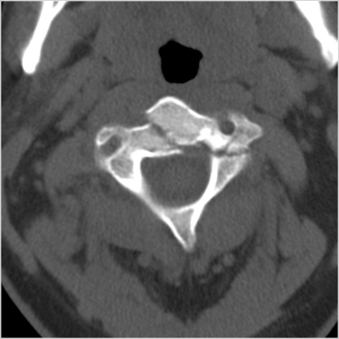
Odontoid fractures can occur from a variety of mechanisms. Anderson and D’Alonzo17 described three types of odontoid fractures: type I, an oblique fracture near the apex of the dens; type II, a transverse fracture through the lower third of the dens but above the body of C2 (Fig. 171-6); and type III, which is a fracture below the base of the dens and through the body of C2 (Fig. 171-7). As with transversely oriented fractures elsewhere, odontoid fractures can be difficult to identify by CT. Axial images may show only a region of lucency or subtle gaps in the cortical margin. Reconstructed images from thin-slice axial images, especially from rapid spiral acquisitions, can be very helpful for identifying odontoid fractures on CT. Plain radiographs should be carefully inspected for signs of odontoid fractures, including prevertebral soft tissue swelling, abnormal angulation of the odontoid process, offset of the dens with respect to the body of C2, and disruption of the cortical margin. The type III fracture (or type 3 C2 body fracture) is a horizontally oriented, rostral fracture at the base of the dens. In such fractures, the lateral radiograph shows a break in the apparent ring that results from the superimposition of densities from the junction of the pedicle and body, dens and body, and dorsal cortex of the C2 body.18 The AP or odontoid view usually shows a fracture with inferior convexity.
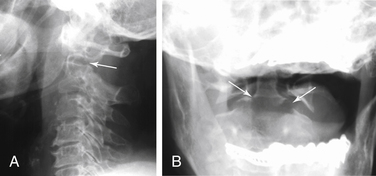
FIGURE 171-7 Low dens (type III) fracture. Motor vehicle accident patient: A, Lateral radiograph shows lucency that disrupts the ring appearance (arrow), unlike the type II fracture in Figure 171-6. B, The low fracture, actually a fracture through the rostral portion of the body of C2, is easily seen in the anteroposterior view (arrows).
Fractures of the body of C2, which have received relatively little attention, include coronally oriented dorsal fractures (type 1), which are similar in some respects to the hangman’s fracture through the pars interarticularis of C2 (Fig. 171-8); oblique, sagittally oriented fractures (type 2), which result from axial loading (Fig. 171-9)19; and the horizontally oriented type 3 fracture described earlier (see Fig. 171-7). CT is particularly helpful in defining the location and extent of fractures in C2 body fractures.
The hangman’s fracture, or traumatic spondylolisthesis, consists of bilateral fractures through the pars interarticularis (Fig. 171-10).20,21 It is usually visible on lateral radiographs as a lucency, with prevertebral soft tissue swelling. The Effendi classification of these fractures is based on the extent of displacement: type I consists of minimal displacement; type II shows ventral displacement and an abnormal C2-3 disc; and type III is ventral displacement of the body of C2 in flexion, with bilateral facet dislocation of C2-3.22
Children can suffer a unique injury of C2, fracture through the subdental synchondrosis. The dens is separated in a sharp, geometric margin from the centrum of C2 below (Fig. 171-11).
Craniocervical Junction
Occipital condyle fractures are especially difficult to identify on plain radiographs. CT with thin-slice thickness and reconstruction images is the best imaging tool (Fig. 171-12). Occipital condyle fractures have also been classified in three groups. Type I fractures are compression fractures from axial loading. Type II fractures are basilar occiput fractures that extend into the occipital condyle. Type III fractures result from avulsion, a result of lateral bending and forced rotation. Because of ligamentous injury, type III are the condyle fractures most likely to be unstable.23,24
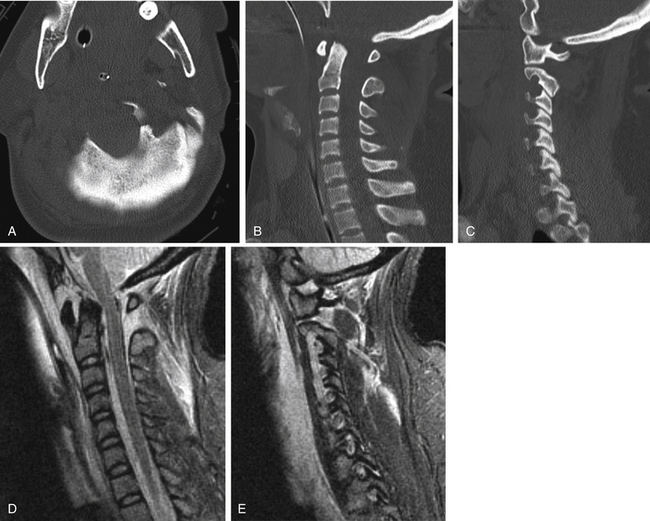
Atlanto-occipital dislocation is often a fatal injury, although less severe forms are increasingly being recognized. Prominent upper cervical prevertebral soft tissue hematoma is nearly always present (Fig. 171-13). Several methods of measuring atlanto-occipital dislocation have been proposed. The Powers ratio is the relationship of the distance from basion (B) to the dorsal arch of the atlas (C), compared with the distance from opisthion (O) to the midpoint of the dorsal surface of the ventral arch (A).25 The ratio BC/OA, which is normally less than 1, increases with ventral dislocation. The bony landmarks to determine the Powers ratio can be difficult to identify, and Harris and colleagues have described two measurements that are easier to perform and less sensitive to the direction of dislocation.26,27 Both measurements are performed on a lateral radiograph (Fig. 171-14). The first is between a dorsal axial line upward from the dorsal vertebral body of C2 and the basion. The basion-axial interval should be no less than 6 mm or more than 12 mm, in both adults and children. The second measurement is between the basion and the tip of the dens, the basion-dens interval. This distance should not be more than 12 mm. This basion-dens interval depends on complete ossification of the dens and therefore may not be obtainable in children younger than 13 years. Evaluation with multidetector CT is somewhat different.28 The normal basion-dens interval is less than 8.5 mm in 95% of the normal adult population. The basion-axial interval is less reliable and useful on CT. The atlanto-occipital interval, or distance between the occipital condyle and C1 lateral mass at the midpoint of the joint, should be less than 1.5 mm. The relationship between the condyle and C1 lateral mass is readily assessed on parasagittal CT reconstructions and should be evaluated routinely (see Fig. 171-13C).
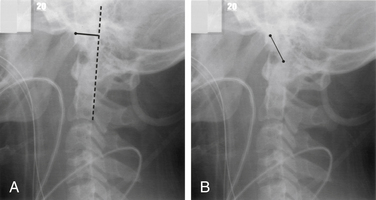
FIGURE 171-14 Craniocervical relationships and atlanto-occipital dissociation (AOD). Lateral radiograph of a patient who suffered AOD shows severe prevertebral soft tissue swelling and distraction of the cranium from the spine. Measurements described by Harris et al.26,27 are illustrated: A, Basion-axial interval, distance from basion to a line extended upward from the dorsal margin of the body of C2. B, Basion-dens interval, distance from basion to the tip of the dens.
(Copyright 2001, University of New Mexico Department of Radiology, Neuroradiology Section.)
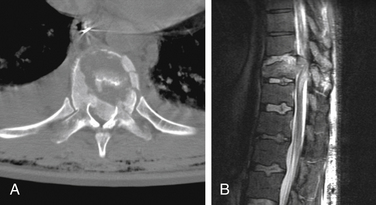
Subaxial Cervical Spine Injuries
Axial loading injuries in the lower cervical spine result in burst fractures. The basic pattern of the burst fracture is similar throughout the thoracic and lumbar spine, as well. The degree of comminution is variable, but there is usually a prominent sagittal component. Dorsal element fractures are common and variable. CT is very helpful in determining the extent of fractures (Fig. 171-15). Involvement of multiple vertebrae can occur with more severe injuries. MRI can directly demonstrate the relationship of displaced bone to the spinal cord, spinal cord compression, and spinal cord edema and hematoma, as well as disc disruption.
A variety of flexion injuries can occur in the subaxial cervical spine. Many of these injuries result in a pattern of dorsal widening or fanning of the facets and spinous processes at the level of injury (Fig. 171-16). This pattern of flexion injury is an important finding on lateral radiographs. Dorsal ligament injury without fracture can result in instability from flexion sprain. A simple ventral compression fracture results in loss of ventral height of a vertebral body. Dorsal ligament injury may or may not accompany a compression fracture. Focal kyphosis is often observed at the level of compression.29–31A fairly common pattern of flexion injury in the lower cervical spine is an avulsion fracture of the spinous process, or “clay-shoveler’s fracture.”
More serious flexion injuries can cause actual disruption of the facet joints and bilateral facet dislocation (Fig. 171-17). The vertebra above the level of dislocation is ventrally displaced relative to the vertebra below the level of dislocation. Dorsal widening and focal kyphosis are observed. CT often reveals small fractures of the articular processes at the level of dislocation. MRI shows a typical pattern of extensive dorsal soft tissue edema from the level of dislocation and above; and the relationship of the spinal cord to the narrowed spinal canal can be seen on MRI.
A flexion teardrop fracture is one of the most severe flexion injuries of the cervical spine. Lateral radiographs show a large triangular fragment of bone from the ventral caudal corner of the fractured vertebra. Unlike the extension teardrop fracture, there is pronounced flexion of the spine at the level of injury. The typical clinical picture of anterior cord syndrome also distinguishes the flexion teardrop fracture.32
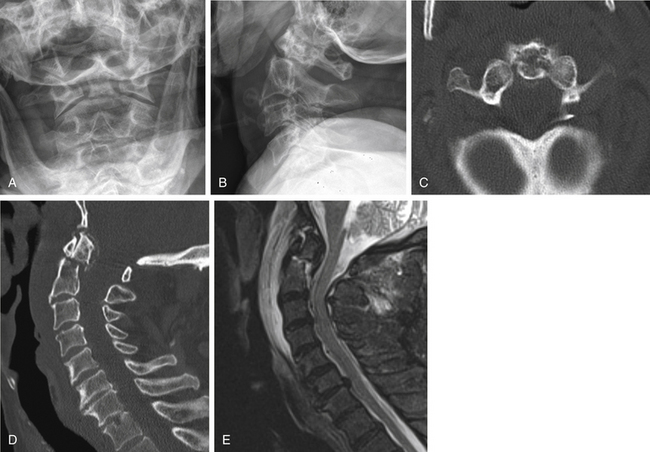
Hyperextension dislocation causes transient dislocation through a disc level and compression of the spinal cord. The usual clinical picture is a central cord syndrome. Radiographic signs are straightening of the cervical spine, diffuse prevertebral swelling, and often an avulsion fracture of the inferior end plate above the level of dislocation (Fig. 171-18). Such a fracture is horizontally oriented and is wider than it is tall. Disc space widening or gas within the disc space is less commonly seen.33,34 MRI shows the prevertebral edema, abnormal signal in the affected disc space, and edema within the spinal cord. In the author’s experience, MRI also often shows dorsal soft tissue edema. Another cause of central cord syndrome resulting from hyperextension was described by Taylor et al.35,36 In such cases, preexisting osteophytes narrow the spinal canal and cause transient spinal cord compression. Diffuse prevertebral soft tissue swelling is lacking in such cases, but MRI shows edema within the spinal cord and the extent of spondylosis (Fig. 171-19).
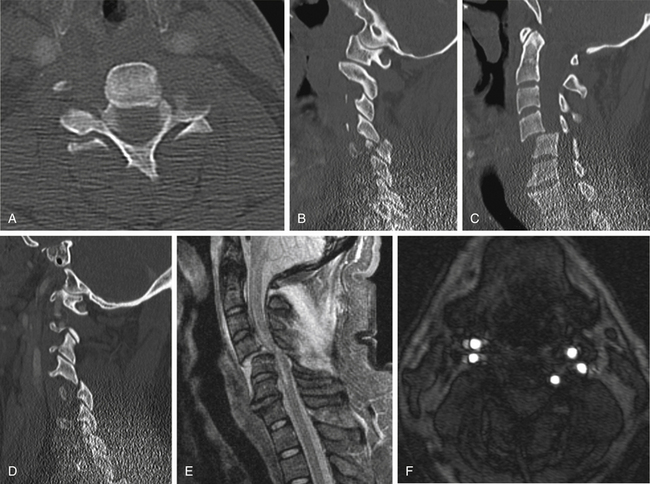
Unilateral facet dislocation results from combined flexion and rotation. Such cases have a typical constellation of imaging findings (Fig. 171-20).37,38 Lateral radiographs show an abrupt change from a typical lateral appearance below the dislocation to an appearance above that level of an oblique projection. The visualization of both facets on the lateral view just above the dislocation gives a “bow-tie” appearance. On the AP view, there is an abrupt change in the line along the spinous processes. CT shows a reversal of the usual “clamshell” appearance of the facets where they are dislocated. In less severe cases, the facets may appear “perched” without frank dislocation, but this finding still implies major ligament and joint disruption.
Fractures involving the lateral masses, pedicles, and laminae can be very difficult to visualize on plain films. Close inspection of the lateral bony margins seen on AP views can show irregularity or overlap in some cases. If there is more extensive ligament injury and displacement, there may be rotational displacement that can simulate a unilateral facet dislocation on plain films. However, CT clearly demonstrates the location of fractures (Fig. 171-21). Fractures of both pedicle and lamina result in separation of the articular mass from the vertebral body and potential instability. MRI can be helpful in determining the extent of ligamentous injury, which may help predict the risk of instability.39
Identification of a fracture should not terminate the evaluation of the entire cervical spine.
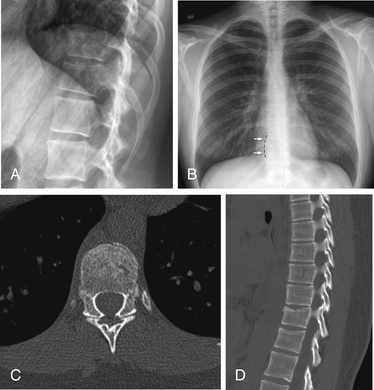
Thoracic and Lumbar Spine
Indications for screening of the thoracic and lumbar spine in the setting of blunt trauma are not as clear-cut as in the cervical spine.40,41 In the trauma patient with back pain, a good starting point for evaluation of thoracolumbar trauma is high-quality AP and lateral radiographs. However, if the patient is already getting chest/abdominal CT imaging, reconstructed axial bone windows with high-quality sagittal and coronal reformats are superior to plain radiography for the exclusion of trauma. In most cases, it suffices to obtain plain radiographs to screen the thoracolumbar spine in the obtunded or intoxicated patient and in the patient with unreliable clinical examinations.40 Dedicated CT imaging of the thoracolumbar spine is usually reserved for patients with significant plain radiographic abnormalities, usually as a part of presurgical planning. In the setting of neurologic deficits, MRI is often indicated to exclude entities such as direct spinal cord injury, traumatic disc herniation, or epidural hematoma. In contrast to the cervical spine, MRI is not usually needed to exclude ligamentous injury if there is no associated fracture of the spine.
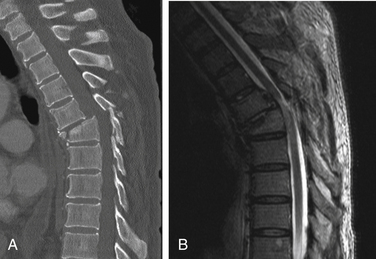
Along with more restricted movement in the thoracic and lumbar spine than in the cervical region, there exist fewer patterns of fracture. Compression fractures and burst fractures have features similar to those described for the cervical spine. Prevertebral soft tissue swelling is not a very useful plain film finding below the cervical spine, but paraspinal soft tissue hematoma can be visible on AP views, especially in the thoracic spine. With compression fractures, ventral loss of height and buckling of the superior end plate and ventral cortical margin occur (Fig. 171-22). In more severe cases, some dorsal buckling of the vertebral body is observed. There is usually focal kyphotic angulation. Mild compression fractures are often more obvious on lateral radiographs than on CT. CT may show only subtle lucency along the ventral, superior margin of the vertebral body in mild fractures. MRI or bone scan can be helpful in resolving any uncertainty about whether a fracture is acute or chronic. Edema will be seen in the marrow space on MRI in acute fractures; after a period of weeks to months, the marrow signal intensity returns to that similar to adjacent, normal marrow.
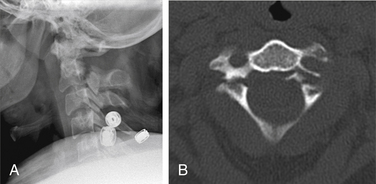
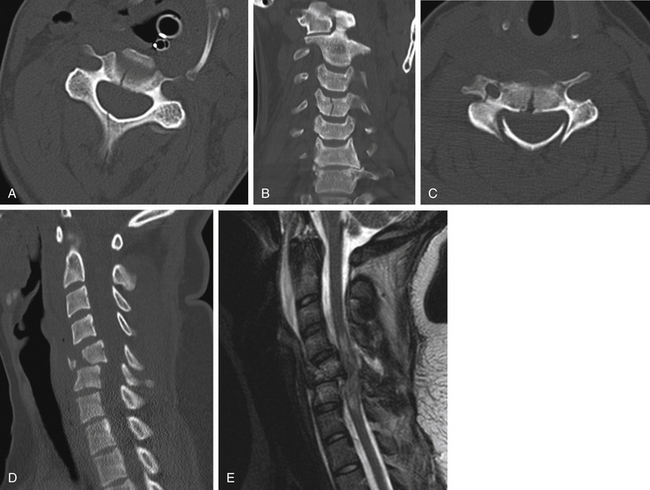
Burst fractures are usually visible on plain films, but CT can much more fully characterize the vertebral body fractures, degree of comminution and displacement, and dorsal element fractures (Fig. 171-23). Fractures of adjacent vertebrae are common, so CT should include enough of the nearby spine to ensure that all fractures near the obvious injury have been detected. This is of obvious value in planning instrumentation. MRI yields additional information about the integrity (or loss thereof) of discs and major ligaments as well as spinal cord damage.
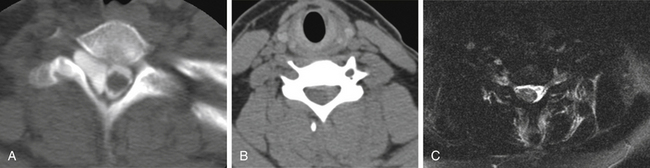
Chance-type injuries are characterized by dorsal distraction in combination with flexion. The most common locations are around the thoracolumbar junction. The classic fracture described by Chance extends in a horizontal plane through a vertebral body into the pedicles (Fig. 171-24).42 These fractures are often more easily appreciated on lateral radiographs than on the axial CT images. Since the fractures lie in the plane of imaging, axial images may be notable only for an absence of bone rather than distinct fracture lines. Sagittal and coronal reconstruction images show the fractures on CT more clearly than the axial images. However, the category of Chance-type injuries has been broadened to include other injuries that result from a similar mechanism.43,44 Thus, the horizontally oriented disruption can also occur through an intervertebral disc, and the plane of dorsal distraction then typically extends through the facet joints. In any of these patterns, MRI demonstrates localized injury through the dorsal elements and soft tissues. In addition, a Chance injury should always suggest the possibility of associated abdominal injuries. Solid organ lacerations and perforations are present in up to half of patients with Chance-type injuries.
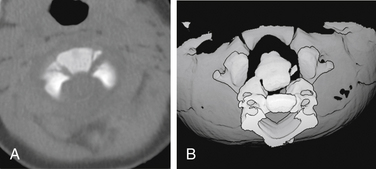
Fracture-dislocation of the thoracic or lumbar spine is the result of very severe injury mechanisms and carries a high risk of spinal cord injury. CT is especially helpful in such cases, and MRI is often also beneficial in evaluating the spinal cord (Fig. 171-25). As shown in Figure 171-26, CT is also helpful in evaluating ligament avulsion.
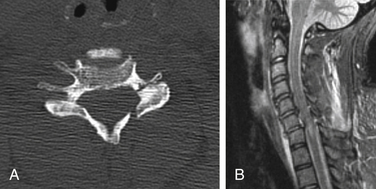
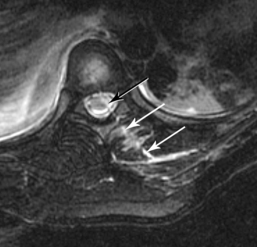
Nerve Root Injuries
Traction injuries can cause damage to the brachial plexus and/or avulsion of cervical nerve roots as they exit the spinal canal. MRI is especially helpful when such injuries are suspected. Imaging findings include absence of the nerve root in the foramen or lateral recess, a fluid collection (pseudomeningocele) in or lateral to the foramen, and displacement of the thecal sac to the opposite side. Myelography or CT can also demonstrate some of these findings (Fig. 171-27). The imaging findings, especially for fluid collections, are likely to evolve over time.
Penetrating Injuries
Plain films may be useful initially in assessing the location of bullet fragments. Once the level of injury is determined from the penetrating injury, CT is especially helpful for evaluating the precise nature of bone injuries and possible involvement of the spinal canal. After it is clear that no contraindications are present, such as metal in the spinal canal, MRI can be used to visualize the spinal cord and possible hematomas (Fig. 171-28).
Vascular Injuries
Vertebral artery injuries, ranging from intimal injury, dissection, and frank occlusion, are fairly common in cases of cervical spine injury, especially with fractures of the dorsal elements that involve the foramen transversarium. CT angiography can be obtained rapidly with multidetector CT (often during simultaneous acquisition of cervical spine CT) with multiplanar reconstructions possible. Magnetic resonance angiography (MRA) may be useful in some cases, especially if MRI is already being obtained. Routine axial MRI, for example, shows lack of signal (“flow void”) in normal arteries. The normal black appearance of the artery is replaced by intermediate or high-signal intensity when there is no flow. Slow blood flow in an artery may give a similar appearance. MRA is a very useful tool for noninvasively evaluating normal and abnormal arteries in trauma patients. Axial MRIs and axial source images from MRA may also demonstrate a flap in cases of dissection or blood in the false lumen (Fig. 171-29). Catheter angiography is needed less often than in the past.
Spinal Cord Injury without Radiographic Abnormality
Spinal cord injury without radiographic abnormality (SCIWORA) can occur from a variety of mechanisms that result in neurologic injury without fractures. The term dates from earlier reliance on radiographs; MRI nearly always demonstrates imaging abnormalities when neurologic deficits occur.45 Postulated mechanisms include flexion, transient distraction, compression of the spinal cord, and ischemia.
Benzel E.C., Hart B.L., Ball P.A., et al. Magnetic resonance imaging for the evaluation of patients with occult cervical spine injury. J Neurosurg. 1996;85(5):824-829.
Como J.J., Diaz J.J., Dunham C.M., et al. Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. J Trauma.. 2009;67(3):651-659.
Diaz J.J.Jr., Cullinane D.C., Altman D.T., et al. Practice management guidelines for the screening of thoracolumbar spine fracture. J Trauma. 2007;63(3):709-718.
Hanson J.A., Blackmore C.C., Mann F.A., et al. Cervical spine injury: a clinical decision rule to identify high-risk patients for helical CT screening. AJR Am J Roentgenol. 2000;174(3):713-717.
Rojas C.A., Bertozzi J.C., Martinez C.R., et al. Reassessment of the craniocervical junction: normal values on CT. AJNR Am J Neuroradiol. 2007;28(9):1819-1823.
1. Acheson M.B., Livingston R.R., Richardson M.L., Stimac G.K. High-resolution CT scanning in the evaluation of cervical spine fractures: comparison with plain film examinations. AJR Am J Roentgenol. 1987;148(6):1179-1185.
2. Woodring J.H., Lee C. The role and limitations of computed tomographic scanning in the evaluation of cervical trauma. J Trauma. 1992;33(5):698-708.
3. Woodring J.H., Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma. 1993;34(1):32-39.
4. Griffen M.M., Frykberg E.R., Kerwin A.J., et al. Radiographic clearance of blunt cervical spine injury: plain radiograph or computed tomography scan? J Trauma. 2003;55(2):222-226. discussion 226–227
5. Hanson J.A., Blackmore C.C., Mann F.A., Wilson A.J. Cervical spine injury: a clinical decision rule to identify high-risk patients for helical CT screening. AJR Am J Roentgenol. 2000;174(3):713-717.
6. Nunez D.B.Jr., Zuluaga A., Fuentes-Bernardo D.A., et al. Cervical spine trauma: how much more do we learn by routinely using helical CT? Radiographics. 1996;16(6):1307-1318. discussion 1318–1321
7. Como J.J., Diaz J.J., Dunham C.M., et al. Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. J Trauma. 2009;67(3):651-659.
8. Chakeres D.W., Flickinger F., Bresnahan J.C., et al. MR imaging of acute spinal cord trauma. AJNR Am J Neuroradiol. 1987;8(1):5-10.
9. Mirvis S.E., Geisler F.H., Jelinek J.J., et al. Acute cervical spine trauma: evaluation with 1.5-T MR imaging. Radiology. 1988;166(3):807-816.
10. Orrison W.W., Benzel E.C., Willis R.K., et al. Magnetic resonance imaging evaluation of acute spine trauma. Emerg Radiol. 1995;2(3):120-128.
11. Rizzolo S.J., Piazza M.R., Cotler J.M., et al. Intervertebral disc injury complicating cervical spine trauma. Spine (Phila Pa 1976). 1991;16(Suppl 6):S187-S189.
12. Benzel E.C., Hart B.L., Ball P.A., et al. Magnetic resonance imaging for the evaluation of patients with occult cervical spine injury. J Neurosurg. 1996;85(5):824-829.
13. Bohrer S.P., Chen Y.M., Sayers D.G. Cervical spine flexion patterns. Skeletal Radiol. 1990;19(7):521-525.
14. Spence K.F.Jr., Decker S., Sell K.W. Bursting atlantal fracture associated with rupture of the transverse ligament. J Bone Joint Surg [Am]. 1970;52(3):543-549.
15. Dickman C.A., Mamourian A., Sonntag V.K., Drayer B.P. Magnetic resonance imaging of the transverse atlantal ligament for the evaluation of atlantoaxial instability. J Neurosurg. 1991;75(2):221-227.
16. Suss R.A., Zimmerman R.D., Leeds N.E. Pseudospread of the atlas: false sign of Jefferson fracture in young children. AJR Am J Roentgenol. 1983;140(6):1079-1082.
17. Anderson L.D., D’Alonzo R.T. Fractures of the odontoid process of the axis. J Bone Joint Surg [Am]. 1974;56(8):1663-1674.
18. Harris J.H.Jr., Burke J.T., Ray R.D., et al. Low (type III) odontoid fracture: a new radiographic sign. Radiology. 1984;153(2):353-356.
19. Benzel E.C., Hart B.L., Ball P.A., et al. Fractures of the C-2 vertebral body. J Neurosurg. 1994;81(2):206-212.
20. Brashear R.Jr., Venters G., Preston E.T. Fractures of the neural arch of the axis. A report of twenty-nine cases. J Bone Joint Surg [Am]. 1975;57(7):879-887.
21. Francis W.R., Fielding J.W., Hawkins R.J., et al. Traumatic spondylolisthesis of the axis. J Bone Joint Surg [Br]. 1981;63(3):313-318.
22. Effendi B., Roy D., Cornish B., et al. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg [Br]. 1981;63(3):319-327.
23. Bettini N., Malaguti M.C., Sintini M., Monti C. Fractures of the occipital condyles: report of four cases and review of the literature. Skeletal Radiol. 1993;22(3):187-190.
24. Clayman D.A., Sykes C.H., Vines F.S. Occipital condyle fractures: clinical presentation and radiologic detection. AJNR Am J Neuroradiol. 1994;15(7):1309-1315.
25. Powers B., Miller M.D., Kramer R.S., et al. Traumatic anterior atlanto-occipital dislocation. Neurosurgery. 1979;4(1):12-17.
26. Harris J.H.Jr., Carson G.C., Wagner L.K. Radiologic diagnosis of traumatic occipitovertebral dissociation: 1. Normal occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol. 1994;162(4):881-886.
27. Harris J.H.Jr., Carson G.C., Wagner L.K., Kerr N. Radiologic diagnosis of traumatic occipitovertebral dissociation: 2. Comparison of three methods of detecting occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol. 1994;162(4):887-892.
28. Rojas C.A., Bertozzi J.C., Martinez C.R., Whitlow J. Reassessment of the craniocervical junction: normal values on CT. AJNR Am J Neuroradiol. 2007;28(9):1819-1823.
29. Green J.D., Harle T.S., Harris J.H.Jr. Anterior subluxation of the cervical spine: hyperflexion sprain. AJNR Am J Neuroradiol. 1981;2(3):243-250.
30. Harris J.H.Jr., Yeakley J.S. Radiographically subtle soft tissue injuries of the cervical spine. Curr Probl Diagn Radiol. 1989;18(4):161-190.
31. Scher A.T. Anterior cervical subluxation: an unstable position. AJR Am J Roentgenol. 1979;133(2):275-280.
32. Kahn E.A., Schneider R.C. Chronic neurological sequelae of acute trauma to the spine and spinal cord. I. The significance of the acute-flexion or tear-drop fracture-dislocation of the cervical spine. J Bone Joint Surg [Am]. 1956;38(5):985-997.
33. Edeiken-Monroe B., Wagner L.K., Harris J.H.Jr. Hyperextension dislocation of the cervical spine. AJR Am J Roentgenol. 1986;146(4):803-808.
34. Harris J.H., Yeakley J.W. Hyperextension-dislocation of the cervical spine. Ligament injuries demonstrated by magnetic resonance imaging. J Bone Joint Surg [Br]. 1992;74(4):567-570.
35. Taylor A.R. The mechanism of injury to the spinal cord in the neck without damage to vertebral column. J Bone Joint Surg [Br]. 1951;33(4):543-547.
36. Borovich B., Peyser E., Gruskiewicz J. Acute central and intermediate cervical cord injury. Neurochirurgia (Stuttg). 1978;21(3):77-84.
37. Braakman R., Vinken P.J. Unilateral facet interlocking in the lower cervical spine. J Bone Joint Surg [Br]. 1967;49(2):249-257.
38. Young J.W., Resnik C.S., DeCandido P., Mirvis S.E. The laminar space in the diagnosis of rotational flexion injuries of the cervical spine. AJR Am J Roentgenol. 1989;152(1):103-107.
39. Halliday A.L., Henderson B.R., Hart B.L., Benzel E.C. The management of unilateral lateral mass/facet fractures of the subaxial cervical spine: the use of magnetic resonance imaging to predict instability. Spine (Phila Pa 1976). 1997;22(22):2614-2621.
40. Diaz J.J.Jr., Cullinane D.C., Altman D.T., et al. Practice management guidelines for the screening of thoracolumbar spine fracture. J Trauma. 2007;63(3):709-718.
41. O’Connor E., Walsham J. Review article: indications for thoracolumbar imaging in blunt trauma patients: a review of current literature. Emerg Med Australas. 2009;21(2):94-101.
42. Chance G.Q. Note on a type of flexion fracture of the spine. Br J Radiol. 1948;21(249):452.
43. Gertzbein S.D., Court-Brown C.M. Flexion-distraction injuries of the lumbar spine. Mechanisms of injury and classification. Clin Orthop Relat Res. 1988;227:52-60.
44. Smith W.S., Kaufer H. Patterns and mechanisms of lumbar injuries associated with lap seat belts. J Bone Joint Surg [Am]. 1969;51(2):239-254.
45. Matsumura A., Meguro K., Tsurushima H., et al. Magnetic resonance imaging of spinal cord injury without radiologic abnormality. Surg Neurol. 1990;33(4):281-283.