CHAPTER 12 Imaging of the Pediatric Elbow
INTRODUCTION
Tomography, using either a simple linear method or a complex motion system, can be used in the evaluation of growth plates that have closed prematurely following trauma. In most practices, computed tomography has completely replaced conventional tomography. Computed tomography examinations now take only seconds to perform, and sedation is usually not necessary, even in very young infants and children. Using current 64-slice multidetector computed tomography technology (MDCT), isovoxel images can be obtained in all three planes down to 0.6-mm collimation. This allows detailed imaging, with the bony trabecular pattern well seen. Examinations are obtained with the patient in the prone position, with the affected arm held above the head with about 90 degrees of flexion at the elbow. Sagittal and coronal two-dimensional reformatted images as well as three-dimensional reconstructions are then made from the raw data. MDCT is a sensitive (92%) and specific (79%) method of evaluating for radiographically occult elbow fractures.6 MDCT can also use automated tube current modulation to markedly decrease the radiation dose to the patient compared with fixed-tube current techniques. MDCT can also be performed with no image degradation through a cast.3 MDCT with reformatting can better delineate intra-articular fractures (Fig. 12-1). Three-dimensional imaging can also provide additional information and help define the joint relationships to aid surgical planning (Figs. 12-2 and 12-3). The resulting three-dimensional image can be rotated in all planes with computerized subtraction of the adjacent soft tissues and bones, if needed.
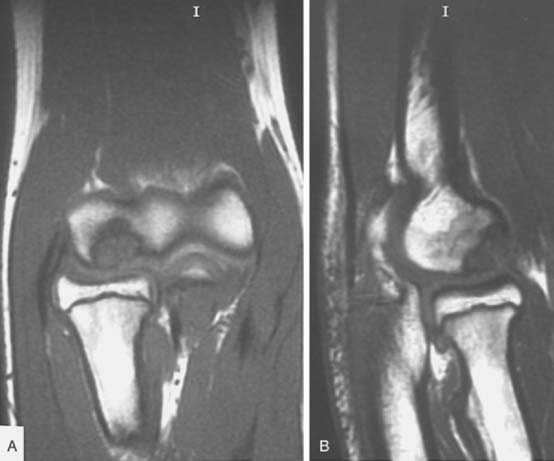
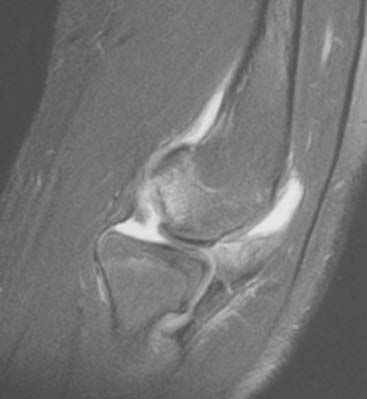
Magnetic resonance imaging (MRI) and ultrasonography are increasingly being used to evaluate the elbow. MRI can evaluate cartilage, bone marrow, and soft tissue structures (Fig. 12-4).8 Radiographs do not show bone bruising, or cartilaginous or soft tissue injury and can underestimate physeal injury. MRI is also occasionally used to better define elbow fractures.2 Owing to the length of the MRI examination (at least 20 minutes), children younger than 5 years old will usually need sedation so that optimal MRI images can be obtained. In children with elbow trauma, MRI reveals a broad spectrum of bone and soft tissue injury, including ligamentous injury, beyond that recognized by radiographs. However, the additional information afforded by MRI usually does not change treatment or clinical outcome in acute elbow trauma.9 MRI can be very useful in the evaluation of osteochondritis dissecans (OCD) of the capitellum. MRI provides information about the size, location and stability of the OCD lesion. All of these factors are important when deciding treatment options (see Chapter 20 for more discussion). Unstable OCD lesions in the capitellum have a peripheral rim of high signal or an underlying fluid-filled cyst on T2-weighted images (Fig. 12-5). Stable OCD lesions have no peripheral signal abnormality.12 Loose bodies in the elbow joint can be visualized by MRI or MDCT, but smaller detached bone fragments are usually better visualized using MDCT (Fig 12-6).
Ultrasonography has the ability to dynamically delineate soft tissues and cartilage in detail.13 Soft tissue swelling, a mass (including vascular masses investigated with duplex Doppler and color flow Doppler), joint effusion, and fractures, particularly in infants and young children with unossified or minimally ossified epiphyses, are studied with this modality.1,7 Ultrasound can detect early changes of medial epicondylar fragmentation and OCD of the capitellum, even in the asymptomatic stage in selected populations such as young baseball players.10
As with other portions of the appendicular and axial skeletons, side-to-side comparison may be helpful when one is presented with an unfamiliar or a rare variant. Comparison views need to be obtained only in selected cases,14,15 such as when consultation with the standard text of normal cases is not helpful.5,11,17
NORMAL DEVELOPMENT
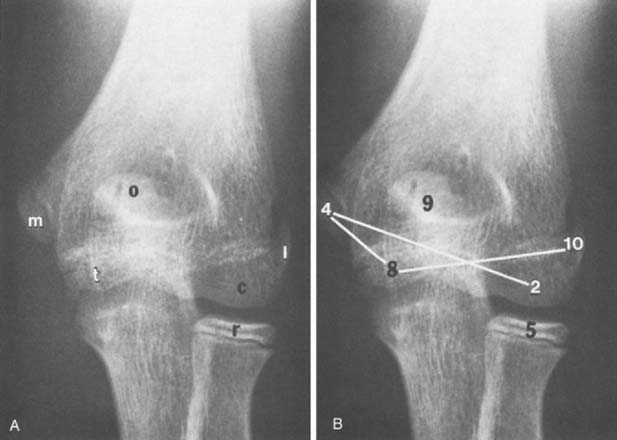
The maturation sequence at the elbow is more variable than that of the hand and wrist. Nonetheless, an appreciation of the normal sequence and timing of the appearance of ossification centers and maturation patterns is important for an understanding of the radiographic appearances of the elbow in children (Fig. 12-7). Several mnemonics have been suggested to help remember the time of appearance of the ossification of these centers. We find that the cross-connecting ossification centers (see Fig. 12-7B) are particularly helpful in remembering at least the order of ossification of these centers. An atlas entitled Radiology of the Pediatric Elbow5 shows standards for elbow maturation in children. To consistently evaluate the developing elbow, one must analyze each of the secondary centers of ossification, accounting for its appearance, configuration during development, and associated changes as it matures and eventually fuses with the humeral shaft. The descriptions that follow are brief, but they outline the major points of development and maturation of the centers.
CAPITELLUM
The capitellum, the first of the elbow’s six centers to ossify, generally becomes radiographically visible during the first and second years of life. Initially spherical, it flattens posteriorly to conform to the adjacent distal end of the humerus. The physis is broader posteriorly than anteriorly, giving the capitellum the appearance of a downward tilt; however, this appearance gradually disappears during the first decade (Fig. 12-8). During maturation, the capitellum fuses with the trochlea and the lateral epicondyle before it unites with the humeral shaft (Fig. 12-9).
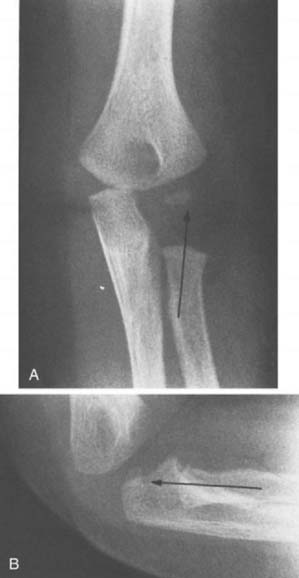
RADIOCAPITELLAR LINE
The radiocapitellar line is a line drawn through the long axis of the proximal radial shaft that should, in the absence of dislocation, pass through the middle of the capitellum ossification center. This is generally true in anteroposterior, lateral, or any oblique projection. In early development, however, the radial metaphysis is wedged so that on the anteroposterior projection a normal radial shaft line may appear to extend laterally to the capitellum. However, on the lateral projection, the normal radiocapitellar line can be appreciated (Fig. 12-10). In older patients, although it may appear that the radiocapitellar line is normal in one projection in a patient with a radial head dislocation, it invariably will be abnormal in the projection taken at right angles, generally the lateral projection.18
MEDIAL EPICONDYLE
The medial epicondyle is the second elbow ossification center to appear in the normal sequence, usually at about 4 years. Lying posteromedially, it is often best appreciated on the lateral projection (Fig. 12-11). Frequently, it develops from more than one ossific nucleus. Although it is the second humeral ossification center to appear, its development is slow, and it is usually the last center to unite with the humeral shaft in the normal child, sometimes as late as 15 or 16 years of age.20 This center may fuse with the trochlea before uniting with the humeral shaft. Injuries involving the nonunited medial epicondyle are relatively common and are among the most difficult to evaluate. Consequently, to avoid errors, Rodgers suggests making a habit of identifying the presence and the position of the medial epicondyle ossification center in each case.16 A classic example of the importance of appreciating the sequence of humeral ossification center appearance is avulsion and displacement of the medial epicondyle ossification center. This frequently results in the displacement of the medial epicondyle into the normal position of the trochlear ossification center. In a child between 4 and 8 years of age, at the time of appearance of the medial epicondyle and the trochlear ossification centers, a radiograph suggesting a trochlear ossification center, without visualization of a medial epicondyle center, should suggest that fracture and dislocation of the medial epicondyle have in fact occurred.13
RADIAL HEAD EPIPHYSIS
The initial ossification of this epiphysis is fairly predictable and usually occurs in the fifth year (see Fig. 12-7B). Although usually beginning as a sphere, the radial head epiphysis often matures as one or more flat sclerotic centers. This pattern may be mistakenly interpreted as a fracture. With maturation, the physis on the anteroposterior radiograph is wider laterally than medially, and this appearance, combined with the medial angulation of the radius at the junction of its shaft and neck, may suggest dislocation on anteroposterior views. Lateral projection of the elbow will not confirm a suspected dislocation. With further maturation of ossification of the proximal radial ossification center, the normal relationship of the radius and capitellum can be seen on anteroposterior radiographs. Notches or clefts of the metaphysis of the proximal radius often are seen as normal variations of ossification during maturation.11,17
Because fractures of the radial neck are extracapsular, they are not associated with hemarthrosis and abnormalities of the humeral fat pads.19
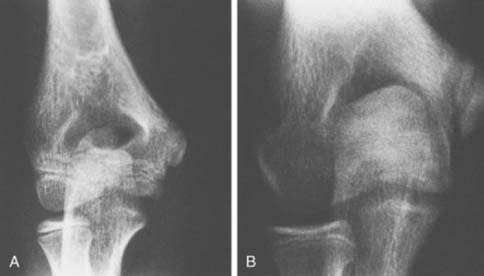
TROCHLEAR EPIPHYSIS
Ossification of the trochlea appears at about 8 years and often is initially multicentric (Figs. 12-12 and 12-13B). The trochlea frequently maintains an irregular contour during its development and should not be confused with abnormal processes such as trauma or avascular necrosis (Fig. 12-14). The trochlea will fuse with the capitellum before fusion with the distal humeral shaft. It is seldom fractured, except when associated with the vertical component of a supracondylar fracture or when its lateral edge is involved with a lateral condylar fracture.
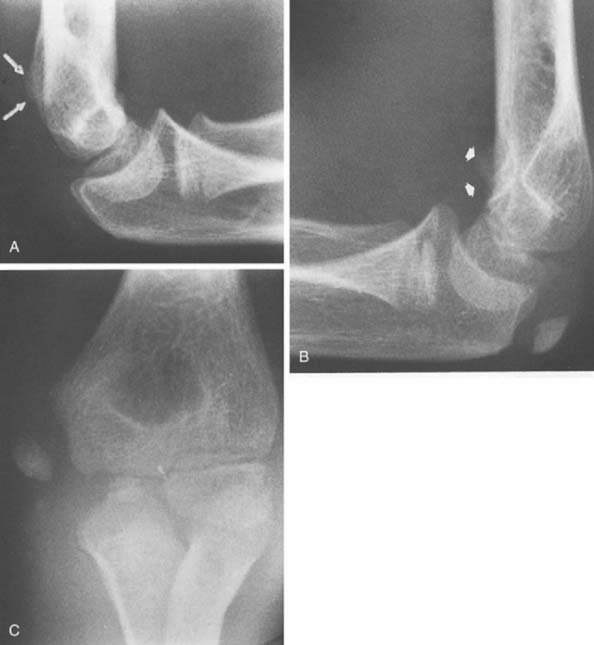
OLECRANON
The ossification center of the olecranon usually develops at 9 years of age, shortly after the trochlea and just before the lateral epicondylar epiphysis. The proximal end of the ulna flattens and becomes sclerotic just before the olecranon physis ossifies. Two ossification centers most often develop, and there is great variability in the configuration of the epiphysis. This results in an occasional misdiagnosis of acute fracture. The posterior ossification center is usually bigger than the anterior ossification center (Fig. 12-15), and these separate centers generally unite before fusion with the proximal humerus. This process usually begins at about 14 years of age.

FIGURE 12-15 A 13-year-old boy with double ossification center of the olecranon. The anterior nucleus is smaller.
The pattern of closure of the olecranon physis is distinct, with fusion occurring first along the joint line and then extending posteriorly. Frequently, fractures are wedged in the opposite direction.21
The olecranon physis has prominent sclerotic margins just before closure. Fusion proceeds posteriorly from the joint side or the anterior surface (Fig. 12-16). During its development, the physeal line remains relatively perpendicular to the ulnar shaft. As a result of differential growth, often with maturation, the olecranon growth plate, which initially is proximal to the elbow joint, comes to lie at a midelbow joint level by the time of fusion. This “wandering physeal line of the olecranon” does not occur in all individuals.4
Although the majority of olecranon fractures are intracapsular and are associated with alterations of fat pads, some are not. The tip of the olecranon is not within the capsule in some individuals. The only other common site of fracture related to the elbow that lies outside the joint capsule is the radial neck (see Chapter 17).4
LATERAL EPICONDYLE
The ossification center of the lateral epicondyle is the last of the elbow centers to appear. Usually, this center is first seen at 10 or 11 years of age, and it fuses to the humeral shaft at about 14 years of age. Unlike the other ossification centers of the elbow, the lateral epicondyle appears first as a thin sliver rather than as a round or spherical ossific nucleus (see Fig. 12-14).
Ossification commences at the lateral portion of the cartilaginous mold so that the physis appears particularly wide. The inferior aspect of the ossification begins at the junction between the distal humerus and the capitellum.5
Because of the relatively short time between the appearance and fusion of this center, it is not always certain in individual cases whether ossification is delayed or fusion to the humerus already has occurred. To avoid confusion about this point, it must be realized that before ossification, the humerus has a sharp, straight, sloping metaphyseal line that changes to a sloping, curving margin at the capitellum. The fused lateral epicondyle, on the other hand, has a smooth, curved margin that is continuous with the capitellum (Fig. 12-17).
NORMAL VARIANTS
The radial tuberosity lies medially at the junction of the medial shaft and the neck. On lateral views, it may appear as an undermineralized focus and may be misinterpreted as a destructive lesion of the bone (see Fig. 12-13). On the anteroposterior view of the elbow, the thin humeral olecranon fossa occasionally appears to be entirely lucent, the so-called perforated olecranon fossa (Fig. 12-18). In some instances, there is a bridge of bone crossing or a separate ossicle within a perforated olecranon fossa.

FIGURE 12-18 A 6-year-old boy with perforated olecranon fossa. There has been a previous supracondylar fracture.
A rare anatomic anomaly is a bony projection from the anterior medial distal humerus known as the supracondylar process (Fig. 12-19), which is discussed in Chapter 2.
1 Barr L.L. Elbow. Clin. Diagn. Ultrasound. 1995;30:135.
2 Beltran J., Rosenberg Z.S., Kawelblum M., Montes L., Bergman A.G., Strongwater A. Pediatric elbow fractures: MRI evaluation. Skeletal Radiol. 1994;23:277.
3 Blickman J.G., Dunlop R.W., Sanzone C.F., Franklin P.D. Is CT useful in the traumatized pediatric elbow? Pediatr. Radiol. 1990;20:184.
4 Brodeur A.E., Silberstein M.J., Graviss E.R. Radiology of the Pediatric Elbow. Boston: G. K. Hall, 1981.
5 Brodeur A.E., Silberstein M.J., Graviss E.R., Luisiri A. The basic tenets for appropriate evaluation of the elbow in pediatrics. Curr. Probl. Diagn. Radiol. 1983;12:1.
6 Chapman V., Grottkau B., Albright M., Elaini A., Halpern E., Jaramillo D. MDCT of the elbow in pediatric patients with posttraumatic elbow effusion. A. J. R. 2006;187:812.
7 Davidson R.S., Markowitz R.I., Dormans J., Drummond D.S. Ultrasonographic evaluation of the elbow in infants and young children after suspected trauma. J. Bone Joint Surg. 1994;76A:1804.
8 Gordon A.C., Friedman L., White P.G. Pictorial review: Magnetic resonance imaging of the paediatric elbow. Clin. Radiol. 1997;52:582.
9 Griffith J.F., Roebuck D.J., Cheng J.C.Y., Chan Y.L., Rainer T.H., Ng B.K., Metreweli C. Acute elbow trauma in children: Spectrum of injury revealed by MR imaging not apparent on radiographs. A. J. R. 2001;176:53.
10 Harada M., Takahara M., Sasaki J., Mura N., Ito T., Ogino T. Using sonography for the early detection of elbow injuries among young baseball players. A. J. R. 2006;187:1436.
11 Keats T.E. An Atlas of Normal Roentgen Variants That May Simulate Disease, 5th ed., St. Louis: Mosby-Year Book; 1992:395.
12 Kijowski R., De Smet A.A. MRI findings of osteochondritis dissecans of the capitellum with surgical correlation. A. J. R. 2005;185:1453.
13 Markowitz R., Davidson R.S., Harty M.P., Bellah R.D., Hubbard A.M., Rosenberg H.K. Sonography of the elbow in infants and children. A. J. R. 1992;159:829.
14 McCauley R.G.K., Schwartz A.M., Leonidas J.C., Darling D.B., Bankoff M.S., Swan C.S.2nd. Comparison views in extremity injury in children: an efficacy study. Radiology. 1979;131:95.
15 Merten D.F. Comparison radiographs in extremity injuries of childhood: current application in radiological practice. Radiology. 1978;126:209.
16 Rodgers L.F. Radiology of Skeletal Trauma. New York: Churchill Livingstone, 1982;435.
17 Schmidt H., Freyschmidt J. Köhler/Zimmer Borderlands of Normal and Early Pathologic Findings in Skeletal Radiology, 4th ed. New York: Thieme Medical Publishers, 1993.
18 Silberstein M.J., Brodeur A.E., Graviss E.R. Some vagaries of the capitellum. J. Bone Joint Surg. 1979;61A:244.
19 Silberstein M.J., Brodeur A.E., Graviss E.R. Some vagaries of the radial head and neck. J. Bone Joint Surg. 1982;64A:1153.
20 Silberstein M.J., Brodeur A.E., Graviss E.R., Luisiri A. Some vagaries of the medial epicondyle. J. Bone Joint Surg. 1981;63A:524.
21 Silberstein M.J., Brodeur A.E., Graviss E.R., Luisiri A. Some vagaries of the olecranon. J. Bone Joint Surg. 1981;63A:722.