 . The 3rd portion of duodenum crosses in front of the aorta and behind the superior mesenteric vessels
. The 3rd portion of duodenum crosses in front of the aorta and behind the superior mesenteric vessels  .
.
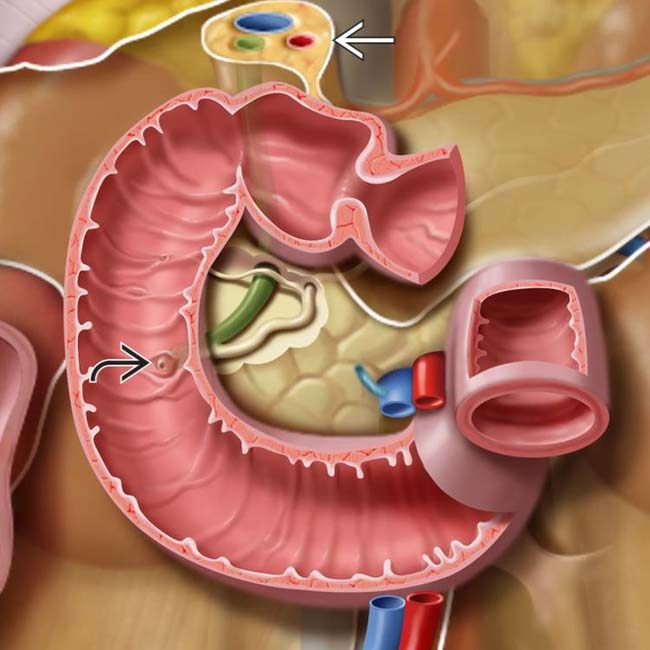
 lies along the medial wall of the 2nd duodenum. The hepatoduodenal ligament
lies along the medial wall of the 2nd duodenum. The hepatoduodenal ligament  attaches the duodenum to the porta hepatic and contains the bile duct, portal vein, and hepatic artery.
attaches the duodenum to the porta hepatic and contains the bile duct, portal vein, and hepatic artery.
 extending from the medial border of the 2nd portion of the duodenum.
extending from the medial border of the 2nd portion of the duodenum.
 . A completely fluid-filled diverticulum may mimic a cystic mass in the head of the pancreas.
. A completely fluid-filled diverticulum may mimic a cystic mass in the head of the pancreas.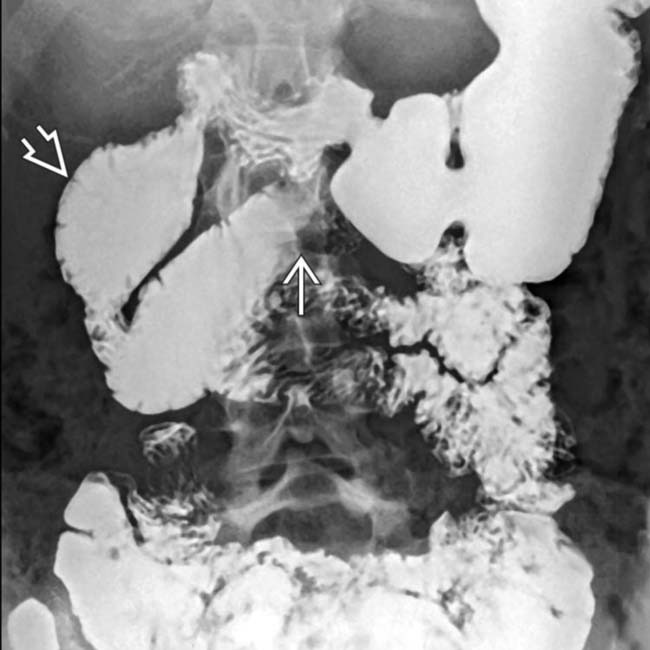
 of the midline duodenum, with dilation of the upstream duodenal lumen
of the midline duodenum, with dilation of the upstream duodenal lumen  . The remainder of the small bowel is normal.
. The remainder of the small bowel is normal.
 . Dilation of the small bowel lumen and a “hidebound” appearance of the small bowel folds (thin and closely spaced)
. Dilation of the small bowel lumen and a “hidebound” appearance of the small bowel folds (thin and closely spaced)  are typical features of this disease.
are typical features of this disease.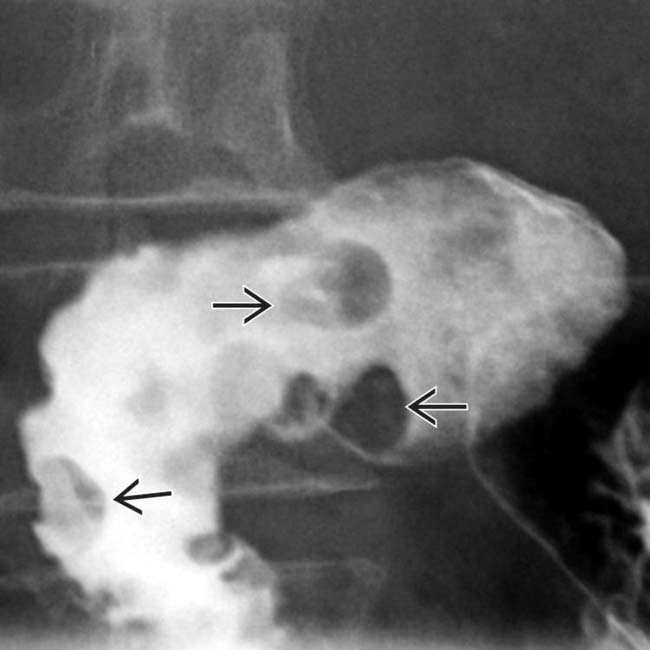
 in the duodenal bulb and descending duodenum. Endoscopic biopsy revealed hyperplasia and elements of hamartoma arising from Brunner glands.
in the duodenal bulb and descending duodenum. Endoscopic biopsy revealed hyperplasia and elements of hamartoma arising from Brunner glands.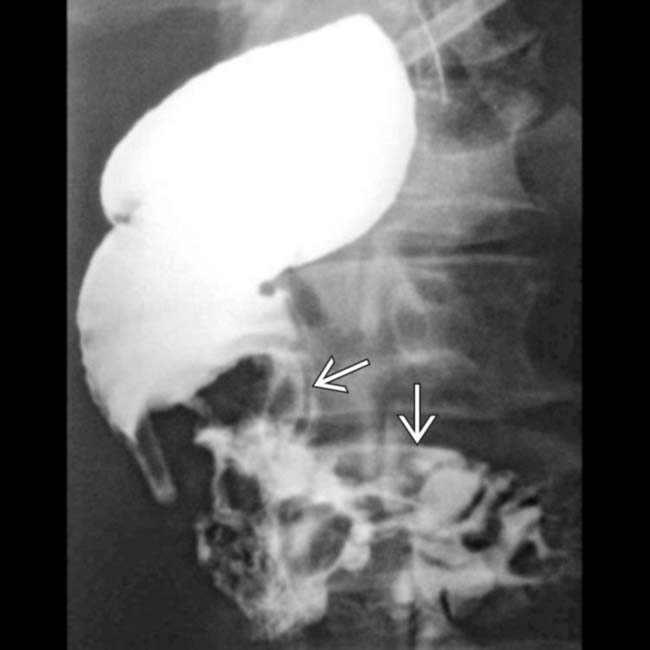
 filling much of the 2nd and 3rd portions of the duodenum. Note the “apple core” appearance, similar to that of colon cancer.
filling much of the 2nd and 3rd portions of the duodenum. Note the “apple core” appearance, similar to that of colon cancer.
 causing abrupt narrowing of the duodenal lumen and irregularity or destruction of the duodenal mucosa.
causing abrupt narrowing of the duodenal lumen and irregularity or destruction of the duodenal mucosa.
 within the duodenal lumen. The mass was resected and proved to be a large adenomatous polyp with foci of frank carcinoma.
within the duodenal lumen. The mass was resected and proved to be a large adenomatous polyp with foci of frank carcinoma.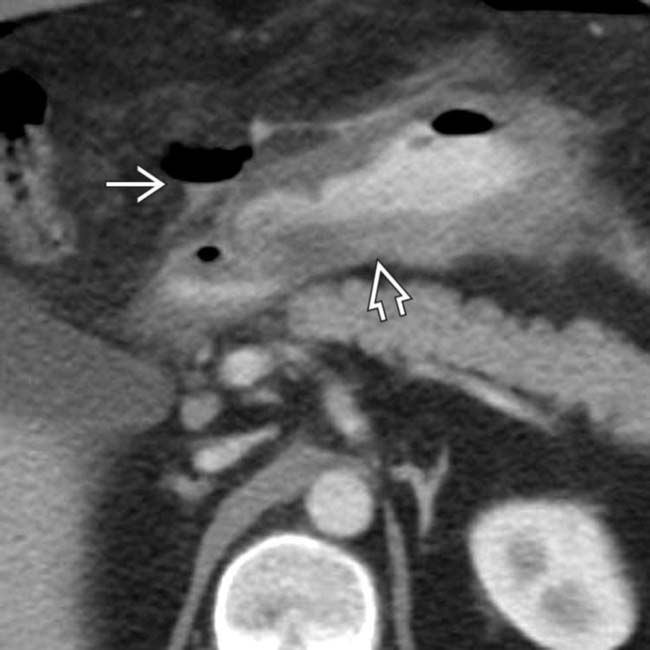
 with extraluminal oral contrast medium and gas
with extraluminal oral contrast medium and gas  tracking from the duodenal bulb. Surgery confirmed a perforated ulcer of the duodenal bulb and gastritis.
tracking from the duodenal bulb. Surgery confirmed a perforated ulcer of the duodenal bulb and gastritis.
 . While this might suggest a primary renal process, the correct diagnosis of a perforated duodenal ulcer is made by the finding of extraluminal gas surrounding the 2nd and 3rd portions of duodenum
. While this might suggest a primary renal process, the correct diagnosis of a perforated duodenal ulcer is made by the finding of extraluminal gas surrounding the 2nd and 3rd portions of duodenum  with its thickened wall.
with its thickened wall.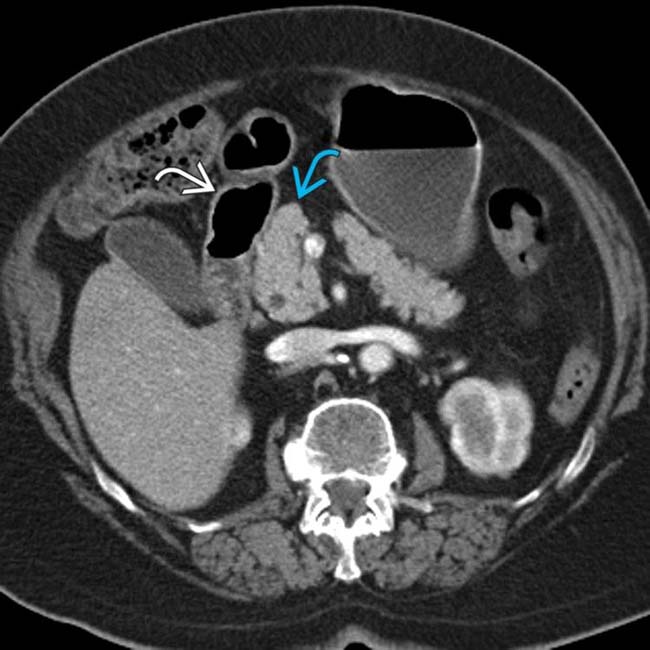
 , and pancreatic head
, and pancreatic head  appear normal.
appear normal.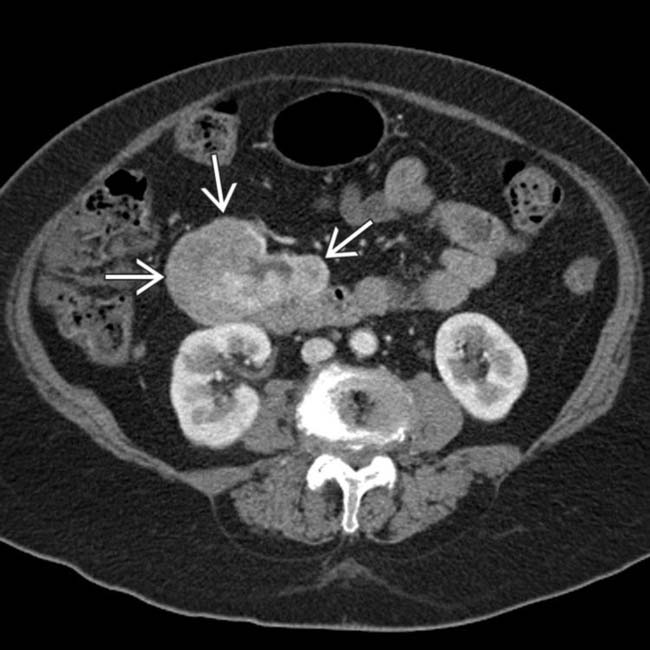
 arising from the duodenum.
arising from the duodenum.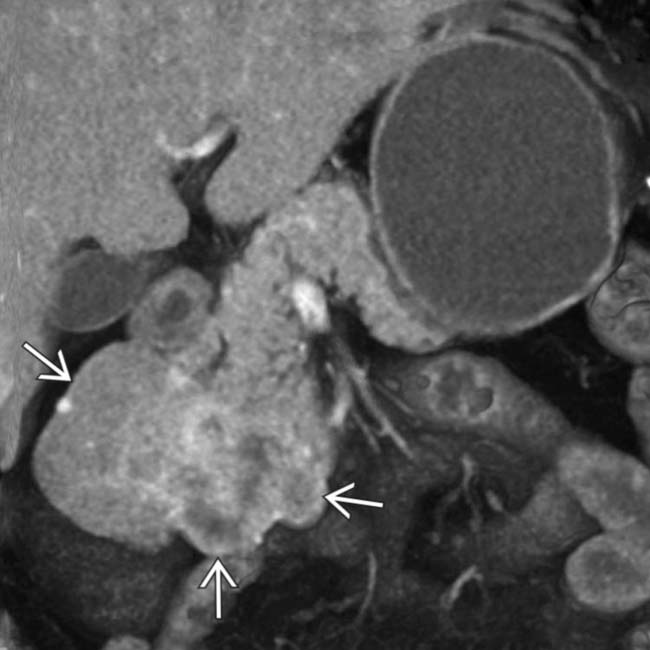
 arising from the duodenum.
arising from the duodenum.
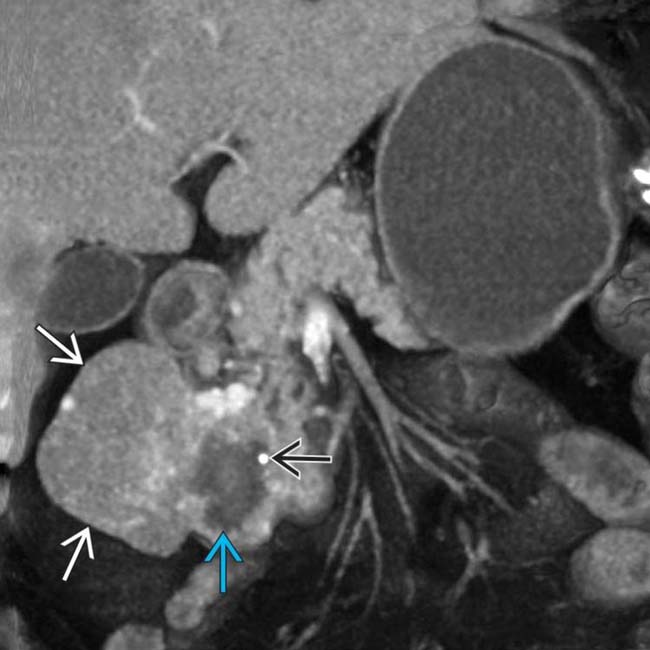
 and calcification
and calcification  within the mass
within the mass  . All features are characteristic of a duodenal GIST, confirmed at surgery. The duodenum is one of the more common locations for GI stromal tumors.
. All features are characteristic of a duodenal GIST, confirmed at surgery. The duodenum is one of the more common locations for GI stromal tumors.


