Ichthyoses

Management strategy
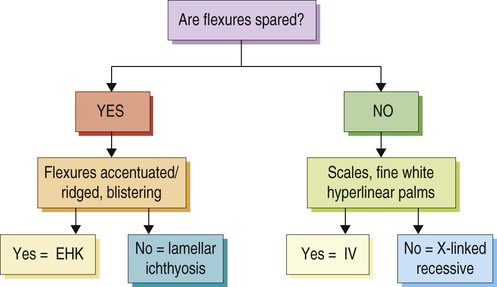
The key to management, where possible, is to establish an exact diagnosis. This provides a platform to plan therapy, discuss prognosis, and consider genetic counseling. It is important to identify the age of onset, the presence or absence of collodion membrane, blistering or erythroderma in the neonatal period, and the type, color, and distribution of scale. Family members should be examined. The Ichthyosis Support Group (ISG) provides a support network for families with resources and information sheets (www.ichthyosis.org.uk).










 Humidification of environment
Humidification of environment Bathing/soaking
Bathing/soaking Emollients
Emollients Keratolytics (salicylic acid (avoid in children), urea, α-hydroxy acids (e.g., lactic acid), propylene glycol)
Keratolytics (salicylic acid (avoid in children), urea, α-hydroxy acids (e.g., lactic acid), propylene glycol) Topical retinoids (tretinoin, tazarotene)
Topical retinoids (tretinoin, tazarotene) Topical liarozole
Topical liarozole Topical calcipotriol
Topical calcipotriol Topical N-acetylcysteine
Topical N-acetylcysteine Topical pimecrolimus 1%
Topical pimecrolimus 1% Narrowband UVB phototherapy (Netherton syndrome)
Narrowband UVB phototherapy (Netherton syndrome) Acitretin/etretinate
Acitretin/etretinate Isotretinoin
Isotretinoin Alitretinoin
Alitretinoin Liarozole
Liarozole