Hypothyroidism
Hypothyroidism is a condition that results from inadequate production or action of thyroid hormone, most commonly due to primary hypothyroidism, or failure of the thyroid gland itself. Hypothyroidism can be overt, with a frank decrease in serum thyroxine (T4) levels and a compensatory increase in thyroid-stimulating hormone (TSH) levels. More commonly seen is subclinical hypothyroidism (also called mild thyroid failure), in which the TSH is mildly elevated but T4 levels are normal. Subclinical hypothyroidism often manifests with few or no symptoms, but hypercholesterolemia and subtle cardiac abnormalities can be seen.
2. How common is hypothyroidism?
Hypothyroidism is a common condition. The prevalence of overt hypothyroidism in the United States is estimated at 0.3% to 0.4%, whereas that of subclinical hypothyroidism is much higher (4%-8%). The mean age at diagnosis is the mid-50s. Hypothyroidism is much more common in women, with a female-to-male ratio of 3:1. Postpartum hypothyroidism, a transient hypothyroid phase after pregnancy, occurs in 5% to 10% of women.
3. What are the two most common causes of hypothyroidism?
Although many disorders can cause hypothyroidism, the two most common causes are chronic lymphocytic thyroiditis (Hashimoto’s disease), an autoimmune form of thyroid destruction, and radioiodine-induced hypothyroidism after treatment of Graves’ disease (autoimmune hyperthyroidism).
4. List the less common causes of hypothyroidism.
 External irradiation to the neck
External irradiation to the neck
 Medications (antithyroid drugs, amiodarone, lithium, bexarotene, tyrosine kinase inhibitors, and interferon)
Medications (antithyroid drugs, amiodarone, lithium, bexarotene, tyrosine kinase inhibitors, and interferon)
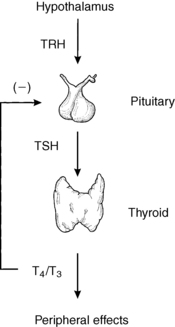
 Central (pituitary/hypothalamic) hypothyroidism (Fig. 34-1)
Central (pituitary/hypothalamic) hypothyroidism (Fig. 34-1)
 Endemic (iodine-deficient) goiter, which is fairly common outside the United States
Endemic (iodine-deficient) goiter, which is fairly common outside the United States
5. List the symptoms commonly experienced in hypothyroidism.
Hypothyroidism commonly manifests with nonspecific symptoms, such as fatigue, cold intolerance, depression, weight gain, weakness, joint aches, constipation, dry skin, hair loss, and menstrual irregularities.
6. What findings on physical examination are consistent with hypothyroidism?
Physical findings may be normal with mild thyroid failure and should not deter further workup if clinical suspicions are high. Common signs of moderate to severe hypothyroidism include:
 Hypertension (diastolic hypertension is a clue)
Hypertension (diastolic hypertension is a clue)
7. What does palpation of the thyroid reveal?
The thyroid may be enlarged, normal, or small in hypothyroidism, but thyroid consistency is usually firm.
8. Summarize unusual presentations of hypothyroidism.
Unusual presentations of hypothyroidism include megacolon, cardiomegaly, pericardial effusion, and congestive heart failure (CHF). Severe CHF in one reported patient scheduled for cardiac transplant resolved with thyroid hormone replacement alone.
9. Describe the laboratory values that may be abnormal during hypothyroidism.
Laboratory clues to hypothyroidism include normochromic, normocytic anemia (menstruating women may also have iron deficiency anemia due to excessive bleeding from irregular menses), hyponatremia, hypercholesterolemia, and elevations of creatine phosphokinase.
10. What tests best confirm the diagnosis of hypothyroidism in the outpatient setting?
Many thyroid function tests are available to the clinician, including assessments of TSH, T4, triiodothyronine (T3), resin uptake, free T4, free T3, and reverse T3. In the outpatient setting only one test is usually necessary: assessment of TSH. TSH, which is synthesized and secreted from the anterior pituitary gland, is the most sensitive indicator of thyroid function in the nonstressed state. Basically, if the TSH level is normal (range: 0.5-5 mU/L), the patient is euthyroid; if the TSH is elevated (> 5 mU/L), the patient has primary gland failure. In the unusual case in which central hypothyroidism is suspected, a free T4 measurement is the best screening test.
11. How should total T4 levels be interpreted?
Care must be taken in interpreting total T4 levels (occasionally performed on health-screening panels). Many conditions unrelated to thyroid disease cause low or elevated values of total T4 because more than 99% of T4 is protein-bound, and total T4 levels depend on the amount of thyroid hormone–binding proteins, which may vary greatly. The total T4 level must always be compared with the patient’s T3 resin uptake (T3RU) value, which reflects the amount of thyroid hormone–binding protein.
12. Explain why thyroid function test results are more difficult to interpret in acutely ill inpatients.
Interpretation of thyroid function test results in acutely ill inpatients is more difficult when hypothyroidism is suspected. Acute nonthyroidal illness may cause suppression of the total T4, free T4, total T3, free T3, and TSH levels, and TSH may then be elevated in the recovery phase (see Chapter 39). Medications, such as dopamine and glucocorticoids, may also suppress the TSH value.
13. How do you diagnose hypothyroidism in acutely ill inpatients?
When hypothyroidism is suspected in the stressed, hospitalized patient, a combination of clinical signs (inappropriate bradycardia, puffy facies, dry skin, and delayed relaxation of deep tendon reflexes) and laboratory values (TSH and free T4 levels) is necessary to exclude or confirm the diagnosis of hypothyroidism. If these values are equivocal, measurement of a reverse T3 level, which is normal or elevated in nonthyroidal illness and low in hypothyroidism, may prove helpful. Inpatient TSH testing also may be confounded by normal diurnal variations in TSH. TSH levels in euthyroid people may exceed the normal range at night, when patients are frequently admitted. A morning test may help clarify the significance of a mildly elevated TSH.
14. Who should be treated for hypothyroidism?
All patients with overt hypothyroidism should be treated. Treatment is also generally recommended for subclinical hypothyroidism, especially for patients with a persistent TSH value greater than 10 mU/L, because when patients are treated with levothyroxine, they may have an improved sense of well-being and improvements in their cardiac and lipid abnormalities. Thyroid antibodies, an indicator of autoimmune thyroid disease, may help predict which patients with subclinical hypothyroidism will progress to overt hypothyroidism; testing is recommended for patients with minimally elevated TSH values.
15. Which thyroid hormone preparation should you use?
Since 1891, when sheep thyroid extract was first used to treat myxedema, many preparations have been developed and are still available. Currently the best replacement regimen is levothyroxine (LT4).
16. What other thyroid hormone preparations are available?
Other thyroid hormone preparations include liothyronine (LT3), which is reserved for special cases because of its potency and short half-life, and desiccated thyroid and thyroglobulin, which give unpredictable serum thyroid hormone concentrations because of variable content and bioavailability.
17. What is the recommended dose of LT4 for replacement therapy in a hypothyroid patient?
Otherwise healthy, young patients may be started on full replacement doses of LT4 (1.6 μg/kg/day). Elderly patients and patients with known or suspected cardiac disease should be started on low doses of LT4 (25-50 μg/day), which are increased by 25 μg/day every for 4 to 6 weeks or until the TSH value is normal. In patients with subclinical hypothyroidism, consider starting with 50% to 75% of the predicted full replacement dose.
18. What is the appropriate goal for TSH in the treatment of primary hypothyroidism?
Traditionally, the target TSH in treated hypothyroid patients has been between 0.5 and 2.0 mU/L, which represents the lower end of the normal range reported by most laboratories. This target was based on the fact that when the usual reference ranges for TSH were developed, they included subjects with antithyroid antibodies suggestive of occult autoimmune thyroid disease. The “normal” ranges are therefore thought to be skewed toward higher TSH values. When normal subjects with no antithyroid antibodies are evaluated, most have TSH values below 2.5 mU/L. However, two studies have failed to provide evidence that a low-normal TSH value is clinically superior to a value in the high-normal reference range.
19. Discuss the evidence supporting combination T4/T3 therapy.
The medical and lay literature has taken a renewed interest in combination therapy. Studies in thyroidectomized animals have shown that T4 therapy alone does not restore tissue levels of T4 and T3 to euthyroid values, even when the TSH value is normalized. Small studies in humans have suggested that patients taking combination therapy have improved cognitive function, mood scores, and cholesterol values as well as decreased weight than when they take LT4 alone. One study suggested that the response to T4/T3 therapy might vary depending on deiodinase gene variations. Although these studies are provocative and intriguing, a large metaanalysis showed no demonstrable difference in symptoms or weight between LT4 monotherapy and combination therapy, and most experts agree that more information is needed before we can recommend combination T4/T3 therapy in most patients. Our current approach is to discuss this information openly with inquiring patients.
20. When should you consider combination T4/T3 therapy?
We suggest a trial of LT4 alone to normalize TSH to within the low-normal range (0.5-2.0 mU/L) for a period of 2 to 4 months. Many patients do extremely well with this approach. Patients who have low-normal TSH while taking LT4 and still feel “hypothyroid” require further evaluation before LT3 therapy is considered. We generally exclude anemia and vitamin B12 deficiency (associated with Hashimoto’s thyroiditis) and inquire about sleep apnea. If results of this assessment are negative, we decrease the LT4 dosage by 12 to 25 μg, which is taken at night, and add 5 μg of liothyronine (LT3), to be taken in the morning. The goal is to see whether the patient’s symptoms improve without persistent suppression of the serum TSH (measured in the morning before medication is taken). No data clearly support or refute this position; we believe it is a position of “good” medical practice.
21. How should the clinician approach surgery in the hypothyroid patient?
There are two broad categories to consider: emergency/cardiac surgery and elective surgery. Hypothyroidism is associated with minor postoperative complications—gastrointestinal (prolonged constipation, ileus) as well as neuropsychiatric (confusion, psychosis); in addition, the incidence of fever in response to infections is lower. Patients scheduled for elective surgery should wait until TSH values are normalized because of the potential postoperative complications associated with hypothyroidism. However, rates of mortality and major complications (blood loss, arrhythmias, and impaired wound healing) in hypothyroid patients are similar to those in euthyroid patients.
22. Summarize the current recommendations for emergency surgery.
Current recommendations are to proceed with emergency surgery in the hypothyroid patient and to monitor for potential postoperative complications while giving replacement therapy with LT4. Patients with ischemic coronary artery disease requiring surgery should proceed without LT4 replacement because T4 increases myocardial oxygen demands and may precipitate worsening cardiac symptoms if given before surgery. Postoperatively, the patient should receive replacement therapy with LT4 at a slow rate and should be monitored for CHF (rate increased in hypothyroid patients undergoing cardiac surgery).
23. How does myxedema differ from hypothyroidism?
Myxedema is a severe, uncompensated form of prolonged hypothyroidism. Complications include hypoventilation, cardiac failure, fluid and electrolyte abnormalities, and coma (see Chapter 38). Myxedema coma is frequently precipitated by an intercurrent systemic illness, surgery, or narcotic/hypnotic drugs. Patients with myxedema coma should receive replacement therapy with 300 to 500 μg of intravenous LT4 followed by 50 to 100 μg each day. Because conversion of T4 to T3 (active hormone) is decreased with severe illness, patients with profound cardiac failure that requires pressors or patients whose TSH level is unresponsive to 1 to 2 days of LT4 therapy should be given LT3 at 12.5 μg intravenously every 6 hours.
Almandoz, J, Gharib, H, Hypothyroidism. etiology, diagnosis, and management. Med Clin N Am 2012;96:203–221.
Arem, R, Patsch, W. Lipoprotein and apolipoprotein levels in subclinical hypothyroidism. Arch Intern Med. 1990;150:2097–2100.
Boeving, A, Paz-Filho, G, Radominski, R, et al, Low-normal or high-normal thyrotropin target levels during treatment of hypothyroidism. a prospective, comparative study. Thyroid 2011;21:355–360.
Bunevicius, R, Kazanavicius, G, Zalinkevicius, R, et al. Effects of thyroxine as compared with thyroxine plus triiodothyronine in patients with hypothyroidism. N Engl J Med. 1998;340:424–429.
Canaris, GJ, Manowitz, NR, Mayor, G, et al. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;104:526–534.
Celi, F, Zemskova, M, Linderman, J, et al, Metabolic effects of liothyronine therapy in hypothyroidism. a randomized, double-blind, crossover trial of liothyronine versus levothyroxine. J Clin Endocrinol Metab 2011;96:3466–3474.
Cooper, DS, Halpern, R, Wood, LC, et al. L-thyroxine therapy in subclinical hypothyroidism. Ann Intern Med. 1984;101:18–24.
Demers, LM, Spencer, CA, Laboratory medicine practice guidelines. laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid 2003;13:45–56.
Elder, J, McLelland, A, O’Reilly, SJ, et al. The relationship between serum cholesterol and serum thyrotropin, thyroxine, and tri-iodothyronine concentrations in suspected hypothyroidism. Ann Clin Biochem. 1990;27:110–113.
Grozinsky-Glasberg, S, Fraser, A, Nahshoni, E, et al, Thyroxine-triiodothyronine combination therapy versus thyroxine monotherapy for clinical hypothyroidism. meta-analysis of randomized controlled trials. J Clin Endocrinol Metab 2006;91:2592–2599.
Hay, ID, Duick, DS, Vliestra, RE, et al, Thyroxine therapy in hypothyroid patients undergoing coronary revascularization. a retrospective analysis. Ann Intern Med 1981;95:456–457.
Hollowell, JG, Staehling, NW, Flanders, WD, et al, Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994). National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489–499.
Ladenson, PW. Recognition and management of cardiovascular disease related to thyroid dysfunction. Am J Med. 1990;88:638–641.
Ladenson, PW, Levin, AA, Ridgway, EC, et al. Complications of surgery in hypothyroid patients. Am J Med. 1984;77:262–266.
Mandel, SJ, Brent, GA, Larsen, PR. Levothyroxine therapy in patients with thyroid disease. Ann Intern Med. 1993;119:492–502.
Panicker, V, Saravanan, P, Vaidya, B, et al. Common variation in the DIO2 gene predicts baseline psychological well-being and response to combination thyroxine plus triiodothyronine therapy in hypothyroid patients. J Clin Endocrinol Metab. 2009;94:1623–1629.
Patel, R, Hughes, RW. An unusual case of myxedema megacolon with features of ischemic and pseudomembranous colitis. Mayo Clin Proc. 1992;67:369–372.
Rosenthal, MJ, Hunt, WC, Garry, PJ, et al, Thyroid failure in the elderly. microsomal antibodies as discriminant for therapy. JAMA 1987;258:209–213.
Roti, E, Minelli, R, Gardini, E, et al. The use and misuse of thyroid hormone. Endocr Rev. 1993;14:401–423.
Walsh, J, Ward, L, Burke, V, et al, Small changes in thyroxine dosage do not produce measurable changes in hypothyroid symptoms, well-being, or quality of life. results of a double-blind, randomized clinical trial. J Clin Endocrinol Metab 2006;91:2624–2630.