57
Hypertrichosis and Hirsutism
Hypertrichosis
• Three mechanisms of hypertrichosis are generally recognized:
• Rx: treat underlying condition, if possible, otherwise see Table 57.2.
Table 57.2
Treatment options for hypertrichosis and unwanted hair.
Epilation technique results typically last longer than those of depilation. Chemical depilatories work by dissolving hair shafts, specifically by breaking disulfide bonds.
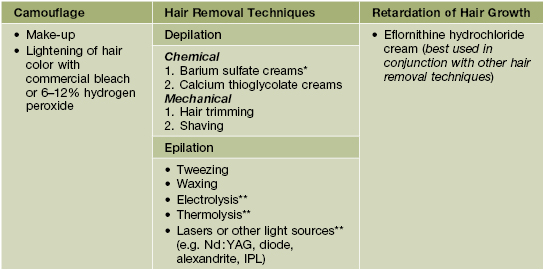
* More effective than calcium thioglycolate but more irritating and odiferous.
** These epilatory methods are operator-dependent and have the potential for permanent hair removal results.
IPL, intense pulsed light.
Generalized Hypertrichosis
• The presence of lanugo hair, excess vellus hair, or terminal hair on most of the body.
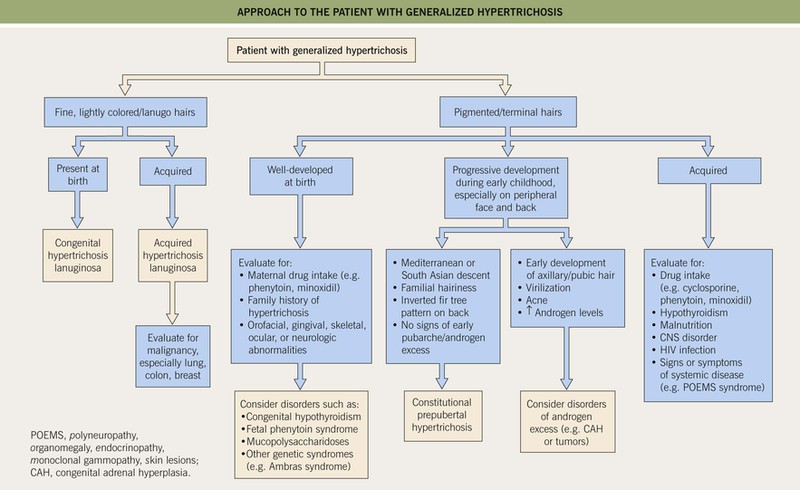
• An approach to a patient with generalized hypertrichosis is presented in Fig. 57.1.
Localized Hypertrichosis
• Congenital localized hypertrichosis is usually related to an underlying hamartoma or occurs at a specific anatomic site (Table 57.1; Figs. 57.2–57.6).
Table 57.1
Classification and key features of selected disorders of localized hypertrichosis.
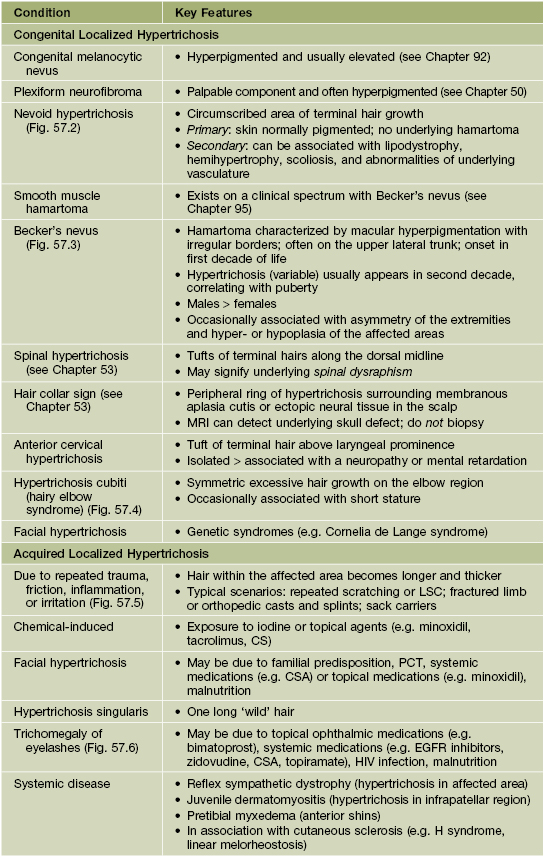
LSC, lichen simplex chronicus; PCT, porphyria cutanea tarda; CSA, cyclosporine; EGFR, epidermal growth factor receptor.

Fig. 57.2 Nevoid hypertrichosis in the scalp of a young boy. There was no underlying melanocytic nevus or hyperpigmentation. Courtesy, Jean L. Bolognia, MD.

Fig. 57.4 Hypertrichosis cubiti. Multiple terminal hairs on both elbows in a child. Courtesy, Francisco M. Camacho Martinez, MD.

Fig. 57.5 Acquired localized hypertrichosis. Hypertrichosis, hyperpigmentation, and epidermal hyperplasia at the site of friction.

Fig. 57.6 Unilateral trichomegaly. Bimatoprost ophthalmic solution (0.03%) was applied to one eye to treat glaucoma. Courtesy, Jean L. Bolognia, MD.
• Acquired localized hypertrichosis most often develops after repeated trauma, friction, irritation, or inflammation (see Table 57.1).
Hirsutism
• Affects ~5–10% of females of reproductive age; can also affect postmenopausal women.
• Quantified using the modified Ferriman and Gallwey (mFG) method (Fig. 57.7).
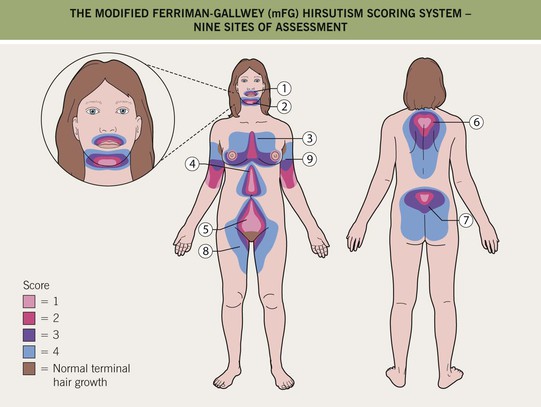
Fig. 57.7 The modified Ferriman–Gallwey (mFG) hirsutism scoring system. In this system, nine body areas are evaluated for the amount of terminal hair growth. A score of ‘0’ (no terminal hair growth) up to ‘4’ (frankly virile) is given to each of the nine areas and these are added together to compute a hormonal hirsutism score (mFG score). A total score <2–3 is considered normal for East Asian and Native American females, whereas <6–8 is considered normal in other populations.
• Defined as an mFG score of >2–3 in women from East Asia as well as Native Americans or an mFG score of ≥6–8 in other populations.
• Etiologies of hyperandrogenism and hirsutism in premenopausal females include.
– Most common: polycystic ovary syndrome (PCOS), idiopathic (end-organ sensitivity; Fig. 57.8).

Fig. 57.8 Facial hirsutism in a young female. This can be due to hyperandrogenism or end-organ sensitivity. Courtesy, Francisco M. Camacho Martinez, MD.
– Less common: nonclassic congenital adrenal hyperplasia, ovarian hyperthecosis, tumoral.
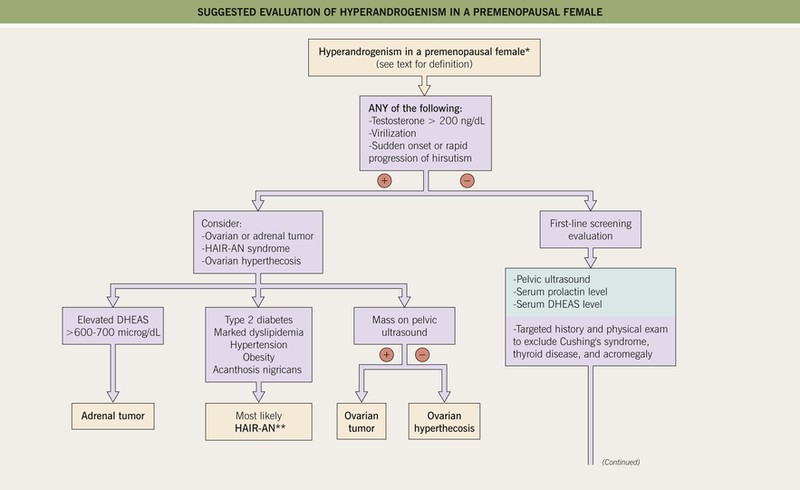
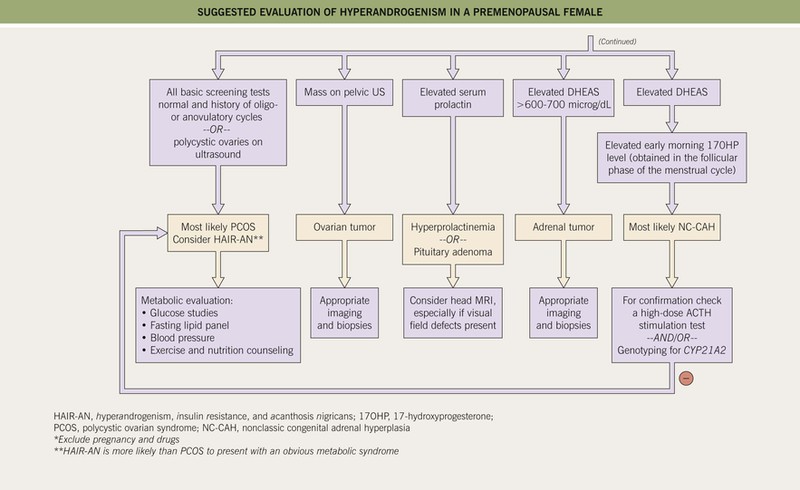
• Suggested algorithms for the evaluation of hirsutism and for hyperandrogenism are shown in Figs. 57.9 and 57.10, respectively.
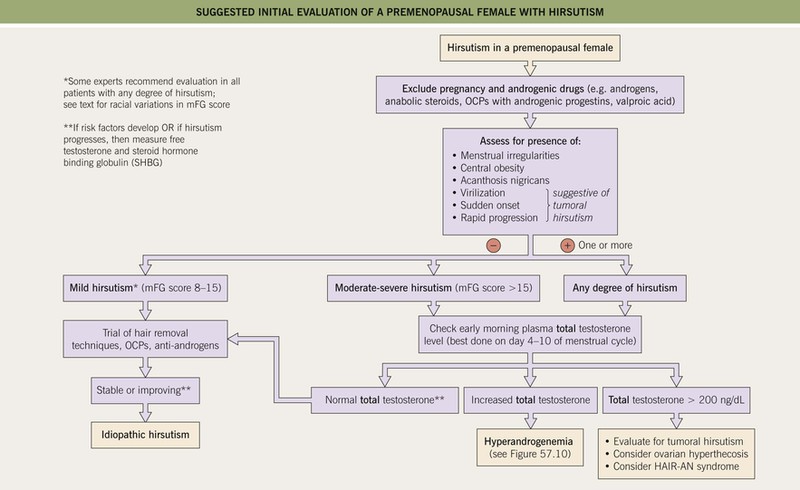
Fig. 57.9 Suggested initial evaluation of a premenopausal female with hirsutism (based on 2008 Endocrine Society clinical practice guidelines). OCP, oral contraceptive pills; mFG, modified Ferriman–Gallwey score (see Fig. 57.7); HAIR-AN, hyperandrogenism, insulin resistance, acanthosis nigricans syndrome.
Polycystic Ovary Syndrome (PCOS)
• Diagnosed by the presence of ≥2 of the following criteria and the exclusion of other possible etiologies (see Fig. 57.10):
1. Oligo- or anovulation (<8 menses/year or cycles >35 days).
2. Clinical and/or biochemical signs of hyperandrogenism (Fig. 57.11).

Fig. 57.11 Hirsutism in a young woman with polycystic ovarian syndrome (PCOS). Modified Ferriman–Gallwey (mFG) score of 9 based on three sites: chest, upper abdomen, and lower abdomen.
3. Polycystic ovaries (pelvic ultrasound).
• Other associated findings may include acanthosis nigricans and insulin resistance; patients are at increased risk for the metabolic syndrome (see Table 45.11), infertility, obstructive sleep apnea, and possibly endometrial carcinoma.
• Rx of hirsutism: hormonal agents (Table 57.3) as well as general hair removal methods (see Table 57.2).
Table 57.3
Systemic agents and practical treatment recommendations for hirsutism and hyperandrogenism.
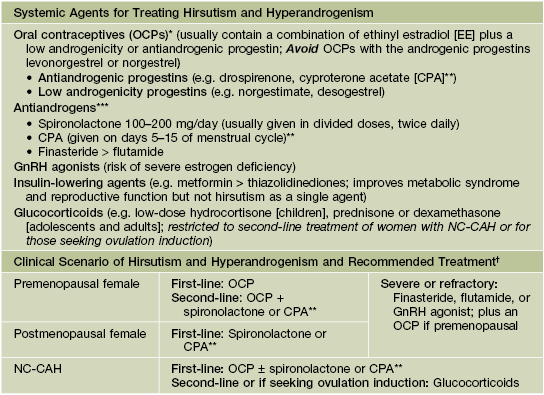
* Should avoid in females who smoke or who have risk factors for hypercoagulability and thrombosis.
** CPA is not available in the United States.
*** Requires concomitant reliable contraceptive method because of the risk of feminization of the male fetus.
† A waiting period of 6–9 months is recommended after initiating a treatment and before adding or changing medications.
NC-CAH, nonclassic congenital adrenal hyperplasia.
Idiopathic Hirsutism
Nonclassic Congenital Adrenal Hyperplasia (NC-CAH)
Ovarian Hyperthecosis
• Occurs in both premenopausal and postmenopausal females.
• Clinical features are similar to those of PCOS but with more pronounced and long-standing hirsutism, an increased likelihood of virilization (Fig. 57.12), and the occurrence postmenopause.

Fig. 57.12 Facial hirsutism (mFG score 4) due to ovarian hyperthecosis. Courtesy, Robert Hartman, MD.
• Testosterone levels are often quite elevated (>200 ng/dl); DHEAS can be normal or increased (see Fig. 57.10).
• Compared to tumoral hirsutism, a slower onset of symptoms and more gradual worsening over years.
• Increased risk of insulin resistance, type 2 diabetes, and endometrial carcinoma.
Tumoral Hirsutism
HAIR-AN Syndrome
• Hyperandrogenism, insulin resistance, and acanthosis nigricans syndrome.
• Marked insulin resistance leads to secondary increased insulin levels and resultant increased ovarian androgen production.
• More likely than PCOS to have overt type 2 diabetes, hypertension, and cardiovascular disease.
• Evaluation involves excluding an androgen-secreting tumor and PCOS.
Hirsutism Associated with Other Endocrine Abnormalities
• Cushing’s syndrome, hyperprolactinemia, pituitary adenoma, acromegaly, and thyroid dysfunction may present with hirsutism and other signs of hyperandrogenism, but typically manifest with other distinguishing and diagnostic features specific to the underlying disease (see Chapter 45).
For further information see Ch. 70. From Dermatology, Third Edition.