Chapter 41 Hypertension
1 What are the hemodynamic determinants of blood pressure (BP)?
Arterial BP is the product of cardiac output (CO) and systemic vascular resistance (SVR).
3 What are the target organs affected by hypertensive crisis?
Four organs are the usual target of severely elevated BP:
 Kidneys: acute kidney injury caused by proliferative endarteritis and fibrinoid necrosis of afferent artery
Kidneys: acute kidney injury caused by proliferative endarteritis and fibrinoid necrosis of afferent artery
 Brain: hypertensive encephalopathy, cerebrovascular accidents (CVA)
Brain: hypertensive encephalopathy, cerebrovascular accidents (CVA)
 Eye or retina: retinal hemorrhage or exudates or papilledema
Eye or retina: retinal hemorrhage or exudates or papilledema
 Heart: acute coronary syndrome, decompensated heart failure, aortic dissection, and acute intravascular hemolysis
Heart: acute coronary syndrome, decompensated heart failure, aortic dissection, and acute intravascular hemolysis
9 Outline the typical long-term antihypertensive regimen after successful treatment of malignant hypertension or hypertensive crisisss
10 What is the appropriate short-term treatment for hypertension in a patient with pheochromocytoma?
13 Why is BP elevated in patients with CVA?
14 How should hypertension be treated in patients with CVA?
The consensus guidelines on treatment of intracerebral bleeding:
 IV medications should be used to treat SBP > 200 mm Hg or MAP > 150 mm Hg with BP monitoring done every 5 minutes.
IV medications should be used to treat SBP > 200 mm Hg or MAP > 150 mm Hg with BP monitoring done every 5 minutes.
 In suspected intracranial hypertension, BP should be lowered with a parenteral agent if SBP is > 180 mm Hg or MAP > 130 mm Hg while maintaining CPP above 60 to 80 mm Hg.
In suspected intracranial hypertension, BP should be lowered with a parenteral agent if SBP is > 180 mm Hg or MAP > 130 mm Hg while maintaining CPP above 60 to 80 mm Hg.
 In the absence of elevated ICP, treat SBP > 180 mm Hg and MAP > 130 mm Hg with a target BP of 160/90 mm Hg or a MAP of 110 mm Hg.
In the absence of elevated ICP, treat SBP > 180 mm Hg and MAP > 130 mm Hg with a target BP of 160/90 mm Hg or a MAP of 110 mm Hg.
 The rate of BP reduction should be slowed if the patient’s neurologic status deteriorates. Oral therapy should be instituted before parenteral treatment is discontinued. Clonidine or α-methyldopa should be avoided because of the risk of impaired cerebral function.
The rate of BP reduction should be slowed if the patient’s neurologic status deteriorates. Oral therapy should be instituted before parenteral treatment is discontinued. Clonidine or α-methyldopa should be avoided because of the risk of impaired cerebral function.
15 Describe the short-term treatment of hypertension in patients with ischemic heart disease and ongoing angina
19 Why does lowering of BP potentially result in a decline in glomerular filtration rate (GFR) in severe hypertension?
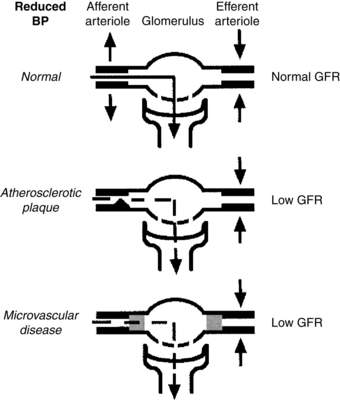
Normally, GFR is maintained despite decreases in BP by compensatory increases in efferent arteriolar tone (Fig. 41-1) Two major causes exist of loss of GFR after reduction of BP in the setting of severe hypertension:
 RAS: In a patient with a fixed atherosclerotic lesion of the main renal artery, a drop in BP can cause a fall in GFR because the fixed lesion limits afferent arteriolar flow to such an extent that even maximal elevation in efferent arteriolar tone cannot compensate and maintain GFR.
RAS: In a patient with a fixed atherosclerotic lesion of the main renal artery, a drop in BP can cause a fall in GFR because the fixed lesion limits afferent arteriolar flow to such an extent that even maximal elevation in efferent arteriolar tone cannot compensate and maintain GFR.
 Long-standing essential hypertension: In this setting, no macrovascular abnormalities are present; the problem is marked sclerosis of the microvasculature of the kidney, including the afferent artery. Because of afferent arteriolar sclerosis, the afferent artery is unable to vasodilate in response to a drop in BP. Hence, GFR falls when BP is lowered even with increases in efferent arteriolar tone that normally would offset, at least partially, decreases in BP.
Long-standing essential hypertension: In this setting, no macrovascular abnormalities are present; the problem is marked sclerosis of the microvasculature of the kidney, including the afferent artery. Because of afferent arteriolar sclerosis, the afferent artery is unable to vasodilate in response to a drop in BP. Hence, GFR falls when BP is lowered even with increases in efferent arteriolar tone that normally would offset, at least partially, decreases in BP.
20 When should an evaluation for secondary hypertension be considered?
 At initial presentation of malignant hypertension (especially if the patient is white, younger than 30 years, or older than 50 years of age)
At initial presentation of malignant hypertension (especially if the patient is white, younger than 30 years, or older than 50 years of age)
 When rapid onset of severe hypertension occurs within less than 5 years
When rapid onset of severe hypertension occurs within less than 5 years
 When an increase in serum creatinine level occurs after the initiation of ACE inhibitor treatment
When an increase in serum creatinine level occurs after the initiation of ACE inhibitor treatment
 In compliant patients whose BP is difficult to control after an adequate trial with a combination of diuretic, β-blocker, and potent vasodilator
In compliant patients whose BP is difficult to control after an adequate trial with a combination of diuretic, β-blocker, and potent vasodilator
21 What are the important causes of secondary hypertension?
Secondary hypertension accounts for 5% of cases of hypertension.
 Renal: renovascular disease, renal parenchymal disease, polycystic kidney disease, Liddle syndrome, syndrome of apparent mineralocorticoid excess, hypercalcemia
Renal: renovascular disease, renal parenchymal disease, polycystic kidney disease, Liddle syndrome, syndrome of apparent mineralocorticoid excess, hypercalcemia
 Endocrine: hyperthyroidism, hypothyroidism, primary hyperaldosteronism, Cushing syndrome, pheochromocytoma, congenital adrenal hyperplasia
Endocrine: hyperthyroidism, hypothyroidism, primary hyperaldosteronism, Cushing syndrome, pheochromocytoma, congenital adrenal hyperplasia
 Drugs: prescription (e.g., estrogen, cyclosporine, steroids); over-the-counter (e.g., pseudoephedrine, nonsteroidal antiinflammatory drugs); illicit (e.g., tobacco smoking, ethanol, cocaine)
Drugs: prescription (e.g., estrogen, cyclosporine, steroids); over-the-counter (e.g., pseudoephedrine, nonsteroidal antiinflammatory drugs); illicit (e.g., tobacco smoking, ethanol, cocaine)
 Neurogenic: increased intracranial pressure, spinal cord section
Neurogenic: increased intracranial pressure, spinal cord section
 Miscellaneous: coarctation of aorta, obstructive sleep apnea, polycythemia vera
Miscellaneous: coarctation of aorta, obstructive sleep apnea, polycythemia vera
22 What are the causes of primary aldosteronism, and how should they be distinguished?
Key Points Hypertension
1. Hypertensive crisis (or hypertensive emergency) is the turning point in the course of hypertension when the immediate management of elevated BP plays a decisive role in limiting or preventing target organ damage.
2. Hypertensive crises can damage four main target organ systems: eye, brain, heart, and kidney.
3. The short-term treatment of choice for malignant hypertension is IV sodium nitroprusside.
4. Long-term therapy for malignant hypertension should include a vasodilator such as hydralazine or minoxidil, a β-blocker, and a diuretic agent.
5. Nitroglycerin and β-blockers are the initial agents of choice for patients with ischemic heart disease and angina.
1 Adams H.P.Jr., del Zoppo G., Alberts M.J., et al. Guidelines for the early management of adults with ischemic stroke. Stroke. 2007;5:1655–1711.
2 Kaplan N.M. Pheochromocytoma. In: Kaplan N.M., ed. Clinical Hypertension. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 1998:345–363.
3 Kelleher C.L., Linas S.L. Hypertensive crisis: emergency and urgency. In: Fink M.P., Abraham E., Vincent J.-L., et al. Textbook of Critical Care. 5th ed. Philadelphia: Saunders; 2005:879–888.
4 Kitiyakara C., Guzman N.J. Malignant hypertension and hypertensive emergencies. J Am Soc Nephrol. 1998;9:133–142.
5 Lange R.A., Hillis L.D. Cardiovascular complications of cocaine use. N Engl J Med. 2001;345:351–358.
6 Pohl M.A. Renal artery stenosis, renal vascular hypertension, and ischemic nephropathy. In: Schrier R.W., ed. Diseases of the Kidney. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2001:1399–1457.
7 Qureshi A.I. Acute hypertensive response in patients with stroke: pathophysiology and management. Circulation. 2008;118:176–187.
8 Qureshi A.I., Ezzeddine M.A., Nasar A., et al. Prevalence of elevated blood pressure in 563,704 adult patients with stroke presenting to the ED in the United States. Am J Emerg Med. 2007;25:32–38.
9 Vaughan C.J., Delanty N. Hypertensive emergencies. Lancet. 2000;356:411–417.