19 Hypertension
The cardiovascular complications associated with hypertension are shown in Box 19.1. The most common and important of these are stroke and myocardial infarction. An increase of 5 mmHg in usual diastolic blood pressure is associated with a 35–40% increased risk of stroke. There is a similar but less steep association for coronary heart disease risk. The risk of heart failure is increased six-fold in hypertensive subjects. Meta-analysis of clinical trials has indicated that these risks are reversible with relatively modest reductions in blood pressure of 10/6 mmHg associated with a 38% reduction in stroke and 16% reduction in coronary events (Collins et al., 1990), while a 5 mmHg reduction in blood pressure is associated with a 25% reduction in risk of renal failure.
The absolute benefits of blood pressure lowering achieved as a result of these relative risk reductions depend on the underlying level of risk in an individual. High-risk subjects gain more benefit in terms of events saved per year of therapy. Absolute risk is highest in those who already have evidence of cardiovascular disease, such as previous myocardial infarction, transient ischaemic attack or stroke, or who have other evidence of cardiovascular dysfunction such as electrocardiogram (ECG) or echocardiograph abnormality. Risk is also increased in the elderly and in people with diabetes or renal failure and is further enhanced by other risk factors such as smoking, dyslipidaemia, obesity and sedentary lifestyle. In those under the age of 75, men are at greater risk than women. Cardiovascular risk in an individual who has no current cardiovascular disease can be estimated from coronary risk prediction charts (Joint British Societies, 2005; see Chapter 24).
Epidemiology
In 90–95% of cases of hypertension, there is no underlying medical illness to cause high blood pressure. This is termed ‘essential’ hypertension, so named because at one time it was erroneously believed to be an ‘essential’ compensation mechanism to maintain adequate circulation. The precise aetiology of essential hypertension is currently unknown. Genetic factors clearly play a part as the condition clusters in families, with hypertension being twice as common in subjects who have a hypertensive parent. Genetic factors account for about one-third of the blood pressure variation between individuals, although no single gene appears to be responsible except in some rare conditions such as polycystic kidney disease and other metabolic conditions such as Liddle’s syndrome (Beevers et al., 2001). The remaining 5–10% of cases are secondary to some other disease process (Box 19.2).
Management of hypertension
In the UK, the management of hypertension is guided by consensus guidelines produced by the British Hypertension Society (BHS) and the National Institute for Health and Clinical Excellence (NICE). In 2004, there were significant differences between NICE and BHS guidance but these were addressed in the form of modified joint guidance issued in 2006 which specifically addressed the areas of controversy (National Collaborating Centre for Chronic Conditions: Hypertension, 2006). The European Society of Hypertension also published a task force discussion document in January 2009 and formal guidance in 2007 (Mancia et al., 2009).
Assessment of the hypertensive patient
Contributing factors
The patient should also be assessed for possible contributory factors to hypertension such as obesity, excess alcohol or salt intake and lack of exercise. Occasionally, hypertension may be provoked by the use of drugs (see Box 19.2), including over-the-counter medicines used as cold and flu remedies. Other risk factors should also be documented and addressed, for example, smoking, diabetes and hyperlipidaemia. It is important to establish whether there is a family history of cardiovascular disease.
Determination of cardiovascular risk
An accurate assessment of cardiovascular disease risk is essential before recommending appropriate management in hypertension. Patients with documented atheromatous vascular disease, for example, previous myocardial infarction or stroke, angina or peripheral vascular disease are at high risk of recurrent events. Those with type 2 diabetes over 40 years of age are also at high risk and can be regarded as ‘coronary equivalents’, that is, with risks similar to non-diabetic patients with previous myocardial infarction. For non-diabetic patients without vascular disease it is necessary to estimate cardiovascular risk (see Chapter 24). A 10-year cardiovascular disease risk of 20% (equivalent to a 15% coronary heart disease risk) is regarded as an appropriate threshold for antihypertensive therapy in patients with moderate hypertension, as well as for lipid-lowering therapy. Treatment decisions based on these tables will favour treatment in elderly subjects. While a younger patient may be at lower absolute risk over 10 years and may not meet the criteria for blood pressure and lipid treatment, they may be at higher lifetime and longer term risk of premature death and vascular disease and, thus, still merit risk factor intervention.
Other factors to consider include microalbuminuria which increases cardiovascular risk by a factor of 2–3 and the combination of reduced GFR and microalbuminuria may increase risk by as much as six-fold (Cirillo et al 2008; Sehestedt et al., 2009).
Treatment
Non-pharmacological approaches
Non-pharmacological management of hypertension is important, although the effects are often disappointing. Patients with mild hypertension in the range 140–159/90–100 mmHg can be assessed for levels of risk while offered lifestyle advice. General health education is important to allow patients to make informed choices about management. In order to maximise potential benefit, patients should receive clear and unambiguous advice, including written information they can digest in their own time. Written advice for patients can be downloaded from the BHS website (http://www.bhsoc.org/).
In patients who are overweight, weight loss results in reduction in blood pressure of about 2.5/1.5 mmHg/kg. The DASH diet (Dietary Approaches to Stop Hypertension) was evaluated in a clinical trial and found to lower blood pressure significantly (4.5/2.7 mmHg) compared with a typical US diet. This diet emphasises fruit, vegetables, and low-fat dairy produce in addition to fish, low-fat poultry and whole grains while minimising red meat, confectionary and sweetened drinks (Appel et al., 1997). Subjects should reduce their salt intake, for example, by not adding salt to food on the plate. A daily sodium intake of <100 mmol (i.e. 6 g sodium chloride or 2.4 g elemental sodium) should be the aim. There is a significant amount of hidden salt in processed meat, ready meals, cheese and even bread. A dietary assessment may be required to accurately quantify a patient’s salt intake and advise on how reductions might be made.
Drug treatment
Treatment thresholds
Treatment thresholds are summarised in Table 19.1. Lifestyle advice should be provided to all patients with any degree of hypertension. Patients with severe hypertension (>220/120 mmHg confirmed on several readings on the same occasion) should be treated immediately and some guidance suggests that dual therapy should be commenced immediately in patients with blood pressure >20 mmHg above their target as monotherapy is unlikely to be fully effective (Mancia et al., 2007). Patients with blood pressures in the range 160–220/100–120 mmHg should be monitored over several weeks and treated if blood pressure remains in this range. The period of observation before starting treatment depends on the severity of the hypertension and the presence or absence of end-organ damage (see Table 19.1). Patients whose blood pressure is in the range 140–159/90–99 mmHg should be observed annually unless they have evidence of target organ damage, cardiovascular complications, diabetes or a calculated cardiovascular risk >20% over 10 years, in which case drug treatment should be offered. Patients with blood pressure in the range 135–139/85–89 mmHg should be reassessed annually, while those with blood pressure lower than this can be rechecked every 5 years.
| Initial blood pressure | Management | |
|---|---|---|
| Systolic (mmHg) | Diastolic (mmHg) | |
| Malignant hypertension | Admit and treat immediately | |
| >220 | >120 | Repeat several times at the same attendance and treat immediately if blood pressure persists in this range |
| 180–219 | 110–119 | Confirm over 1–2 weeks and treat if blood pressure remains in this range |
| 160–179 | 100–109 | Repeat over 3–4 weeks (end-organ damage present) or 2–12 weeks (no end-organ damage), institute non-pharmacological measures and treat if blood pressure persists in this range |
| 140–159 | 90–99 | Repeat over several weeks. Institute non-pharmacological measures. Treat if remains in this range and patient has target organ damage, cardiovascular complications or an estimated 10-year cardiovascular risk >20%. Otherwise reassess annually |
| 135–139 | 85–89 | Reassess annually |
| <135 | <85 | Reassess in 5 years |
Target blood pressures
Within the Hypertension Optimal Treatment (HOT) study (Hansson et al., 1998), patients were allocated diastolic target blood pressures of <90, 85, 80 mmHg. The study struggled to stratify patients effectively into these treatment groups but analysis suggested that the optimum target blood pressure was <140/85 mmHg with little benefit in lowering to lower levels of 120/70 mmHg but also little evidence of harm.
The UK Prospective Diabetes Study Group (1998a,b) suggested ‘tight’ blood pressure control was better than less tight in patients with non-insulin-dependent diabetes. The targets in the UK Prospective Diabetes Study were ‘tight’ <150/85 mmHg and ‘less tight’ <180/105 mmHg but the actually achieved blood pressures were lower, for example, 154/87 mmHg versus 144/82 mmHg. Recommendations in diabetics have, therefore, suggested treating to a target of 140/80 mmHg or less, although few studies have successfully lowered blood pressure to these levels.
A more recent study (Cardio-Sis) randomised non-diabetic subjects with systolic blood pressure >150 mmHg to target systolic blood pressure of <140 or <130 mmHg (Verdecchia et al., 2009). The primary end-point was left ventricular hypertrophy though the secondary end-point of a composite cardiovascular end-point was reduced (as well as the primary end-point) in the 130-mmHg group, with no increase in adverse events. This, however, is not robust enough evidence to recommend a reduction in blood pressure target levels and would require a larger study of hard clinical end-points to confirm these findings.
Achievement of target blood pressures is incorporated as a quality indicator for the General Medical Services Contract for primary care doctors in the UK. Diabetic patients are an exception and benefit from more aggressive blood pressure reduction. Target blood pressures for diabetic and non-diabetic subjects are summarised in Table 19.2. It should be emphasised that the audit standard will not be achieved in all patients.
Table 19.2 Target clinic blood pressures according to British Hypertension Society guidelines 2004 (Williams et al., 2004)
| Clinic blood pressure | ||
| No diabetes (mmHg) | Diabetes (mmHg) | |
| Optimal treated blood pressure | <140/85 | <130/80 |
| Audit standard | <150/90 | <140/80 |
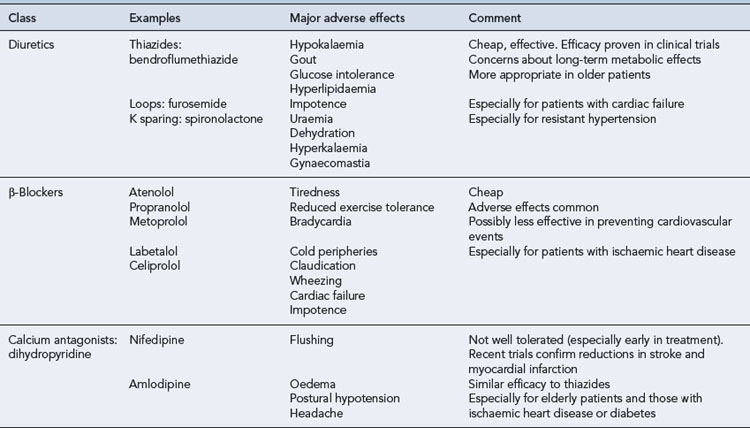
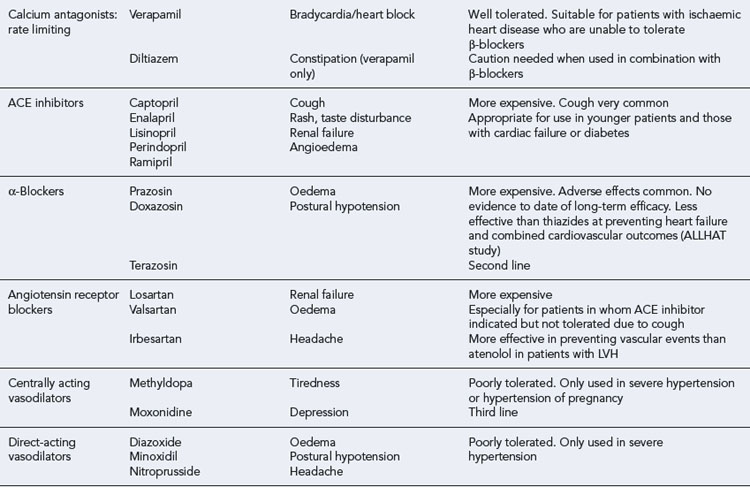
Antihypertensive drug classes
β-Adrenoreceptor antagonists
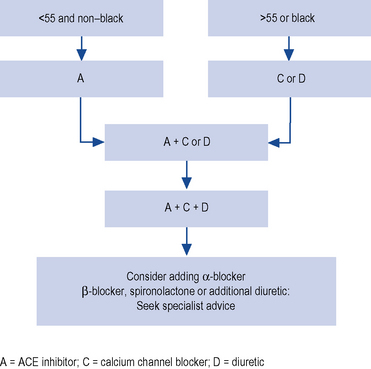
β-Adrenoreceptor antagonists also have substantial clinical trial evidence of benefit over placebo in hypertension, and are relatively inexpensive. However, their use is declining and they have been relegated to fourth-line therapy in the UK according to NICE guidance (Fig. 19.1). This recommendation largely stems from the evidence that they may be less effective at preventing stroke in conjunction with their diabetogenic effects. The Losartan For Endpoint reduction in hypertension (LIFE) study compared an atenolol/thiazide-based regime with a losartan-based regime and demonstrated equivalent levels of blood pressure reduction but with a small excess incidence of stroke in the atenolol arm (Dahlöf et al., 2002). In the Anglo Scandinavian Cardiac Outcomes Trial (ASCOT) study, the risk of diabetes was 2.5% higher in the atenolol arm compared with the amlodipine arm with similar increased risk of diabetes found within the atenolol arm of the LIFE study (Dahlöf et al., 2005). A Cochrane review warned of the excess risk in developing diabetes in patients prescribed combinations of thiazide diuretics and β-blockers. This would equate to one new case per 500 treated (Mason et al., 2004). The combination of thiazide and a β-blocker should, therefore, be avoided if possible, particularly in those who are at risk of developing diabetes (e.g. obese, strong family history of diabetes, South Asian origin).
To complicate matters, however, a long-term 20-year follow-up study of the UKPDS study found similar cardiovascular outcomes between patients on β-blockers and ACE inhibitors with a reduction in all causes of mortality which actually favoured β-blockers (Holman et al., 2008). β-Blockers do remain most suitable for younger hypertensives who have another indication for β-blockade, such as coronary heart disease. β-Blockers are also effective in suppressing atrial fibrillation and this may be one group of patients where first-line therapy with β-blockers is still merited.
Diuretics
Most blood pressure lowering occurs with very low doses of thiazide diuretics. Increasing the dose substantially increases the risk of metabolic disturbance without causing further blood pressure reduction. For bendroflumethiazide it is rarely (if ever) appropriate to use doses greater than 2.5 mg/day and a dose of 1.25 mg daily is often effective. Most studies of diuretics have also incorporated β-blockers and this combination can have adverse metabolic consequences which may lead to new onset diabetes. Within the Anti-hypertensive and Lipid Lowering treatment to prevent Heart Attack Trial (ALLHAT), the absolute risk of developing diabetes was 3.5% higher in the chlortalidone group than the lisinopril group (ALLHAT Collaborative Research Group, 2002).
Calcium channel blockers
Although effective for lowering blood pressure and preventing cardiovascular events, adverse effects are common, for example, oedema and flushing. Gum hypertrophy may occur with dihydropyridines and constipation with verapamil. Concerns have previously been raised by observational studies (Psaty et al., 1995) and meta-analysis (Furberg et al., 1995) that there may be an increased risk of coronary heart disease in recipients of dihydropyridine calcium channel blockers. However, randomised clinical trials have not confirmed these observations (Gong et al., 1996, Staessen et al., 1997) and have indicated that dihydropyridines are of similar efficacy to thiazide diuretics in preventing cardiovascular events (Brown et al., 2000).
α-Adrenoreceptor blockers
Drugs of this class antagonise α-adrenoceptors in the blood vessel wall and, thus, prevent noradrenaline (norepinephrine)-induced vasoconstriction. As a result, they reduce total peripheral resistance and blood pressure. Prazosin was originally used but had the disadvantage of being short-acting and causing first-dose hypotension. Newer agents such as doxazosin and terazosin have a longer duration of action. There are concerns about the first-line use of β-blockers since the ALLHAT study has indicated that doxazosin is more often associated with heart failure and stroke than thiazide diuretics (ALLHAT Collaborative Research Group, 2000). However, they are an appropriate choice as add-in therapy for patients inadequately controlled using other agents. They can frequently cause postural hypotension but may alleviate symptoms in men with prostatic hyperterophy.
Other agents
Recent additions to the licensed armory of antihypertensive agents include the renin antagonist aliskiren. There is evidence that this agent may have a similar blood pressure lowering effect to other agents and may be safely added to other inhibitors of the renin–angiotensin–aldosterone system to provide a greater level of inhibition (O’Brien et al., 2007). Due to its cost and a relative lack of experience in its use, it can only be suggested as an add-on therapy where other more established treatment options have failed to control blood pressure. It is generally well tolerated but may cause diarrhoea at higher doses.
The endothelin antagonist darusentan is undergoing clinical trials in resistant hypertension. Early studies show it may be effective in resistant cases but may be associated with a high incidence of fluid retention (Weber et al., 2009).
Drug selection
Drugs should be chosen on the basis of efficacy, safety, convenience to the patient and cost. For assessing efficacy, it is essential to use evidence from large-scale clinical trials that demonstrate measurable effects on hard end-points like incidence of stroke and other cardiovascular events or death. Smaller scale studies looking at the effects of drugs on blood pressure and surrogate markers such as left ventricular hypertrophy or carotid artery stenosis may generate a hypothesis of a future treatment strategy but should be used to change current strategies. When considering safety, it is important to recognise that these drugs will be taken in the long term and there are advantages to using drugs which have long-established safety records. It is also important to recognise the importance of symptomatic adverse effects since these may reduce adherence. Patients should feel as well during treatment of their blood pressure as they did before drug treatment was instituted. Patient convenience is another important factor and use of once-daily preparations will result in better adherence than more frequent regimens. Since the hypertensive population is very large it is necessary to be conscious of the cost of individual preparations. Combinations of low doses of antihypertensive drugs are often better tolerated than single drugs taken in high dose. The choice of drugs available for treating hypertension is shown in Table 19.3, and common therapeutic problems are noted.
Clinical trial evidence
The Blood Pressure Lowering Treatment Trialists Collaboration (2000) carried out a meta-analysis of old against new treatments. They concluded that newer treatments were no more effective than older therapies. Since this study was done several landmark comparative clinical trials have been published.
The Captopril Prevention Project (CAPPP) demonstrated that captopril was as effective as diuretics or β-blockers for preventing cardiovascular morbidity (Hansson et al., 1999a). However, captopril was associated with a 25% higher stroke risk, perhaps because it did not reduce blood pressure as effectively as conventional therapy in this particular study.
The LIFE study demonstrated that losartan was more effective at preventing vascular events, especially stroke, than atenolol in just over 9000 hypertensive patients with left ventricular hypertrophy, although reductions in blood pressure were similar. Losartan was also better tolerated (Dahlöf et al., 2002).
The ALLHAT study (ALLHAT Collaborative Research Group, 2002) involved over 40,000 older, high-risk hypertensive patients with the aim of determining whether the occurrence of fatal coronary heart disease or non-fatal myocardial infarction was lower in those treated with newer agents (amlodipine, lisinopril or doxazosin) compared with a thiazide-like diuretic (chlortalidone). The doxazosin arm was discontinued early because of a higher rate of events, especially heart failure, compared with the diuretic. For the remaining three drugs there was no difference in occurrence of the primary end-point. Chlortalidone was more effective than amlodipine and lisinopril in lowering blood pressure and preventing heart failure and was also marginally more effective than lisinopril in preventing stroke.
The second Australian National Blood Pressure Study Group (Wing et al., 2003) compared enalapril with hydrochlorthiazide in just over 6000 hypertensive subjects recruited in primary care. The primary end-point was any cardiovascular event or death from any cause. In this relatively small study, there was a trend in favour of the ACE inhibitor which was of borderline statistical significance.
The VALUE study (Julius et al., 2004) compared amlodipine and valsartan in high-risk hypertensive subjects. No differences in the primary composite cardiac end-point were observed, although non-fatal myocardial infarction was less common with amlodipine, which also lowered blood pressure to a greater extent. Conversely, onset of diabetes was less common with valsartan.
The ASCOT study (Dahlöf et al., 2005) compared a modern treatment regimen based on amlodipine and perindopril with a traditional regimen based on atenolol and bendroflumethiazide. The study involved over 20,000 high-risk hypertensives. The amlodipine-based therapy was associated with better blood pressure reduction and reductions in the occurrence of cardiovascular events, total mortality and diabetes, although the primary composite end-point was not significantly affected. It is uncertain how much of the benefit can be attributed to the better blood pressure control achieved in the amlodipine-based arm and how specific these findings are to the drug doses and sequencing specified in the trial protocol for each arm of the study.
These various trials have provided results that are conflicting, in part because of differences in trial design and quality. However, there is increasing evidence that β-blockers may be less effective at preventing cardiovascular end-points, as suggested by LIFE and ASCOT studies. In a meta-analysis (Lindholm et al., 2005), β-blockers were less effective than other antihypertensives at preventing stroke, although no significant differences were observed in effects on myocardial infarction or death. There is no consistent evidence that thiazides or thiazide-like drugs are less effective than newer agents in preventing cardiovascular events.
Recommendations for drug sequencing
In the UK, the BHS and NICE issued joint guidelines in 2006 on the order in which drugs should be used (National Collaborating Centre for Chronic Conditions, 2006). This replaced previous guidelines which differed between the two reflecting the ongoing controversy regarding the role of β-blockers. These recommend an initial choice of an ACE inhibitor or ARB (A) as first-line therapy in younger (<55 years) non-black patients. The rationale for this is that these patients often have hypertension associated with high concentrations of renin. It is, therefore, logical to treat these patients with drugs that antagonise the renin–angiotensin system.
For patients >55 and black patients, who tend to have hypertension associated with low renin concentrations, calcium channel blockers (C) or thiazide diuretics (D) are advocated as first-line options. If initial drug therapy fails to control blood pressure, A and D or C is suggested. Subsequently, a combination of A plus C plus D may be used. After this, further therapies, for example, β-blocker, α-blocker, spironolactone, etc., could be added as necessary to achieve adequate control (Fig. 19.1). β-Blockers may be used in those patients with a high sympathetic drive, in pregnant women where labetolol has a good safety record or where other agents are not tolerated.
European guidance (Box 19.3) has eschewed a formal ranking of treatments and instead suggested a table of drugs and indications where they might be most appropriately indicated (Mancia et al., 2007).
Special patient groups
Elderly
The elderly have a high prevalence of hypertension, with over 70% having blood pressures greater than 140/90 mmHg. They are also at high absolute risk of cardiovascular events. Therefore, the absolute benefits of blood pressure treatment are particularly large in this group. Antihypertensive therapy may also reduce the risk of heart failure and dementia. The Study of Cognition and Prognosis in the Elderly (SCOPE) study (Lithell et al., 2003) was designed to investigate the effects of candesartan on the occurrence of cognitive decline or dementia but revealed no benefit, probably because of the lack of difference in blood pressure between the two arms of the study
The elderly are at particular risk of certain adverse effects of treatment such as postural hypotension and it is important that both sitting and standing blood pressure are monitored. Nevertheless, the benefits of therapy are so great that treatment should be offered at any age unless the patient is very frail or their life expectancy is very short. Isolated systolic hypertension (systolic >160 mm Hg, diastolic <90 mmHg) is common in the elderly and there is irrefutable evidence that drug treatment is beneficial in this group (SHEP Co-operative Research Group, 1991, Staessen et al., 1997). The elderly have more variable blood pressure and larger numbers of measurements may be required to confirm hypertension.
Calcium channel blockers and low-dose thiazide diuretics are safe and effective treatments for elderly hypertensive people and their use is endorsed by large-scale clinical trials. β-Blockers are less effective at reducing blood pressure and preventing clinical end-points. The Swedish Trial in Old Patients with hypertension-2 (STOP-2) compared the effects of conventional (β-blocker or thiazide) and newer drugs (ACE inhibitors or calcium channel blockers) on cardiovascular morbidity in older subjects and did not detect significant differences (Hansson et al., 1999b).
In the Hypertension in the Very Elderly Trial (HYVET), 4000 patients with a mean age of 84, blood pressure 160–199 mmHg systolic at entry were treated to a target of systolic 150 mmHg for 1.8 years with indapamide (a thiazide-like diuretic) and if required the ACE inhibitor perindopril. There was a 30% reduction in fatal and non-fatal stroke, 21% reduction in death from all causes, and fewer adverse events in the actively treated group (Beckett, 2008).
The elderly certainly benefit from treatment of hypertension but the threshold and target for treatment has not been fully elucidated. Most studies in the elderly recruited patients with relatively high baseline targets (>160–190 mmHg systolic) achieving blood pressure on treatment of between 150 and 170 mmHg and only one achieved target blood pressure lower than 140 mmHg and in this study outcome was poorer in the treated group (JATOS Study Group, 2008). There may be little benefit in striving for strict systolic targets beyond 150 mmHg in these patients, particularly if control is being achieved to the detriment of overall patient well-being.
Diabetes
In type 2 (non-insulin dependent) diabetes, hypertension is particularly common, affecting 70% of people in this group. It is strongly associated with obesity and insulin resistance and control of blood pressure is more important for preventing complications than tight glycaemic control. There is no evidence that one group of drugs is more or less effective than any other. The ADVANCE trial treated diabetics with indapamide and perindopril in addition to prestudy antihypertensive agents. The active group was found to have a further reduction in blood pressure and a significant reduction in adverse renal outcomes (21%) (Patel et al., 2007). It remains a subject of debate whether ACE inhibitors and ARBs have specific renoprotective benefits over and above their effects on blood pressure.
Renal disease
A further note of caution regarding overtreatment of blood pressure to overaggressive targets comes from the ONTARGET study which randomised patients with vascular disease or high-risk diabetics to high-dose ramipril, telmisartan (ARB) or both. Many patients were already taking polypharmacy for hypertension and blood pressures at entry were approximately 142/82 mmHg in all groups. Treatment reduced blood pressure by 6.4/4.3 mmHg in the ramipril group, 7.4/5.0 mmHg in the telmisartan group and 9.8/6.3 mmHg in the combination group. This would give the combination group a post-treatment blood pressure of 132/76 mmHg. This combination group was associated with adverse renal outcomes, for example, renal failure and high potassium with no improvement in other cardiovascular outcomes (Yusuf et al., 2008a).
Stroke
Hypertension is the most important risk factor for stroke in patients with or without previous stroke. There is increasing evidence that in those with a previous stroke, blood pressure reduction reduces the risk of stroke recurrence as well as other cardiovascular events. The PROGRESS study, while clearly demonstrating a benefit of lowering blood pressure in patients with cerebrovascular disease, only demonstrated benefit in those whose blood pressure was >140 mmHg on entry or who were already on antihypertensives. The size of benefit was proportional to the size of the blood pressure reduction. The combination of perindopril and indapamide lowered systolic blood pressure by 12.3 mmHg and stroke incidence by an impressive 43%, while perindopril alone was associated with a small drop in systolic blood pressure and no reduction in stroke risk (PROGRESS Collaborative Group, 2001). On treatment, blood pressure in the actively treated group was 132 mmHg systolic which has led some to suggest a target of 130 mmHg for such patients but this is based on post hoc analysis and has not been recommended in formal guidance.
The PROFESS study randomised patients with cerebrovascular disease to telmistartan or placebo and obtained systolic blood pressure of 136 in the active group versus 140 mmHg in the placebo group with no difference in the vascular outcomes between the two groups. This may have been due to the relatively small difference in blood pressure between the two groups (Yusuf et al., 2008b).
The question ‘what to do with blood pressure in the setting of acute stroke?’ has remained an evidence-free zone until fairly recently. Blood pressure naturally rises then falls in the days and hours following acute stroke and some have argued that elevated levels are necessary to maintain brain circulation due to the failure of cerebral autoregulatory mechanisms around the time of stroke. The theory that lowering blood pressure could reduce cerebral perfusion due to a lack of the usual autoregulatory mechanisms is counterweighted by the potential for further damage due to cerebral oedema. The Control Hypertension and Hypotension Immediately Poststroke Study (CHHIPS) randomised acute stroke patients to placebo, lisinopril (sublingual) or intravenous bolus of labetolol and evaluated the incidence of neurological deterioration. There was no adverse outcome in any actively treated group despite reductions in blood pressure (21 vs. 11 mmHg for systolic blood pressure; Potter et al., 2009) This was a relatively small study and larger confirmatory studies are required before firm recommendations for patient management should be made.
In patients with intracerebral haemorrhage, acute reduction of blood pressure has also been demonstrated to be feasible and probably safe with reduced haematoma growth in the actively treated group (Anderson et al., 2008).
Hormone replacement therapy
A list of the indications and contraindications to the various antihypertensive agents can be found in Table 19.4.
Table 19.4 Use of antihypertensive drugs adapted from British Hypertension Society guidelines
| Class | Indications | Contraindications |
|---|---|---|
| Diuretics | Elderly | Gout |
| ISH | ||
| Heart failure | ||
| Secondary stroke prevention | ||
| β-Blockers | Myocardial infarction | Asthma/chronic obstructive pulmonary disease |
| Angina | Heart block | |
| (Heart failure) | (Heart failure) | |
| (Dyslipidaemia) | ||
| (Peripheral vascular disease) | ||
| (Diabetes, except with coronary heart disease) | ||
| Calcium antagonists: dihydropyridine | Elderly isolated systolic hypertension | |
| (Elderly) | ||
| (Angina) | ||
| Calcium antagonists (rate limiting) | Angina | Combination with β-blocker |
| (Myocardial infarction) | (Heart block) | |
| (Heart failure) | ||
| ACE inhibitors | Heart failure | Pregnancy |
| Left ventricular (LV) dysfunction | Renovascular disease | |
| Type 1 diabetic nephropathy | (Renal impairment) | |
| Secondary stroke prevention | (Peripheral vascular disease) | |
| (Chronic renal disease) | ||
| (Type 2 diabetic nephropathy) | ||
| (Proteinuric renal disease) | ||
| α-Blockers | Benign prostatic hypertrophy | Urinary incontinence |
| (Dyslipidaemia) | (Postural hypotension) | |
| (Heart failure) | ||
| Angiotensin receptor blockers | ACE inhibitor intolerance | As ACE inhibitors |
| Type 2 diabetic nephropathy | ||
| Hypertension with LVH | ||
| Heart failure in ACE inhibitor-intolerant subjects | ||
| Post-MI | ||
| (LV dysfunction post-MI) | ||
| (Intolerance of other antihypertensive drugs) | ||
| (Proteinuric renal disease) | ||
| (Chronic renal failure) | ||
| (Heart failure) | ||
| Centrally acting vasodilators | Pregnancy (methyldopa only) | |
| Resistant hypertension unresponsive to first-line therapy | ||
| Direct-acting vasodilators | Resistant hypertension, unresponsive to first-line therapy |
Note: Strong indications and contraindications are shown. Text in parentheses indicates weak/possible indications or contraindications.
Ancillary drug treatment
Aspirin
Blood pressure should be controlled (<150/90 mmHg) before aspirin is instituted.
Lipid-lowering therapy
There is increasing evidence from clinical trials of the benefit of lipid-lowering drug treatment in patients with hypertension. For example, in the ASCOT study lipid-lowering arm (ASCOT-LLA), treatment with atorvastatin 10 mg was associated with substantial reductions in coronary heart disease and stroke, in spite of the fact that those with total cholesterols initially higher than 6.5 mmol/L were excluded from the study (Sever et al., 2003). Lipid-lowering therapy, usually with a statin, should be prescribed to patients under 80 years of age with a total cholesterol >3.5 mmol/L who either have pre-existing vascular disease or a 10-year cardiovascular risk of >20%.
Answers
Questions
Answers
Answers
Answers
Answer
There is no good evidence that antihypertensive drug treatment is beneficial in the early stages of acute stroke and there is a risk that lowering blood pressure may compromise cerebral perfusion further. However, in the longer term, blood pressure reduction is valuable for preventing further strokes and other cardiovascular events. It would be appropriate to monitor the blood pressure and start treatment after a few days if it remains persistently elevated. A thiazide diuretic and/or ACE inhibitor are commonly used under these circumstances, following the demonstration of benefit in the PROGRESS study (PROGRESS Collaborative Group, 2001).
ALLHAT Collaborative Research Group. Major cardiovascular events in hypertensive patients randomised to doxazosin vs. chorthalidone. Antihypertensive and lipid lowering treatment to prevent heart attack trial (ALLHAT). J. Am. Med. Assoc.. 2000;283:1967-1975.
ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: the antihypertensive and lipid lowering treatment to prevent heart attack trial (ALLHAT). J. Am. Med. Assoc.. 2002;288:2981-2997.
Anderson C.S., Yining H., Wang J.G., et al. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): a randomised pilot trial. Lancet Neurol.. 2008;7:391-399.
Appel L.J., Moore T.J., Obarzanek E., et al. A clinical trial of the effects of dietary patterns on blood pressure. N. Engl. J. Med.. 1997;336:1117-1124.
Beckett N.S., Peters R., Fletcher A.E., et al. Treatment of hypertension in patients 80 years of age or older. N. Engl. J. Med.. 2008;358:1887-1898.
Beevers G., Lip G.Y.H., O’Brien E. The pathophysiology of hypertension. Br. Med. J.. 2001;322:912-916.
Blood Pressure Lowering Treatment Trialists Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood pressure lowering drugs: results of prospectively designed overviews of randomized trials. Lancet. 2000;356:1955-1964.
Brown M.J., Palmer C.R., Castaigne A., et al. Morbidity and mortality in patients randomised to double blind treatment with a long acting calcium channel blocker or diuretic in the international nifedipine GITS study (INSIGHT). Lancet. 2000;356:366-372.
Cirillo M., Lanti M.P., Menotti A., et al. Definition of kidney dysfunction as a cardiovascular risk factor: use of urinary albumin excretion and estimated glomerular filtration rate. Arch. Int. Med.. 2008;168:617-624.
Collins R., Petro R., MacMahon S., et al. Blood pressure, stroke and coronary heart disease. Part 2. Short-term reductions in blood pressure: overview of randomised drugs trials in their epidemiological context. Lancet. 1990;335:827-838.
Dahlöf B., Devereux R., Kjeldsen S.E., et al. Cardiovascular morbidity and mortality in the Losartan For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359:995-1003.
Dahlöf B., Sever P.S., Poulter N.R., ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo Scandinavian Cardiac Outcomes Trial – Blood Pressure Lowering Arm (ASCOT–BPLA). Lancet. 2005;366:895-906.
Furberg C.D., Psaty B.M., Meyer J.V. Nifedipine: dose-related increase in mortality in patients with coronary heart disease. Circulation. 1995;92:1326-1331.
Gong L., Zhang W., Zhu Y., et al. Shanghai Trial Of Nifedipine in the Elderly (STONE). J. Hypertens.. 1996;14:1237-1245.
Hansson L., Lindholm L.H., Niskanen L., et al. Effect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension. The Captopril Prevention Project (CAPPP). Lancet. 1999;353:611-616.
Hansson L., Lindholm L.H., Ekbom T., et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity in the Swedish Trial in Old Patients with hypertension-2 study. Lancet. 1999;354:1751-1756.
Hansson L., Zanchetti A., Carruthers S.G., for the HOT Study Group. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the hypertension optimal treatment (HOT) randomised trial. Lancet. 1998;351:1755-1762.
Holman R.R., Paul S.K., Bethel M.A., et al. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N. Engl. J. Med.. 2008;359:1565-1576.
JATOS Study Group. Principal results of the Japanses trial to assess optimal systolic blood pressure in elderly hypertensive patients. Hypertens. Res.. 2008;31:2115-2127.
Joint British Societies. JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart. 2005;91:v1-v52.
Julius S., Kjeldsen S.E., Weber M., et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet. 2004;363:2022-2031.
Lindholm L.H., Carlberg B., Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366:1545-1553.
Lithell H., Hansson L., Skoog I., SCOPE Study Group. The Study of Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomised double-blind intervention trial. J. Hypertens.. 2003;21:875-1866.
Mancia G., de Backer G., Dominiczak A., et al. Guidelines for the management of arterial hypertension. The Task Force for the Management of Arterial Hypertension of the European Society of hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens.. 2007;25:1105-1187.
Mancia G., Laurent S., Agabiti-Rosei E., et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J. Hypertens.. 2009;27:2121-2158.
Mason J., Dickinson H., Nicolson D., et al. The diabetogenic potential of thiazide diuretics and beta-blocker combinations in the management of hypertension. Available at: http://www2.cochrane.org/colloquia/abstracts/ottawa/P-097.htm, 2004.
National Collaborating Centre for Chronic Conditions. Hypertension. In Management of hypertension in adults in primary care: partial update. London: Royal College of Physicians; 2006. Available at: http://www.nice.org.uk/page.aspx?o=CG034fullguideline
O’Brien E., Barton J., Nussberger J., et al. Aliskiren reduces blood pressure and suppresses plasma renin activity in combination with a thiazide diuretic, an angiotensin-converting enzyme inhibitor, or an angiotensin receptor blocker. Hypertension. 2007;49:276-284.
Patel A., MacMahon S., Chalmers J., et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370:829-840.
Potter J.F., Robinson T.G., Ford G.A., et al. Controlling hypertension and hypotension immediately post stroke (CHHIPS): a randomized, placebo-controlled, double-blind pilot trial. Lancet Neurol.. 2009;8:48-56.
PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood pressure lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033-1041.
Psaty B.M., Heckbert S.R., Kocpsell T.D., et al. The risk of myocardial infarction associated with antihypertensive drug therapies. J. Am. Med. Assoc.. 1995;274:620-625.
Sehestedt T., Jeppesen J., Hansen T.W., et al. Which markers of subclinical organ damage to measure in individuals with high normal blood pressure? J. Hypertens.. 2009;27:1165-1171.
Sever P.S., Dahlof B., Poulter N.R., et al. Prevention of coronary and stroke events with atorvastatin in patients who have average or lower-than-average cholesterol concentrations in the Anglo Scandinavian Cardiac Outcomes Trial – Lipid Lowering Arm. Lancet. 2003;361:1149-1158.
SHEP Co-operative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). J. Am. Med. Assoc.. 1991;265:3255-3264.
Staessen J.A., Fagard R., Thijs L., for the Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;350:757-764.
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. Br. Med. J.. 1998;317:703-713.
UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. Br. Med. J.. 1998;317:713-726.
Verdecchia P., Staessen J.A., Angeli F., on behalf of the Cardio-Sis investigators. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial. Lancet. 2009;374:525-533.
Weber M.A., Black H., Bakris G., et al. A selective endothelin-receptor antagonist to reduce blood pressure in patients with treatment-resistant hypertension: a randomised, double-blind, placebo-controlled trial. Lancet. 2009;374:1423-1431.
Williams B., Poulter N.R., Brown M.J., et al. Guidelines for the management of hypertension: report of the fourth working party of the British Hypertension Society, 2004 – BHS IV. J. Hum. Hypertens.. 2004;18:139-185. Reprinted by permission from Macmillan Publishers Ltd
Wing L.M.H., Reid C.M., Ryan P., et al. A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly. N. Engl. J. Med.. 2003;348:583-592.
Yusuf S., Teo K.K., Pogue J., et al. ONTARGET Investigators Telmisartan, ramipril, or both in patients at high risk for vascular events. N. Engl. J. Med.. 2008;358:1547-1559.
Yusuf S., Diener H.C., Sacco R.L., PRoFESS Study Group. Telmisartan to prevent recurrent stroke and cardiovascular events. N. Engl. J. Med.. 2008;359:1225-1237.
Brown M.J., Cruickshank J.K., Dominiczak A.F., et al. Better blood pressure control: how to combine drugs. J. Hum. Hypertens.. 2003;17:81-86.
Gradman A.H., Basile J.N., Carter B.L., et al. Combination therapy in hypertension. J. Am. Soc. Hypertens.. 2010;4:42-50.
Hollenberg N.K. Atlas of Hypertension, sixth ed. Philadelphia: Current Medicine; 2009.
Ljungman C., Mortensen L., Kahan T., et al. Treatment of mild to moderate hypertension by gender perspective: a systematic review. J. Womens Health. 2009;18:1049-1062.
Mancia G., Laurent S., Agabiti-Rosei E., et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J. Hypertens.. 2009;27:2121-2158.
Messerli F., Williams B., Ritz E. Essential hypertension. Lancet. 2007;370:591-603.
Mohler E.R., Townsend R.R. Advanced Therapy in Hypertension and Vascular Disease. Hamilton: BC Decker Inc; 2005.
Safar M., O’Rourke M. Arterial Stiffness in Hypertension. Oxford: Elsevier; 2006.