7 Hyperinflation Therapy
Note 1: This book is written to cover every item listed as testable on the Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE).
The listed code for each item is taken from the National Board for Respiratory Care (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and the WRE, it will be shown simply as: (Code: …). If an item is testable only on the ELE, it will be shown as: (ELE code: …). If an item is testable only on the WRE, it will be shown as: (WRE code: …).
MODULE A
1. Instruct the patient in deep-breathing techniques (Code: IIID1a) [Difficulty: ELE: R, Ap; WRE: An]
Teach the following cough techniques to the patient with obstructive airways disease:
2. Instruct the patient in inspiratory muscle training techniques (ELE code: IIID1b) [Difficulty: R, Ap]
Initially, teach the following steps to patients with obstructive airways diseases:
MODULE B
1. Instruct the patient in incentive spirometry techniques (Code: IIID1a) [Difficulty: ELE: R, Ap; WRE: An]
Because the goal of IS is to prevent or treat atelectasis, the patient should inhale a near-normal inspiratory capacity (IC). The patient can benefit more by holding the IC for several seconds, which is referred to as sustained maximal inspiration (SMI). Before the operation, the cooperative surgical patient should have the IC measured at the bedside or calculated from a pulmonary function test in which vital capacity (VC) is measured (review Chapter 4 for IC information). The IC is measured again postoperatively.
Monitor your patient’s progress in the following ways:
2. Increase or decrease the patient’s incentive spirometry goal (Code: IIIF2b) [Difficulty: ELE: R, Ap; WRE: An]
See Table 7-1 for IS guidelines. The following guidelines are also suggested:
| Postoperative Bedside Spirometry | Treatment Modality |
|---|---|
| IC >80% of the preoperative value | No treatment needed unless radiographic or clinical evidence of atelectasis exists. |
| IC at least 33% of the preoperative value or VC of at least 10 mL/kg | IS is indicated. |
| IC <33% of the preoperative value or VC <10 mL/kg | IPPB is indicated. |
IC, Inspiratory capacity; IPPB, intermittent positive-pressure breathing; IS, incentive spirometry; VC, vital capacity.
MODULE C
1. Manipulate incentive spirometry equipment by order or protocol (ELE code: IIA13) [Difficulty: R, Ap, An]
2. Get the necessary equipment, put it together, and make sure that it works properly
Two basic types of IS equipment exist: flow displacement and volume displacement units.
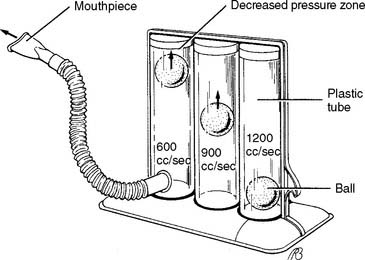
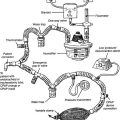
a. Flow displacement
With flow displacement units, patients breathe in a flow great enough to raise one or more plastic balls in calibrated cylinders (Figure 7-2). The patient is encouraged to try to keep the ball (or balls) suspended by breathing in more deeply. Encourage the patient to breathe in slowly to suspend the balls for as long as possible. Have the patient watch as the balls are held up by the inspired breath to provide positive reinforcement for doing a good job. The patient is not helped by breathing in a fast, short breath and having the balls pop up and down. Volume is calculated by multiplying the flow per second needed to suspend the balls by the number of seconds that the balls are suspended. For example, 600 cc/sec × 2 sec = 1200 cc IC. Assemble the device by attaching the flow tube to the unit and the mouthpiece to the flow tube.
b. Volume displacement units
With volume displacement units, patients breathe in a preset volume goal from the reservoir bellows (Figure 7-3). Many of these units have a whistle built into them to warn if the breath is too fast. Patients who cannot generate enough inspiratory flow to use a flow displacement unit should use a volume displacement unit instead.
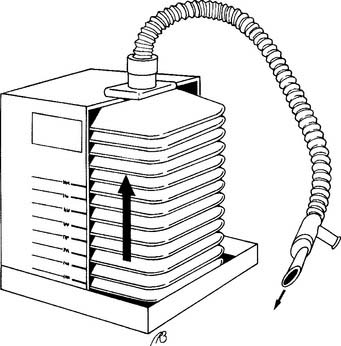
Figure 7-3 Volume incentive breathing exerciser.
(From Eubanks DH, Bone RC: Comprehensive respiratory care, ed 2, St Louis, 1990, Mosby.)
Assemble the device by attaching the flow tube to the unit and the mouthpiece to the flow tube.
MODULE D
1. Analyze the available information to determine the patient’s pathophysiologic state (Code: IIIH1) [Difficulty: ELE: R, Ap; WRE: An]
Review the information in Chapter 1 that deals with the interpretation of breath sounds and chest x-ray findings. As was discussed earlier, atelectasis is the primary problem that can be treated with IS.
2. Determine the appropriateness of the prescribed respiratory care plan and recommend modifications when indicated
a. Determine the appropriateness of the prescribed therapy and goals for the patient’s pathophysiologic state (Code: IIIH3) [Difficulty: ELE: R, Ap; WRE: An]
IS is the easiest and least expensive way to treat atelectasis if the patient can properly perform the procedure. See Table 7-1 for guidelines on the indications for IS or IPPB.
b. Review the planned therapy to establish the therapeutic plan (Code: IIIH2a) [Difficulty: ELE: R, Ap; WRE: An]
c. Recommend changes in the therapeutic plan when indicated (Code: IIIH4) [Difficulty: ELE: R, Ap; WRE: An]
The following should be considered when the patient’s response is evaluated:
d. Terminate the incentive spirometry treatment based on the patient’s response to therapy (Code: IIIF1) [Difficulty: ELE: R, Ap; WRE: An]
e. Recommend discontinuing the incentive spirometry treatment based on the patient’s response to therapy (Code: IIIG1i) [Difficulty: ELE: R, Ap; WRE: An]
Second, ineffective treatment may lead to treatment discontinuation. If the patient cannot perform a proper IS treatment (unconscious, physically unable to perform, inadequate inspiratory volume), another way to treat atelectasis should be found. This could include IPPB. (See Chapter 14 for the discussion.) The physician would order this change in therapy.
3. Respiratory care protocols
c. Explain planned therapy and goals to the patient in understandable (nonmedical) terms to achieve the best results from the treatment (Code: IIIA6) [Difficulty: ELE: R, Ap; WRE: An]
d. Monitor the outcome of the hyperinflation therapy protocol (Code: IIIH7b) [Difficulty: ELE: R, Ap; WRE: An]
e. Communicate the outcome of therapy and change the treatment based on the protocol (Code: IIIA5) [Difficulty: ELE: R, Ap; WRE: An]
Review Table 7-1 for guidelines on the use of incentive spirometry. These and the previous discussion on adjusting the IS goal can be used to develop and implement a protocol and evaluate its outcomes. It may be possible to use a simpler patient care plan such as cough and deep-breathing exercises with ambulation. Or, it may be necessary to switch to IPPB.
4. Record and evaluate the patient’s response to the treatment(s) or procedure(s) by doing the following:
a. Record and interpret the following: heart rate and rhythm, respiratory rate, blood pressure, body temperature, and pain level (Code: IIIA1b4) [Difficulty: ELE: R, Ap; WRE: An]
b. Record and interpret the patient’s breath sounds (Code: IIIA1b3) [Difficulty: ELE: R, Ap; WRE: An]
c. Record and interpret the type of cough the patient has and the nature of the sputum (Code: IIIA1b3) [Difficulty: ELE: R, Ap; WRE: An]
American Association for Respiratory Care. Clinical practice guideline: incentive spirometry. Respir Care. 1991;36(12):1402.
Cairo JM. Lung expansion devices. In Cairo JM, Pilbeam SP, editors: Mosby’s respiratory care equipment, ed 8, St Louis: Mosby, 2009.
Douce FH. Incentive spirometry and other aids to lung inflation. In Barnes TA, editor: Core textbook of respiratory care practice, ed 2, St Louis: Mosby, 1994.
Eubanks DH, Bone RC. Comprehensive respiratory care, a learning system, ed 2. St Louis: Mosby, 1990.
Fink JB. Bronchial hygiene and lung expansion. In: Fink JB, Hunt GE, editors. Clinical practice in respiratory care. Philadelphia: Lippincott Williams & Wilkins, 1999.
Fink JB. Volume expansion therapy. In: Burton GG, Hodgkin JE, Ward JJ, editors. Respiratory care: A guide to clinical practice. Philadelphia: Lippincott-Raven, 1997.
Fink JB, Hess DR. Secretion clearance techniques. In: Hess DR, MacIntyre NR, Mishoe SC, editors. Respiratory care principles & practice. Philadelphia: WB Saunders, 2002.
Johnson NT, Pierson DJ. The spectrum of pulmonary atelectasis: pathophysiology, diagnosis, and therapy. Respir Care. 1986;31:1107.
Mang H, Obermayer A. Imposed work of breathing during sustained maximal inspiration: comparison of six incentive spirometers. Respir Care. 1989;34:1122.
Rutkowski JA. Hyperinflation therapy. In: Wyka KA, Mathews PJ, Clark WF, editors. Foundations of respiratory care. Albany: Delmar, 2002.
Scuderi J, Olsen GN. Respiratory therapy in the management of postoperative complications. Respir Care. 1989;34:281.
Shapiro BA, Kacmarek RM, Cane RD, et al. Clinical application of respiratory care, ed 4. St Louis: Mosby, 1991.
Wilkins RL. Lung expansion therapy. In Wilkins RL, Stoller JK, Kacmarek RM, editors: Egan’s fundamentals of respiratory care, ed 9, St Louis: Mosby, 2009.
Wojciechowski WV. Incentive spirometers, secretion evacuation devices, and inspiratory muscle training devices. In Barnes TA, editor: Core textbook of respiratory care practice, ed 2, St Louis: Mosby, 1994.
SELF-STUDY QUESTIONS FOR THE ENTRY LEVEL EXAM See page 588 for answers
SELF-STUDY QUESTIONS FOR THE WRITTEN REGISTRY EXAM See page 613 for answers