Chapter 63 Hypercoagulable States
Table 63-3 Causes of Acquired Antithrombin Deficiency
| Decreased Synthesis | Increased Consumption | Enhanced Clearance |
|---|---|---|
| Hepatic cirrhosis | Major surgery | Heparin |
| Severe liver disease | Acute thrombosis | Nephrotic syndrome |
| l-asparaginase | Disseminated intravascular coagulation | |
| Severe sepsis | ||
| Multiple trauma | ||
| Malignancy | ||
| Prolonged extracorporeal circulation |
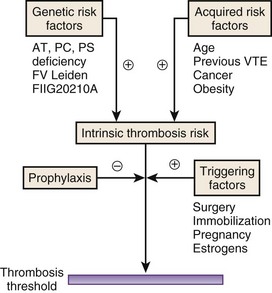
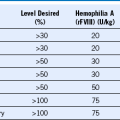
Figure 63-1 THROMBOSIS THRESHOLD.
(From Anderson JA, Weitz JI: Hypercoagulability and uncommon vascular diseases. In Jaff MR, White CJ, editors: Vascular disease: Diagnostic and therapeutic approaches, Minneapolis, Minn, 2011, Cardiotext Publishing.)
Figure 63-2 PROTEIN C PATHWAY.
(From Anderson JA, Weitz JI: Hypercoagulability and uncommon vascular diseases. In Jaff MR, White CJ, editors: Vascular disease: Diagnostic and therapeutic approaches, Minneapolis, Minn, 2011, Cardiotext Publishing.)
Table 63-4 Types of Inherited Protein C Deficiency
| Type | Antigen | Activity |
|---|---|---|
| I | Low | Low |
| II | Normal | Low |
Table 63-6 Features of Heparin-Induced Thrombocytopenia
| Feature | Details |
|---|---|
| Thrombocytopenia | Platelet count of 100,000/µl or less or a decrease in platelet count of 50% or more |
| Timing | Platelet count falls 5 to 10 days after starting heparin |
| Type of heparin | More common with unfractionated heparin than LMWH |
| Type of patient | More common in surgical patients than medical patients; more common in women than in men |
| Thrombosis | Venous thrombosis more common than arterial thrombosis |
Routine Investigations to Evaluate a Patient With (Venous) Thrombosis
| Test | Abnormality | Diagnostic Information |
|---|---|---|
| Complete blood count | Elevated hematocrit Increased white count Increased platelet count Leukopenia Thrombocytopenia |
Myeloproliferative disorder (e.g., essential thrombocythemia, polycythemia vera); may be found in paroxysmal nocturnal hemoglobinuria; if associated with heparin administration, consider heparin-induced thrombocytopenia |
| Blood film | Leukoerythroblastic film | Underlying neoplasm invading bone marrow |
| Liver function tests | Abnormal tests | May point to malignancy |
| Renal function | Impaired renal function | Assess prior to anticoagulation with heparin or LMWH |
| Urinalysis | Proteinuria | Nephrotic syndrome; may be associated with venous thromboembolism or renal vein thrombosis |
| PT and aPTT | Prolonged PT and aPTT | To enable safe anticoagulation to proceed if required Need to exclude lupus anticoagulant |
When to Perform a Thrombophilia Screen
Clinical Scenario
• First episode of unprovoked venous thromboembolism in individuals younger than 40 years of age
• Thrombosis in an unusual site (e.g., cerebral or mesenteric thrombosis)
• Two or more first-degree relatives with unprovoked thrombosis
• Females with a history of more than one second-trimester pregnancy loss or intrauterine death
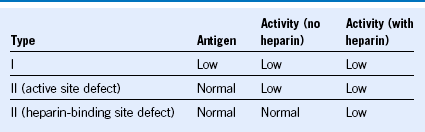
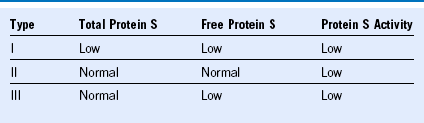
Essential Tests for Thrombophilia Screening
Functional assay for antithrombin: (with heparin to detect type II defects)
Functional assay for protein C
Functional assay for protein S: (immune assays for total and free protein S)
APC resistance assay: with genetic test for factor VLeiden for confirmation of abnormal results
Clinical Scenarios That Merit Long-Term Anticoagulation*
• Two or more unprovoked venous thrombotic events in less than 2 years, or within a relatively short space of time
• A single unprovoked thrombosis in an individual with antithrombin deficiency, APS, dual heterozygosity for the factor VLeiden and FIIG20210A gene mutations, or homozygosity for these mutations
• A single unprovoked massive or submassive pulmonary embolism
• An episode of venous thrombosis in a patient with active malignancy