Chapter 25 HYPERBILIRUBINEMIA
General Discussion
This discussion focuses on neonatal hyperbilirubinemia in infants 35 or more weeks of gestation.
Risk factors for neonatal hyperbilirubinemia are outlined below.
Causes of Hyperbilirubinemia
Hemolytic Causes (increased unconjugated bilirubin level, >6% reticulocytes, hemoglobin concentration of <13 g/dL)
Nonhemolytic causes (increased unconjugated bilirubin level, normal percentage of reticulocytes)
Key Historical Features
Risk Factors for Hyperbilirubinemia in Newborns
 Blood type ABO or Rh incompatibility
Blood type ABO or Rh incompatibility
 Ethnicity (Asian, Native American)
Ethnicity (Asian, Native American)
 Exclusive breastfeeding, particularly if nursing is not going well and weight loss is excessive
Exclusive breastfeeding, particularly if nursing is not going well and weight loss is excessive
 Birth trauma (cephalohematoma, cutaneous bruising, instrumented delivery)
Birth trauma (cephalohematoma, cutaneous bruising, instrumented delivery)
 Excessive weight loss after birth
Excessive weight loss after birth
 Gestational age (age 35-36 weeks is a major risk factor; age 37-38 weeks is a minor risk factor)
Gestational age (age 35-36 weeks is a major risk factor; age 37-38 weeks is a minor risk factor)
 Infections: toxoplasmosis, other agents, rubella, cytomegalovirus, herpes simplex (TORCH)
Infections: toxoplasmosis, other agents, rubella, cytomegalovirus, herpes simplex (TORCH)
 Jaundice observed before hospital discharge
Jaundice observed before hospital discharge
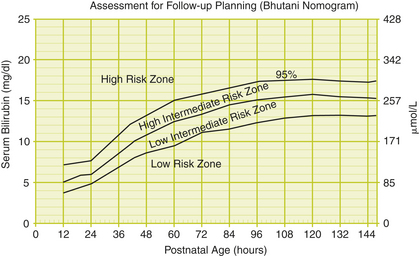
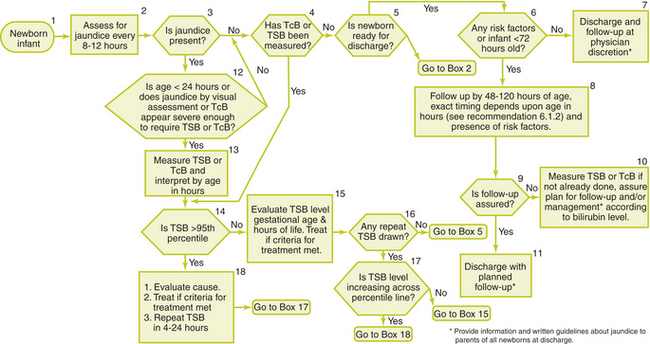
Suggested Work-Up
The suggested work-up for the jaundiced infant of 35 or more weeks’ gestation depends on the clinical picture and is outlined below. A transcutaneous bilirubin or total serum bilirubin measurement, or both, should be performed on every infant who is jaundiced in the first 24 hours after birth and in all infants in whom jaundice appears excessive for the infant’s age. If there is any doubt about the degree of jaundice, the transcutaneous bilirubin or total serum bilirubin should be measured. All bilirubin levels should be interpreted on a nomogram according to the infant’s age in hours (Figures 25-1 and 25-2). An algorithm for the management of jaundice is presented in Figure 25-3.
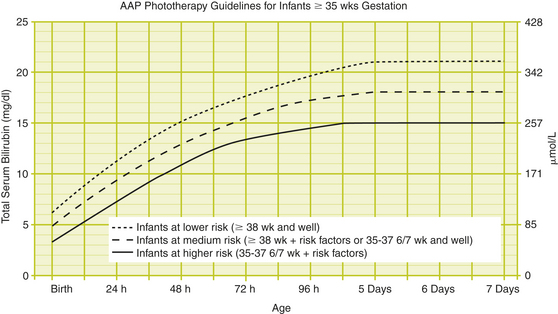
Figure 25-2 AAP Phototherapy Guidelines for Infants ≥35 weeks’ gestation.
(From Subcommittee on Hyperbilirubinemia, American Academy of Pediatrics. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114:297–316, with permission.)
| Jaundice in the First 24 Hours | |
| Measurement of transcutaneous bilirubin and/or total serum bilirubin | To determine bilirubin level and interpret on a nomogram according to the infant’s age in hours |
| Jaundice Appears Excessive for Infant’s Age | |
| Measurement of transcutaneous bilirubin and/or total serum bilirubin | To determine bilirubin level and interpret on a nomogram according to the infant’s age in hours |
| Infant Receiving Phototherapy or Total Serum Bilirubin is Rising Rapidly and Unexplained by History and Physical Examination | |
| Blood type and Coombs’ test if not obtained with cord blood | To evaluate for isoimmune hemolysis |
| Complete blood count (CBC) and smear | To evaluate for infection, evidence of hemolysis, or polycythemia |
| Direct (conjugated) bilirubin | To evaluate for causes of impaired bilirubin excretion |
| Consider: | |
| Reticulocyte count | To evaluate for hemolysis |
| G6PD assay | To evaluate for G6PD deficiency in infants whose family history or ethnic or geographic origin suggest the likelihood of G6PD deficiency |
| End Tidol Co (ETCO) if available | To evaluate for hemolysis |
| Repeat total serum bilirubin in 4 to 24 hours depending on infant’s age and total serum bilirubin level | |
| Total Serum Bilirubin Concentration Approaching Exchange Levels or Responding to Phototherapy | |
| Reticulocyte count | To evaluate for hemolysis |
| G6PD assay | To evaluate for G6PD deficiency |
| Albumin | To evaluate for hypoalbuminemia |
| ETCO if available | To evaluate for hemolysis |
| Elevated Direct (Conjugated) Bilirubin Level | |
| Urinalysis and urine culture Evaluate for sepsis if indicated by history and physical examination | To evaluate for UTI |
| Jaundice Present at or Beyond Age 3 Weeks, or Sick Infant | |
| Total and direct (conjugated) bilirubin level | To determine bilirubin level and evaluate for cholestasis |
| Check results of newborn thyroid and galactosemia screen | To evaluate for hypothyroidism and galactosemia |
Additional Work-Up
| Peripheral blood smear | If hemolysis is suspected |
| Red cell enzyme studies | If G6PD deficiency or pyruvate kinase deficiency is suspected |
| Hemoglobin electrophoresis | If hemoglobinopathy is suspected |
| Thyroid-stimulating hormong (TSH) | If hypothyroidism is suspected |
| Toxicology screen | If the history is suggestive of toxin exposure |
| Purified protein derivative (PPD) | If tuberculosis infection is suspected |
| Toxoplasmosis titers | If toxoplasmosis is suspected |
| Syphilis titers | If syphilis is suspected |
| Chromosomal analysis | If a chromosomal abnormality is suspected |
1. Bhutani V.K., Johnson L., Sivieri E.M. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics. 1999;103:6–14.
2. Dennery P.A., Seidman D.S., Stevenson D.K. Neonatal hyperbilirubinemia. N Engl J Med. 2001;344:581–590.
3. Porter M.L., Dennis B.L. Hyperbilirubinemia in the term newborn. Am Fam Physician. 2002;65:599–606.
4. Subcommittee on Hyperbilirubinemia. American Academy of Pediatrics. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316.