Chapter 6 Human Movement and Anterior Cruciate Ligament Function
Anterior Cruciate Ligament Deficiency and Gait Mechanics
INTRODUCTION
The anterior cruciate ligament (ACL) plays an important role in stability of the knee primarily through its passive constraint to anterior tibial translation and tibial rotation. In addition, the ACL influences the dynamic function of the knee. For example, ambulatory changes have been associated with functional adaptations after loss of ACL function. The nature of these functional adaptations may be considered a potential functional marker for the ability to return to vigorous activities3,28,29 as well as for secondary degenerative cartilage changes after ACL injury.7
The purpose of this chapter is
Differences in the manner in which patients adapt their gait characteristics to the loss of the ACL provide a possible explanation for the variable outcome after this injury. It is likely that some patients can dynamically adapt to the loss of an ACL, whereas others will not adapt. The large variation in treatment selection and outcome8,9 suggests a need for better methods of assessing the clinical and functional status of the patient after ACL rupture. Diagnostic methods for identifying a torn ACL have improved substantially; however, prognostic methods for assessing the probability of successful treatment are not yet available. Even quantitative laxity measurements obtained from devices such as the KT-1000 have not been predictive of clinical outcome.36 Thus, variability in dynamic adaptations achieved through alteration in the patterns of muscle firing1,23,34 during a particular activity provides a possible explanation for the differences in outcome of patients after ACL injury.
JOINT KINETICS DURING GAIT AND THE ACL-DEFICIENT KNEE
An analysis of the kinetics (forces and moments) that act at the knee during walking provides useful insight into the functional changes associated with the ACL-deficient knee. In particular, the moments that act at the knee suggest the cause and potential effect of gait changes after ACL injury. For example, a reduction in the intersegmental moment tending to flex the knee (balanced by net quadriceps contraction) during walking was among the first changes in walking mechanics reported in the ACL-deficient knee.10 The reduction of the net internal quadriceps moment is consistent with quadriceps muscle atrophy, which is frequently reported after ACL injury20 and helps to explain why it is difficult to restore quadriceps strength in these knees. Thus, it is useful to examine the physical meaning and relevance of the intersegmental moment at the knee during walking. This section provides a summary of the methods used to determine the joint moments, an example of how to interpret the magnitude and pattern of the flexion-extension moment at the knee in context of the function of the knee flexors and extensors during ambulation, and an example of how an analysis of the flexion-extension moment during walking can provide insight into the functional role of the ACL.
Critical Points JOINT KINETICS DURING GAIT AND THE ACL-DEFICIENT KNEE
Definition of Intersegmental Moment
A moment is a vector quantity that can be considered a rotational force (lever arm x force) in the sense that it tends to produce a rotation about a specific point. Whereas moments can be calculated at any point, it is useful to use the joints between adjacent limb segments to define the moments that act on the body during walking. For example, the moment acting at the knee would be the intersegmental moment between the thigh and the shank. The external moment tending to flex or extend the joint is illustrated in Figure 6-1. The intersegmental moments are typically calculated from measurement of the foot-ground reaction forces (using a force platform) and the motion of markers placed on the limbs using an optoelectronic system for motion capture. The weight and inertial forces are often approximated by modeling the leg as a collection of rigid segments representing the thigh, shank, and foot. The reader should be aware of the assumptions used in performing these calculations.5 Finally, the units of a moment are force and length. Therefore, it is useful when comparing different-sized subjects to express the intersegmental moments in nondimensional units by dividing the moment by the subject’s height (ht) and body weight (bw). Thus, moments measured during gait are often expressed in units of percentage of the product of the body weight and height (% bw x ht), so that moments can be compared among subjects of different heights and weights.
Interpretation of Intersegmental Moment
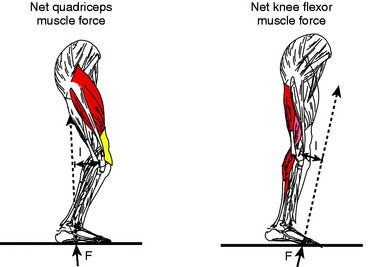
The moment can be visualized in the context of the direction of the ground reaction vector relative to the position of the knee joint center (see Fig. 6-1). If the vector passes anterior to the knee, the moment will tend to extend the knee, whereas if the vector passes posterior to the knee, the moment will tend to flex the knee. As noted previously, the direction of the moment can be used to infer the net muscular moment. Thus, an external moment tending to flex the knee will be balanced by a net quadriceps moment. Previous studies have demonstrated that the external moments measured can be interpreted in terms of the loads on muscles, passive soft tissue, and joint surfaces.32 In addition, the joint moments have been shown to be sensitive indicators of differences between normal and abnormal function.3,10,31
It is useful to examine the assumptions used as the basis for the interpretation of the joint moments during function. Mechanical equilibrium dictates that external forces and moments must be balanced by internal forces and moments. Internal forces generated by muscle, passive soft tissue, and joint contact force create these internal moments. If muscles act only synergistically when balancing the external moments, one could directly infer the internal muscle force in synergistic muscle groups. For example, the total force in the quadriceps needed to balance an external moment tending to flex the knee joint could be determined.32 However, if antagonistic muscle activity is present, the external moment reflects the net balance between agonist and antagonist muscles. The force in the synergistic muscle group would be greater under these conditions. The external moment can, however, be used to obtain a conservative estimate or lower bound on the synergist muscle force. Throughout this chapter, external moments are described from the measurements taken in the laboratory and inferences are made in terms of the net muscular moment (see Fig. 6-1).
The Flexion-Extension Moment and the ACL-Deficient Knees
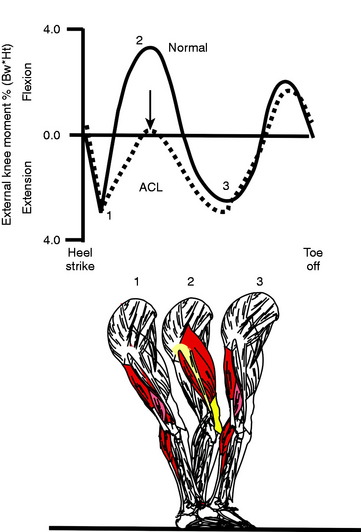
The normal temporal pattern of the flexion-extension moment during stance phase of walking can be interpreted in terms of the net quadriceps moment or net knee flexor muscle moment (hamstrings and/or gastrocnemius) during stance phase (Fig. 6-2). Typically, at heel strike, there is an external moment that tends to extend the knee joint, demanding a net knee flexor force. As the knee moves into midstance, the external moment reverses its direction, demanding a net quadriceps force. As the knee passes midstance, the moment again reverses its direction, demanding net flexor muscle force. Finally, in the pre-swing phase, the moment tends to flex the knee, demanding a net quadriceps muscle force. As previously noted, a reduction of the net quadriceps moment relative to normal is frequently seen in ACL-deficient subjects during level walking (see Fig. 6-2). Specifically, ACL-deficient subjects walk in a manner that has been interpreted as a tendency to avoid or reduce the demand on the quadriceps muscle.10 Whereas the reduction in net quadriceps moment can be interpreted as either a reduction in the quadriceps or an increase in the knee flexor muscle moment, the fact that quadriceps atrophy is a common finding after ACL injury20 supports the conclusion of a reduction in quadriceps contraction during walking.
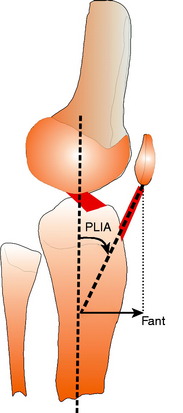
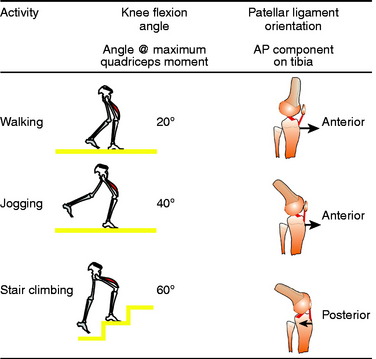
The mechanics of the knee extensor mechanism suggests a possible cause for the inhibition of quadriceps contraction during walking. As illustrated in Figure 6-3, the anterior angulation of the patellar ligament insertion angle (PLIA) causes an anterior force to be applied to the tibia when the quadriceps contracts. In the absence of the ACL, the tibia moves forward when the quadriceps contracts until the force is balanced by other secondary restraints to anterior tibial displacement, such as the medial collateral ligament, meniscus, or a hamstrings contraction. Thus, more anterior tibial translation could occur in ACL-deficient knees than in uninjured knees when the quadriceps contracts. The amount of anterior force is greatest at full extension because the PLIA has the largest anterior angle at full extension and this angle reduces as the knee flexes.17,25 Thus, walking would produce a substantial component of anterior force owing to quadriceps contraction because the knee remains near full extension throughout stance phase, with maximum flexion angles less than 30°. A reduction in quadriceps contraction could eliminate large anterior tibial translations near full extension and prevent sensations of joint instability by the patient.
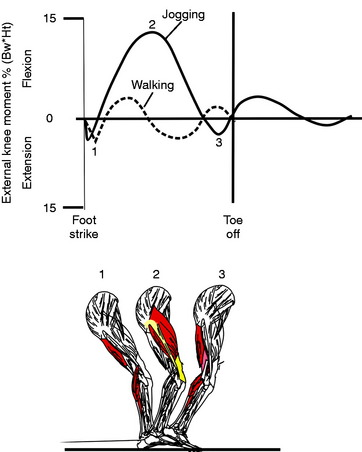
Interestingly, the magnitude of the net quadriceps moment can increase by more than a factor of 5 during jogging as compared with level walking (Fig. 6-4), yet the percentage change in the net quadriceps moment between ACL-deficient and normal subjects is substantially less during jogging than during walking.10 The fact that the maximum net quadriceps moment during jogging occurs when the knee is at approximately 40° of flexion, as compared with 20° during level walking, might provide an explanation for the fact that patients with an ACL-deficient knee do not show a similar reduction in the net quadriceps moment during jogging compared with walking. Similarly, while ascending stairs, the maximum net quadriceps moment occurs at approximately 60° of flexion and thus the amount of reduction in the net quadriceps moment is small compared with that during level walking. The adaptations during activities of daily living appear to be dependent upon the angle of knee flexion when the greatest net quadriceps moment occurs. These observations suggest an interaction between the direction of pull of the patella ligament and the functional role of the ACL (Fig. 6-5). When the knee is near full extension, the patellar ligament places an anterior pull on the tibia. As the knee flexes beyond approximately 45°, the orientation of the patellar ligament reverses direction during the quadriceps contraction and places a posterior pull on the tibia. At deeper flexion angles, the contraction of the quadriceps acts to compensate for an absent ACL.
Thus, during level walking when the maximum net quadriceps moment occurs between 0° and approximately 20°, there is a greater tendency for the quadriceps contraction to produce an anterior pull on the tibia. The adaptation to avoid quadriceps contraction eliminates this anterior force component when the knee is near full extension (see Fig. 6-3).
The Anatomy of the Extensor Mechanism and Quadriceps Inhibition
The variation in the amount of reduction in the net quadriceps moment during walking can be explained by anatomic differences in the anatomy of the extensor mechanism as defined by the PLIA (see Fig. 6-3). As noted previously, the PLIA is of particular importance to the knee extensor mechanism because it determines the decomposition of quadriceps force into anterior and superior directions (see Fig. 6-3) while transferring the quadriceps contraction to the tibia. Previous studies confirmed this relationship by showing that the patellar ligament pulls the tibia anteriorly when the knee is near full extension and also that anatomic variations exist between individuals in both PLIA and the moment arm of the patellar ligament.17 Thus, knees with larger PLIAs generate larger anterior forces on the tibia with the same level of quadriceps contraction.
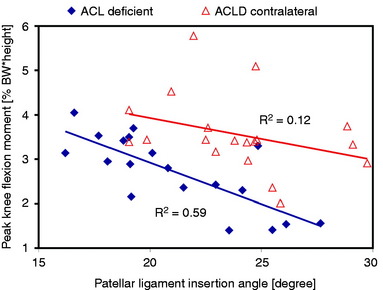
More importantly, it has been shown that the PLIA negatively correlates to the peak knee flexion moment (balanced by net quadriceps moment) during walking in ACL-deficient knees,35 whereas no correlation exists in uninjured contralateral knees of ACL-deficient patients (Fig. 6-6). The negative correlation between PLIA and the peak external knee flexion moment indicates that ACL-deficient knees with higher PLIAs significantly reduce usage of the quadriceps during walking. These results suggest that the subject-specific anatomy of the knee extensor mechanism provides a possible explanation for the variability15 previously observed in adaptation of a quadriceps reduction strategy after ACL injury. This mechanism may explain the reduction in the external knee flexion moment, which is balanced by net quadriceps force, among ACL-deficient knees. This mechanism is further supported by the clinical observation of quadriceps atrophy in ACL-deficient subjects,20 because reduced use of the quadriceps during walking should lead to muscle atrophy. However, the variability between individuals’ adaptations to ACL injury suggests that other factors, such as PLIA, may influence which subjects adopt a strategy of quadriceps reduction.13,28
KNEE KINEMATICS DURING WALKING AND ACL INJURY
The anatomy of the ACL suggests its potential role in determining the motion (kinematics) of the knee during ambulation. Clearly, passive function of the ACL for guiding motion and stabilizing the knee has been well documented. However, the analysis of the functional role of the ACL during dynamic in vivo ambulatory activities is more complex than for passive movements. The force generated by the ACL during passive stretch is relatively small compared with the magnitude of the muscle forces and extrinsic forces (load bearing) that occur during ambulation. Further, the ability to capture the movement of the knee under conditions that reflect natural movement remains a challenge. The kinematic role of the ACL during functional activities has been described for several weight-bearing activities.4,16,22,37 The knee kinematics presented in this chapter focus primarily on walking. The mechanics of walking can provide valuable insights into the functional role of the ACL during locomotion.6 Functional adaptation to the loss of the ACL can be detected during walking, because it has been suggested that patients can adapt patterns of locomotion that compensate for the loss of the ACL. In addition, walking is the most frequent ambulatory activity of daily living, and specific characteristics of this activity have been associated with cartilage thinning.7,26 ACL rupture has been identified as a significant risk factor for premature knee OA. This chapter focuses on the internal-external rotation (IE) and anteroposterior (AP) translation that occur at the knee during walking. These secondary movements (IE, AP) of the knee are directly related to the function of the ACL and have been shown to change in patients with ACL-deficient knees during walking for the reasons described previously.
Critical Points KNEE KINEMATICS DURING WALKING AND ACL INJURY
Methods for Defining and Measuring Knee Kinematics during Walking
The kinematics of human movement during walking is normally described in terms of relative motion between adjacent limb segments (Fig. 6-7). In practice, human gait is most often described in terms of the sagittal plane motion (flexion-extension). This practice has come as a consequence of the much larger motions in this plane, making these motions relatively easy to measure and perhaps most relevant to function. However, the motion at the knee is more complex than other major joints of the lower extremity, involving all six degrees of freedom (three rotations and three translations). The complexity of the kinematic analysis substantially increases when going from a sagittal plane analysis to a complete three-dimensional analysis. The appropriate interpretation of in vivo kinematic measurements requires a precise and physically meaningful definition of anatomic references. For the kinematics described in this chapter, the anatomic femoral coordinate system was located at the midpoint of the transepicondylar line of the distal femur, and the anatomic tibial coordinate system was set at the midpoint of a line connecting the medial and the lateral points of the tibial plateau. The AP translation was determined by calculating the displacement between the origins of the tibial coordinate system relative to a femoral coordinate system projected onto the AP axis of the tibia (see Fig. 6-7). IE rotations were measured by projecting the mediolateral femoral axis onto a plane created by the AP and mediolateral axes fixed in the tibia. Additional details of defining the system used in this chapter can be found in Andriacchi and Dyrby,4 Andriacchi and coworkers,5 and Dyrby and Andriacchi.14
AP Translation and IE Rotation of the Knee during Normal Walking
The flexion-extension motion of the knee is the primary motion of the joint because this movement is required for most ambulatory activities. However, AP translation and IE rotation are important secondary movements of the knee because these movements can influence the moment-generating capacity of the muscles2 as well as the movement of the position of the tibial-femoral contact, all important for normal function. The AP translation and IE rotation of knee have been described for normal walking based on the coordinate system described previously.4,14
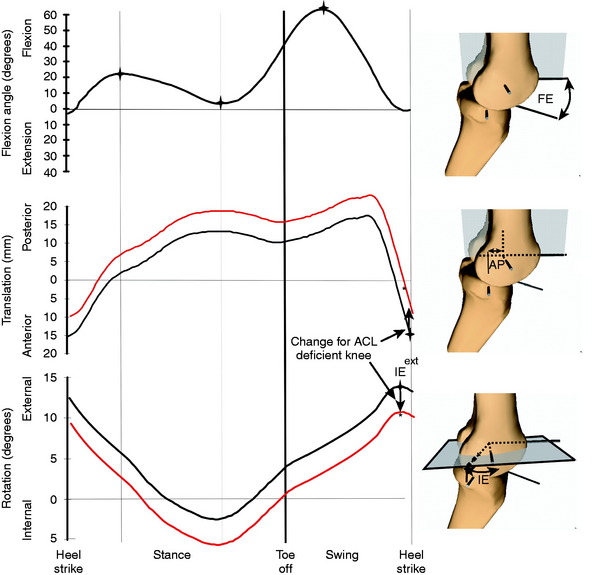
The characteristics of AP translation and IE rotation (see Fig. 6-7) provide a useful basis for understanding the pathomechanics of kinematic changes associated with the loss of the ACL. During normal walking, the tibia is in an anterior position at heel strike that is the result of anterior tibial translation during the terminal portion of swing phase (see Fig. 6-7). During the major portion of stance phase, the tibia translates to a posterior direction. Finally, during the later portion of swing phase, the tibia moves in an anterior direction relative to the femur, reaching a maximum anterior position at or just before heel strike. In addition, at heel strike, the tibia is externally rotated and internally rotates through the major portion of stance phase. The tibia begins to externally rotate during swing phase as the knee extends prior to heel strike and reaches a maximum external rotation at or just before heel strike. The motion of the tibia during the terminal portion of swing phase reflects the natural screw-home motion18 of the knee in which the tibia externally rotates as the knee extends. This natural screw-home movement occurs during the non–weight-bearing portion of the gait cycle in which the passive structure and joint surface drive the movement of the knee. As previously noted, during the weight-bearing stance phase of the walking cycle, the kinematics are driven by the extrinsic forces that act at the knee rather than the internal passive structures such as the ligaments. Thus, the swing phase of repetitive activities such as walking can provide useful insight into the functional role of the ACL because the passive force capacity can have a substantial influence on the knee motion during non–weight-bearing activities.
Kinematic Changes after ACL Injury
Kinematic changes at the knee during ambulation have been reported for patients with ACL-deficient knees.4,16 In particular, the normal external rotation and anterior translation of the tibia that occur as the knee extends during terminal swing are reduced in the absence of the ACL. The tibia maintains this offset relative to normal throughout the stance phase of the walking cycle. These observations indicate that the ACL plays a critical role in the positioning of the knee at the end of swing phase4 in preparation for heel strike during walking (see Fig. 6-7), suggesting a loss of the normal screw-home movement.18 The loss of the screw-home movement at the end of swing phase produces an offset toward internal rotation in the average position of the tibia relative to the healthy knee that is maintained through stance phase. The reduced anterior displacement of the ACL-deficient knee at heel strike also appears to be related to modified kinematics during terminal swing phase. Thus, the transition between swing phase and stance is an important consideration in evaluating the ACL-deficient knee.11,24
ACL injury is associated with premature OA of the knee.19–21,27 The kinematic changes at the knee after ACL injury have been implicated as a factor in the cause of premature OA in this population.7 A shift in the rotational alignment near heel strike can shift the load-bearing contact to regions in the cartilage that have not adapted to the high loads occurring at heel strike. Typically, the thickest regions of the femoral and tibial load-bearing articular cartilage are aligned when the knee is at full extension.
The change in the rotational characteristics at the knee could cause specific regions of the cartilage to be loaded that were not loaded prior to the ACL injury. It has been suggested that the altered contact mechanics in the newly loaded regions could produce local degenerative changes to the articular cartilage.12,40 As previously reported, cartilage in highly loaded areas is mechanically adapted relative to underused areas where signs of fibrillation can be observed in healthy knees in relatively young subjects.12,38 Thus, a spatial shift in the contact region could place loads on a region of cartilage that may not adapt to the rapidly increased load initiating degenerative changes.39
THE ADDUCTION MOMENT AT THE KNEE AND ACL INJURY
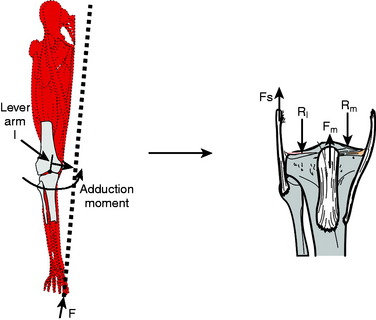
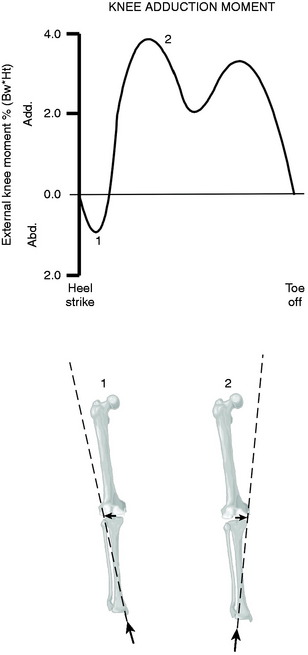
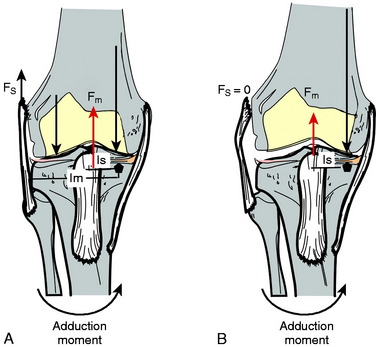
The external adduction moment during walking is a result of the line of action of the ground reaction force passing medial to the center of the knee (Fig. 6-8). The offset or lever arm of this force causes a moment that tends to adduct the knee during walking (Fig. 6-9). The adduction moment will influence the relative distribution of load (see Fig. 6-8) between the medial and the lateral compartments of the knee,32 causing a higher force on the medial compartment relative to the lateral compartment. The adduction moment has become an ambulatory biomechanical marker for risk of progression of medial compartment OA at the knee.7,26 In general, patients with a higher adduction moment have worse treatment outcome after high tibial osteotomy,31 more severe disease,33 and a higher rate of progression of OA.26
The Adduction Moment and OA at the Knee
The adduction moment during walking can be an important consideration in patients with ACL-deficient knees because OA in this group occurs most frequently in the medial compartment. It has been shown that patients with a varus angulation at the knee and ACL injury introduce additional problems that should be considered when making treatment decisions.30 Varus angulation in conjunction with clinical indication of medial compartment OA, cartilage damage, or loss of medial meniscus function is a potential indication for high tibial osteotomy. Gait analysis can provide useful insight into those patients who are at greater risk for medial compartment OA.
Critical Points THE ADDUCTION MOMENT AT THE KNEE AND ACL INJURY
The adduction moment during walking makes the knee vulnerable to lateral joint opening in the absence of stabilizing muscle forces. As illustrated in Figure 6-10, muscle contraction can dynamically stabilize the knee to resist a varus thrust and can compensate for lateral joint laxity. Thus, there is a potential interaction between the reduced quadriceps contraction, a high adduction moment, and lateral laxity30 because a high adduction moment can produce a tendency to open the joint laterally in the absence of the stabilizing forces of muscle contraction (see Fig. 6-9). Based on the mechanics of walking, lateral laxity presents an additional risk in the presence of a varus malaligned knee, a high adduction moment, and reduced quadriceps activity because this combination of conditions can cause the entire force across the knee to be transmitted to the medial compartment. This combination of conditions places the medial compartment of the joint at greater risk for breakdown and should be considered in the overall clinical evaluation of patients with ACL injury.
SUMMARY
1 Andriacchi T.P. Dynamics of pathological motion: applied to the anterior cruciate–deficient knee. J Biomech. 1990;23:99-105.
2 Andriacchi T.P. Functional analysis of pre and post-knee surgery. Total knee arthoplasty and ACL reconstruction. J Biomech Eng. 1993;115:575-581.
3 Andriacchi T.P., Birac D. Functional testing in the anterior cruciate ligament–deficient knee. Clin Orthop Relat Res. 1993;288:40-47.
4 Andriacchi T.P., Dyrby C.O. Interactions between kinematics and loading during walking for the normal and ACL-deficient knee. J Biomech. 2005;38:293-298.
5 Andriacchi T.P., Johnson T.S., Hurwitz D.E., Natarajan R.N. Musculoskeletal dynamics, locomotion, and clinical applications. In: Mow V.C., Huiskes R., editors. Basic Orthopaedic Biomechanics and Mechano-Biology. Philadelphia: Lippincott Williams & Wilkins; 2004:91-122.
6 Andriacchi T., Muendermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr Opin Rheumatol. 2006;18:514-518.
7 Andriacchi T.P., Mundermann A., Smith R.L., et al. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32:447-457.
8 Barber S.D., Noyes F.R., Mangine R.E., et al. Quantitative assessment of functional limitations in normal and anterior cruciate ligament–deficient knees. Clin Orthop Relat Res. 1990;255:204-214.
9 Barrett G.R., Treacy S.H. The effect of intraoperative sometric measurement on the outcome of anterior cruciate ligament reconstruction. Arthroscopy. 1996;12:645-651.
10 Berchuck M., Andriacchi T.P., Bach B.R., Reider B.R. Gait adaptations by patients who have a deficient ACL. J Bone Joint Surg Am. 1990;72:871-877.
11 Beynnon B.D., Fleming B.C., Labovitch R., Parsons B. Chronic anterior cruciate ligament deficiency is associated with increased anterior translation of the tibia during the transition from non-weightbearing to weightbearing. J Orthop Res. 2002;20:332-337.
12 Bullough P.G. The pathology of osteoarthritis. In: Moskowitz R., Howell D., Goldberg V., editors. Osteoarthritis Diagnosis and Medical/Surgical Management. Philadelphia: W. B. Saunders; 1992:36-69.
13 Chmielewski T.L., Rudolph K.S., Fitzegeral G.K., et al. Biomechanical evidence supporting a differential response to acute ACL injury. Clin Biomech. 2001;16:586-591.
14 Dyrby C.O., Andriacchi T.P. Secondary motions of the knee during weight bearing and non–weight bearing activities. J Orthop Res. 2004;22:794-800.
15 Ferber R., Osternig L.R., Woollacott M.H., et al. Gait mechanics in chronic ACL deficiency and subsequent repair. Clin Biomech. 2002;17:274-285.
16 Georgoulis A.D., Papadonikolakis A., Papageorgiou C.D., et al. Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament–deficient and reconstructed knee during walking. Am J Sports Med. 2003;31:75-79.
17 Gross M.T., Tyson A.D., Burns C.B. Effect of knee angle and ligament insufficiency on anterior tibial translation during quadriceps muscle contraction: a preliminary report. J Orthop Sports Phys Ther. 1993;17:133-143.
18 Hallen L.G., Lindahl O. The “screw-home” movement in the knee-joint. Acta Orthop Scand. 1966;37:97-106.
19 Jacobsen K. Osteoarthrosis following insufficiency of the cruciate ligaments in man. A clinical study. Acta Orthop Scand. 1977;48:520-526.
20 Kannus P. Ratio of hamstring to quadriceps femoris muscles’ strength in the anterior cruciate ligament insufficient knee. Relationship to long-term recovery. Phys Ther. 1988;68:961-965.
21 Kannus P., Jarvinen M. Posttraumatic anterior cruciate ligament insufficiency as a cause of osteoarthritis in a knee joint. Clin Rheumatol. 1989;8:251-260.
22 Li G., Defrate L.E., Rubash H.E., Gill T.J. In vivo kinematics of the ACL during weight-bearing knee flexion. J Orthop Res. 2005;23:340-344.
23 Limbird T.J., Shiavi R., Frazer M., Borra H. EMG profiles of knee-joint musculature during walking: changes induced by anterior cruciate ligament deficiency. J Orthop Res. 1988;6:630-638.
24 Ma C.B., Janaushek M.A., Vogrin T.M., et al. Significance of changes in the reference position for measurements of tibial translation and diagnosis of cruciate ligament deficiency. J Orthop Res. 2000;18:176-182.
25 Matthews L.S., Sonstegard D.A., Henke J.A. Load bearing characteristics of the patello-femoral joint. Acta Orthop Scand. 1977;48:511-516.
26 Miyazaki T., Wada M., Kawahara H., et al. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617-622.
27 Nebelung W., Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament–deficient knees in high-level athletes. Arthroscopy. 2005;21:696-702.
28 Noyes F.R., Matthews D.S., Mooar P.A., Grood E.J. The symptomatic anterior cruciate–deficient knee. Part II: the results of rehabilitation, activity modification, and counseling on functional disability. J Bone Joint Surg Am. 1983;65:163-174.
29 Noyes F.R., Mooar P.A., Matthews D.S., Butler D.L. The symptomatic anterior cruciate–deficient knee. Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg Am. 1983;65:154-162.
30 Noyes F.R., Schipplein O.D., Andriacchi T.P., et al. The anterior cruciate ligament–deficient knee with varus alignment. An analysis of gait adaptations and dynamic joint loadings. Am J Sports Med. 1992;20:707-716.
31 Prodromos C.C., Andriacchi T.P., Galante J.O. A relationship between gait and clinical changes following high tibial osteotomy. J Bone Joint Surg Am. 1985;67:1188-1194.
32 Schipplein O.D., Andriacchi T.P. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9:113-119.
33 Sharma L., Hurwitz D.E., Thonar E.J., et al. Knee adduction moment, serum hyaluronic acid level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum. 1998;41:1233-1240.
34 Shiavi R., Zhang L.Q., Limbird T., Edmondstone M.A. Pattern analysis of electromyographic linear envelopes exhibited by subjects with uninjured and injured knees during free and fast speed walking. J Orthop Res. 1992;10:226-236.
35 Shin C.S., Chaudhari A.M., Dyrby C.O., et al. The patella ligament insertion angle influences quadriceps usage during walking of anterior cruciate ligament deficient patients. J Orthop Res. 2007;25:1643-1650.
36 Snyder-Mackler L., Fitzgerald G.K., Bartolozzi A.R.3rd, Ciccotti M.G. The relationship between passive joint laxity and functional outcome after anterior cruciate ligament injury. Am J Sports Med. 1997;25:191-195.
37 Tashman S., Kolowich P., Collon D., et al. Dynamic function of the ACL-reconstructed knee during running. Clin Orthop Relat Res. 2007;454:66-73.
38 Wong M.M., Siegrist M., Cao X. Cyclic compression of articular cartilage explants is associated with progressive consolidation and altered expression pattern of extracellular matrix proteins. Matrix Biol. 1999;18:391-399.
39 Wu J.Z., Herzog W., Epstein M. Joint contact mechanics in early stages of osteoarthritis. Med Eng Phys. 2000;22:1-12.
40 Yao J.O., Seedhom B.B. Mechanical conditioning of articular cartilage to prevalent stresses. Br J Rheumatol. 1993;32:956-965.