Human Age and Microorganisms
After reading this chapter, the student will be able to:
• Identify the different effects microorganisms have on the different age groups
• Explain the different immune reactions that occur in the different age groups
• Describe the infections that typically can occur in pregnant women and ultimately can have an effect on fetal development
• Name and describe congenital infections, including causative agent, transmission, symptoms, and treatments
• Discuss the common microbial infections that affect infants and children
• Describe the microbial infections that commonly occur in young adults
• Illustrate the environmental exposures to microbes that are typical for young adults
• Describe the common microbial infections in the elderly and compare these with the other age groups
• Explain the immune system of the elderly and contrast it to the other age groups
• Portray factors that can influence the susceptibility to microbial infections and disease among the elderly
Perinatal
Introduction
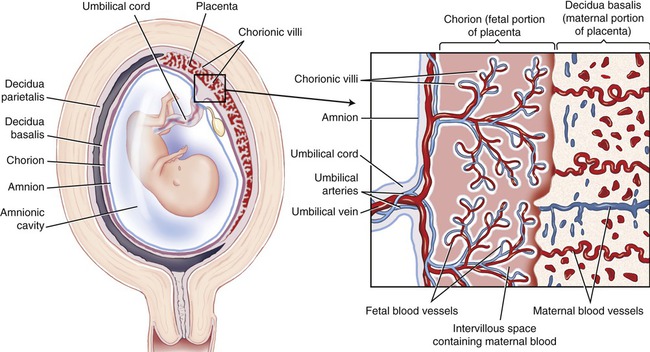
The placenta is a highly specialized (Figure 23.1) structure that generally is an effective barrier, protecting the fetus from microorganisms that may be present in the mother’s circulation or in the urogenital tract. Placental tissue normally separates maternal and fetal blood supplies so that no intermixing occurs. Unfortunately, some infectious organisms may penetrate this barrier and injure the developing embryo or fetus.
Infections During Pregnancy
The length of pregnancy in humans is approximately 39 weeks and is called the gestation period, divided into three phases referred to as trimesters. The embryonic phase of development extends from fertilization to the end of the eighth week, and the developing individual is referred to as an embryo. From the eighth week until birth the developing infant is called a fetus. Neither an embryo nor a fetus has a developed immune system (see Chapter 20, The Immune System). IgM and IgA synthesis is limited until the second half of the pregnancy, IgG antibody synthesis is absent, and cell-mediated immune responses are absent or poorly developed. In other words, the embryo/fetus is completely dependent on its mother’s immune system. Immunosuppression in the mother will result in a potentially disastrous susceptibility of the unborn to infectious disease. Certain infections can be more common during pregnancy (Table 23.1) and others may recur (Table 23.2), all of which can present a particular risk to the woman and/or her unborn child.
TABLE 23.1
Infections That May Be More Common or Severe During Gestation
| Infection | Covered in Chapter(s): | Comments |
| Urinary tract infections (UTIs) | 15 | Cystitis; pyelonephritis; atony of the urinary bladder, leading to less effective emptying/flushing |
| Malaria | 14 | Probably due to depressed cell-mediated immunity |
| Viral hepatitis | 7 and 12 | Probably due to additional stress on metabolic activities |
| Influenza | 11 | Higher mortality during pandemics; may be prevented by vaccination |
| Poliomyelitis | 7 | Paralysis more common |
| Coccidioidomycosis | 11 | Leading cause of maternal mortality in endemic areas in the southwestern United States and Latin America |
| Candidiasis | 10 | Vulvovaginitis |
| Listeriosis | 12 | Influenza-like disease can cause auto-abortions in pregnant women |
TABLE 23.2
Maternal Infections That May Recur During Pregnancy
| Infection | Covered in Chapter(s): | Comments |
| Cytomegalovirus | 7 | Sheds from cervix, is present in mother’s milk |
| Herpes simplex virus | 10 and 12 | Increased replication in cervical region |
| Epstein-Barr virus | 14 | Virus sheds in oropharynx; antibody titers are increased |
| Polyomavirus | 15 | Virus appears in urine |
Congenital Infections
Congenital Cytomegalovirus Infection
• About 1 in 150 children is born with a congenital CMV infection
• Approximately 1 in 750 children is born with or develops a permanent disability due to a CMV infection
• Roughly 8000 children each year suffer permanent disabilities due to CMV
• More than 90% of infected newborns are asymptomatic at the time of birth
• About 5% to 15% of asymptomatic babies at birth will develop symptoms within the first 2 years of life. These symptoms may include hearing loss, low intelligence, microcephaly, and chorioretinitis.
• Symptomatic newborns show various severities of the illness. Manifestations include hepatosplenomegaly, jaundice, purpura, microcephaly, cerebral calcifications, and chorioretinitis. Central nervous system involvement is the most common demonstration of congenital CMV infections. Ocular and hearing defects are common, and others include microcephaly, periventricular calcification, severe psychomotor retardation, strabismus, seizures, and low birth weight.
Congenital Rubella
• Cloudy corneas and other eye defects
• Skin rash at birth: Thrombocytopenic purpura (blueberry muffin rash)
An infected fetus generally produces its own IgM to the virus, which can be detected in the umbilical cord and in the blood of the infant. Some congenitally infected children will develop insulin-dependent diabetes later in life. The main risk factor for congenital rubella occurs when a pregnant woman who has not been vaccinated comes into contact with a person who has rubella (also called German measles; see Chapter 7, Viruses).
Congenital Toxoplasmosis
Toxoplasmosis is caused by the parasite Toxoplasma gondii. The organism can be found in raw meat, and is commonly found in cat litter and contaminated soil. The life cycle of Toxoplasma gondii is illustrated in Figure 23.2. Although toxoplasmosis is common in men and women, the infection during pregnancy can lead to congenital toxoplasmosis, which can damage the baby’s eyes, nervous system, skin, and ears. Clinical features in the infant include the following:
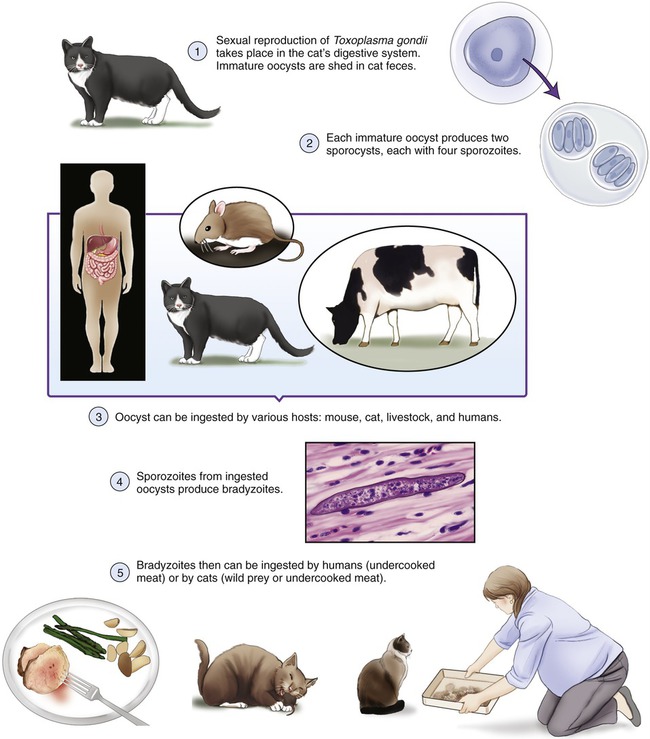
Oftentimes there are no detectable abnormalities at birth, but health problems may become apparent in the second or third decade of life. To prevent toxoplasmosis pregnant women should avoid cleaning litter boxes, other areas that have contact with cat litter, and also should cook meat until it is well done. Cross-contamination should be avoided. Treatment is possible for the pregnant mother, usually with spiramycin, and fetal infections diagnosed during pregnancy can be treated with pyrimethamine and sulfadiazine. CDC recommendations to prevent congenital toxoplasmosis are shown in Box 23.1.
Congenital HIV Infection
Clinical symptoms of congenital HIV infections include poor weight gain, susceptibility to sepsis, developmental delays, lymphocytic pneumonitis, oral thrush, enlarged lymph nodes, hepatosplenomegaly, diarrhea, and pneumonia. Some infants develop AIDS by age 1 year. Most infections occur during late pregnancy or during delivery; transmission rates can be reduced by lowering the HIV load by using antiretroviral drugs during pregnancy. Elective cesarean section and avoiding breastfeeding may also reduce the risk of infection. The medical and supportive services recommended by the U.S. Department of Health and Human Services after a child is born to an HIV-positive mother are listed in Box 23.2. In developing countries, about a quarter of infants born to HIV-positive mothers are infected.
Vaginal Infections
A common vaginal infection known as bacterial vaginosis (BV) is an imbalance of the normal bacterial flora of the vagina (see Chapter 16, Infections of the Reproductive System). With BV, increased numbers of anaerobic organisms are found, including Gardnerella vaginalis, Mycoplasma hominis, and Bacteroides. Although these organisms are part of the normal vaginal flora, they do cause problems when they outnumber the normal Lactobacillus flora. Pregnant women with BV are more likely to give birth to a premature infant with a low birth weight than are women who do not have the vaginal infection.
Infants and Children
Immune System in Infants and Children
The immune system of a newborn is immature and often unable to escalate an effective immune response. At birth and for the next few months the infant is dependent on the passive antibodies received through the placenta before birth, and via colostrum and breastmilk after birth. Antibodies that can cross the placenta are IgGs. In addition to IgGs, colostrum and breastmilk also contain IgAs (see Chapter 20, The Immune System) together with a variety of white blood cells. These passive antibodies are the same as the ones circulating in the mother’s circulatory system, representing the mother’s immunity to her environment. Therefore, infants usually have antibodies against microbes in their own home. However, a mother with a compromised or weak immune system will pass fewer antibodies to her child, who will thus have fewer passive antibodies and thus a weaker immune system.
Although there is some protection for an infant in its mother’s womb, which contains microbes to which she has developed antibodies, the infant will not be immediately protected against new exposures. The greatest danger of infectious diseases to an infant is caused by microbes against which the mother has no antibodies; she cannot therefore pass on passive immunity to her infant. The hospital environment often contains bacteria that have developed resistance against antibiotics (see Healthcare–associated [Nosocomial] Infections in Chapter 9, Infection and Disease), which can cause a tremendous problem if an infant becomes infected.
Common Microbial Infections in Infants and Children
Skin Infections
The skin becomes colonized by normal flora during birth. The normal skin flora of an individual is dependent on age. For example, micrococci are more prominent in infants and children than on the adult skin. Skin infections are common during the neonatal period and in preschool age children exposed to contagious organisms. For more details on infections of the skin refer to Chapter 10 (Infections of the Integumentary System, Soft Tissue, and Muscle).
• Deep folliculitis: This condition may be extensive, involving a wide area, especially the scalp in infants and young children.
• Staphylococcal scalded skin syndrome, caused by group II staphylococci, is more common in infants than in adults.
• Impetigo: Three different forms of impetigo are recognized on the basis of clinical, bacteriological, and histological findings. In infants the most common form is impetigo neonatorum, caused by Staphylococcus aureus. It is a highly contagious disease and a real problem in nurseries. The illness usually occurs between the fourth and tenth day after birth and if not immediately treated can result in an epidemic in nurseries. Impetigo is also common in older children and usually is not serious; however, if attending a child care center the child may receive antibiotic treatment to be able to return to the center, usually 24 hours after the start of antibiotic therapy.
Other Neonatal Infections
• Group B streptococcal disease (GBS): Group B beta-hemolytic streptococci and gram-negative bacilli infection can be acquired by cross-infection in the nursery or transmitted by their mothers during birth. Some of the most common illnesses caused by group B Streptococcus are sepsis, pneumonia, and meningitis (also see Chapter 14, Infections of the Circulatory System).
• Herpes simplex infections may come from cold sores of attending adults.
• Escherichia coli infections are common neonatal infections that can lead to urinary tract infections, sepsis, meningitis, and pneumonia.
• Staphylococcal conjunctivitis (sticky eye) can occur through contamination of the infant with staphylococci from the noses and fingers of adult carriers.
Infections in Children
In their first 10 years of life children are constantly exposed to a variety of microbes, especially in day care centers and elementary school. The following is a limited list of common infections in children; a detailed listing and more information can be found on the CDC website: http://www.cdc.gov/ncidod/diseases/children/diseases.htm
• Sore throat (pharyngitis) caused by Streptococcus pyogenes, which can result in complications (see Streptococcal Infections in Chapter 11, Infections of the Respiratory System).
• Rheumatic fever is a childhood disease that does not stand alone. It is always preceded by another streptococcal infection (see Medical Highlights: Complications of Strep Throat [Rheumatic Fever] in Chapter 11).
• Scarlet fever, once a serious childhood disease, is now treatable (see Scarlet Fever in Chapter 11).
• Otitis media: Ear infections.
• Chickenpox: A disease caused by the varicella-zoster virus, causing an itchy skin rash (see Chapter 7, Viruses). Vaccination is available.
• Rubella: German measles is a viral respiratory infection and it is recommended by the CDC that children should be vaccinated (see Chapter 7).
• Common cold: Caused by human parainfluenza viruses (see Chapter 7).
• Mumps and measles: Both are vaccine-preventable diseases (see Chapter 7).
Young Adults
Immune System in Young Adults
The immune system of young adults is active and generally has defenses against most childhood diseases, various cold viruses, and other microbes that the individual has been exposed to or has been vaccinated against. The metabolism of young adults is generally high; therefore production of new cells, including those of the immune system, flourishes during young adulthood. However, the immune system still faces major challenges because of the changing environments young adults are experiencing. Also, after puberty the thymus gland, the organ responsible for the maturation of T lymphocytes, starts to show some atrophy (see Chapter 20, The Immune System).
Common Microbial Infections in Young Adults
Infectious Mononucleosis
Infectious mononucleosis is caused by the Epstein-Barr virus and often occurs in young adults, especially during the high school years. It is also called the “kissing disease” because it occurs predominantly in high school–aged children. Oftentimes the virus is transmitted by sharing of drinking glasses, bottles, or utensils. For more information refer to Infectious Mononucleosis and Life Application: “Kissing Disease” in Chapter 14, Infections of the Circulatory System.
Sexually Transmitted Infections
Most college students are or have been sexually active, and many have had multiple partners, increasing the risk for STIs. The rates of chlamydia, gonorrhea, and HPV are highest among female adolescents. For information about specific sexually transmitted infections please refer to Chapter 17, Sexually Transmitted Infections/Diseases.
Influenza
Adolescents and college-age students usually are not considered to be at high risk for serious influenza with resulting mortality. However, because of living in close quarters, they can easily spread the infections. In addition, segments of this population, such as those with asthma, HIV, and those who are pregnant, are at high risk for a serious infection. Influenza vaccination is available on many college campuses not only to high-risk individuals but also to those who want to avoid becoming ill with influenza. Vaccination would greatly reduce the spread of the illness and also lessen the number of days during which students miss classes. For more information about influenza refer to Chapter 11, Infections of the Respiratory System.
Meningococcal Disease
Meningococcal disease may be caused by Neisseria meningitidis and can cause both sporadic disease as well as outbreaks. According to the CDC, N. meningitidis has become the leading cause of bacterial meningitis in children and young adults in the United States. For more information refer to Meningococcal Meningitis and also to Life Application: Meningitis: The Dorm Disease? in Chapter 13, Infections of the Nervous System and Senses.
Environmental Exposures Typical for Young Adults
During adolescence many individuals become sexually active, exposing themselves to sexually transmitted microorganisms. Many of these microbes will cause infection and show symptoms, and some of them will be asymptomatic (see Chapter 17, Sexually Transmitted Infections/Diseases).
Many young adults also will attend college or join the military, where they usually are in close quarters, which can be breeding grounds for various microorganisms, some of them potentially pathogenic. After finishing college individuals enter the work force, where they are again exposed to new microbes—the immune system being challenged and actively producing antibodies (see Active Immunity [Humoral] in Chapter 20, The Immune System). Another possible exposure to new microbial environments is encountered during the travel many young adults undertake, including international destinations.
Older Adults
The United States population is rapidly aging, leading to the publication of “The State of Aging and Health in America 2007,” a report released by the CDC and the Merck Company Foundation in March 2007. According to the report, by 2030 the number of Americans age 65 years and over will be more than 71 million, encompassing about 20% of the U.S. population. This will provide a challenge to the healthcare system to preserve the health of this elderly population. Besides other health challenges for an aging body, it is important to understand that microbes will interact differently in the elderly than in a young adult.
Immune System in Older Adults
The aging immune system is also often less able to differentiate between the body’s own cells and foreign substances, and may start attacking some of the body’s own cells. This can result in autoimmune disorders (see Chapter 20, The Immune System), which become more frequent during aging. The immune system is responsible for the destruction of cancer cells, invading microbes, and other foreign substances. The aging immune system is less capable of doing so, which may explain the increased incidence of cancer in the older population. Because of the reduced activity of the immune system, allergic reactions also decline.
Common Microbial Infections in Older Adults
Pneumonia
Although pneumonia (see also Chapter 11, Infections of the Respiratory System) occurs in people of all ages, it occurs more commonly in older people, where it tends to be more serious. Pneumonia is one of the most common and also significant health problems in the elderly, especially those hospitalized or residing in other healthcare facilities. It is often the terminal event after a prolonged serious illness and is the leading infectious cause of death in this age group. The major risk factor for developing pneumonia in this age group is the presence of another serious illness, or it can be a result of a previous illness such as influenza. In 30% to 50% of cases the infectious agent is not identified; the most common identifiable organisms causing the illness are listed as follows:
• Streptococcus pneumoniae causes pneumococcal pneumonia and is the most common bacterial cause of community-acquired pneumonia in the elderly. Individuals 65 years of age and older are three to five times more likely to die of this condition than are younger individuals. Drug-resistant strains cause drug-resistant Streptococcus pneumonia (DRSP) disease, with the elderly being highly susceptible (see Drug-resistant Streptococcus pneumoniae Disease in Chapter 11, Infections of the Respiratory System).
• Haemophilus influenzae account for 8% to 20% of pneumonias in the elderly, most frequently in those with chronic bronchitis.
• Legionella spp.: The susceptibility to these organisms increases with age.
• Gram-negative bacilli are more common in institutional settings and include Klebsiella, Pseudomonas aeruginosa, Enterobacter spp., Proteus spp., Escherichia coli, and others. Gram-negative bacilli often colonize in the pharynx of seriously ill patients and account for approximately 40% to 60% of all culture-diagnosed pneumonias.
• Anaerobic bacteria cause 20% of community-acquired infections and 31% of nosocomial cases of pneumonia in the elderly. These microbes usually cause illness among the elderly on aspiration, especially by those with conditions that cause altered consciousness due to medications and medical conditions. The organisms involved may be Fusobacterium nucleatum, peptostreptococci, peptococci, and Bacteroides fragilis.
• Viral causes of pneumonia include influenza and parainfluenza viruses, respiratory syncytial virus, and occasionally adenoviruses.
Influenza
Influenza is caused by one of the influenza viruses and affects the entire body, but its most evident effect is on the airways (see Chapter 11, Infections of the Respiratory System). Influenza affects persons of all ages but is particularly serious in the elderly. In a typical year the illness leads to more than 20,000 deaths, with older people accounting for more than 80% of these. Influenza vaccination is recommended for all older persons. Pneumonia and severe bronchitis commonly accompany influenza in the older population, and the rate of severity increases with age. Pneumonia may be due to primary influenza, other viral infection (e.g., the common cold), or secondary bacterial infection.
Urinary Tract Infections
Urinary tract infections (UTIs) are a common problem in the elderly. Diagnosis, prevention, and treatment can often be a problem because the clinical symptoms may be atypical. Furthermore, the host defenses decrease with age. Common risk factors for urinary tract infections in the elderly are listed in Box 23.3. For more information about urinary tract infections refer to Chapter 15, Infections of the Urinary System.
Skin Infections
Aging leads to changes in the skin and its appendages. These changes include dryness, atrophy, and decline in cell replacement, barrier function immunologic responsiveness, thermoregulation, and many more. These changes can cause a variety of skin infections including herpesvirus infections (e.g., varicella-zoster virus and herpes simplex virus [HSV]), cellulitis, erysipelas, necrotizing fasciitis, impetigo, folliculitis, furunculosis, candidiasis, and a variety of rashes. For more detailed information about the various skin infections please refer to Chapter 10, Infections of the Integumentary System, Soft Tissue, and Muscle.
HEALTHCARE APPLICATION
Pneumonias in the Elderly*
| Organism | Comments | Treatment |
| Streptococcus pneumoniae | Community-acquired; person-to-person contact or inhalation | Penicillin, first-generation cephalosporin, a macrolide, a fluoroquinolone |
| Haemophilus influenzae | Mostly in patients with chronic bronchitis; transmitted by aerosol | Cefuroxime, third-generation cephalosporins, trimethoprim-sulfamethoxazole, levofloxacin |
| Legionella spp. | Susceptibility increases with age; Legionnaire’s disease | Erythromycin with or without rifampin, newer macrolide, a fluoroquinolone |
| Pseudomonas aeruginosa | Institutional setting; colonizes the posterior pharynx of seriously ill patients | Antipseudomonal penicillin or ceftazidime plus an aminoglycoside |
| Anaerobic bacteria | Community-acquired and nosocomial; usually the result of aspiration | Penicillin or clindamycin |
| Influenza A virus | Influenza—most important cause of pneumonia in the elderly | Amantadine or rimantadine and an antibiotic |
*Also see Healthcare Application: Pneumonias in Chapter 11, Infections of the Respiratory System.
Summary
• Microorganisms affect the various human age groups in different manners because of a variety of factors, one of the most important ones being the functional capacity of the immune system.
• Microbial infections that can be passed on from a mother to a child either during pregnancy or during birth are referred to as perinatal infections. Many of them will become evident after birth.
• A congenital disorder is any medical condition that is present at birth, regardless of the origin. Congenital infections, on the other hand, are intrauterine infections that occur during pregnancy when microorganisms enter the blood, infect the placenta, and ultimately the fetus.
• Many infections and illnesses in infants are due to perinatal infections, but others may be transmitted to the newborn during the first week or two after birth.
• The immune system of the infant is immature and its defense against microorganisms depends on passive antibodies received from the mother during pregnancy and lactation.
• Young children during their day care, preschool, and elementary school years are exposed to a multitude of microbes, infections, and diseases, all of which stimulate the maturation of the immune system. Vaccination also plays an important role in this process.
• Although most infections that occur in young adults can also occur in middle-aged and older adults, certain infections such as mononucleosis and sexually transmitted infections occur more commonly in adolescents and college-aged individuals.
• In general, the immune system of young adults can respond to all the microbes it has previously been exposed to. However, once entering college, the military, or the work environment new microbial environments will challenge the immune systems of young adults to make more antibodies.
• The population aged 65 years and over is constantly increasing in the United States as well as in the rest of the world. Various infectious diseases are of great concern in this population.
• A progressive decline or dysfunction in the aging immune system is referred to as immune senescence, and is responsible for the increased incidence of severe infectious disease in the elderly. The severity of infections often increases with increasing age.
Review Questions
1. The highly specialized structure that protects the fetus from microorganisms is the:
2. Congenital CMV infections are caused by:
3. The most common virus transmitted during pregnancy is:
4. A fetus infected with rubella virus produces which of the following antibodies that can then be detected in the umbilical cord?
5. The type of antibody that can cross the placenta is:
6. Staphylococcal scalded skin syndrome is most common in:
7. Infectious mononucleosis most often occurs in:
8. Almost half of all the STIs diagnosed in the United States are among:
9. Infectious diseases in the adult population are responsible for about one third of all deaths in individuals over the age of:
10. All the following infections may recur during pregnancy except:
11. A bacterial or viral infection that can be passed from a mother to her child before or during birth is called a(n) __________ infection.
12. Impetigo neonatorum is caused by __________.
13. Infectious mononucleosis is caused by __________.
14. Chlamydia commonly occurring in young adults is a(n) __________ disease.
15. The decline in the functioning of the immune system during aging is referred to as __________.
16. Discuss congenital CMV infections and give three statistics about the infection in the United States.
17. Describe the measures the CDC has recommended to avoid congenital toxoplasmosis.
18. Name the most commonly occurring sexually transmitted infections on U.S. college campuses.
19. Name and discuss the most common microbial infections that occur in the elderly population.
20. Differentiate between the immune systems of the infant, young adult, and older individual.