How to choose the most appropriate ultrasound-guided approach for central line insertion: Introducing the rapid central venous assessment protocol
Overview
Standard central venous access performed with the “blind” technique was historically based on the puncture of two central veins (the subclavian vein and the internal jugular vein),1 but ultrasound (US) guidance has expanded the spectrum to at least four sites: the internal jugular vein, the brachiocephalic (or “innominate”) vein, the subclavian vein, and the axillary vein. In many patients, two additional, centrally located venous segments can be cannulated: the external jugular vein (in its final tract close to the junction of the subclavian vein) and the cephalic vein (in its final, infraclavicular tract close to the junction of the axillary vein).
The shift from a “heads-or-tails” choice (subclavian vs. jugular) to a wide spectrum of choices (internal jugular, brachiocephalic, subclavian, axillary, etc.) is the real “Copernican” revolution of the US era. Whereas in the last century the physician was bound to choose between the subclavian and jugular sites on the basis of personal preference, instinct, or experience, selection of the most appropriate vein to cannulate can be determined today on a rational basis by means of US technology.2
The rapid central vein assessment
US guidance is an evidence-based methodology that significantly reduces the complications related to insertion of CVCs.3–5 However, the benefit of using US is not limited to real-time US-guided venipuncture. The GAVeCeLT (Italian Group for Venous Access Devices) recommended the use of US during CVC insertion for six different purposes: (1) US evaluation of all veins available, (2) choice of the vein on the basis of rational US-based criteria, (3) real-time US-guided venipuncture, (4) US-based control of guidewire/catheter orientation during the procedure, (5) US-based control of pleura-pulmonary integrity after axillary or subclavian vein puncture, and (6) transthoracic echocardiography for verification of the position of the tip of the catheter at the end of the procedure.
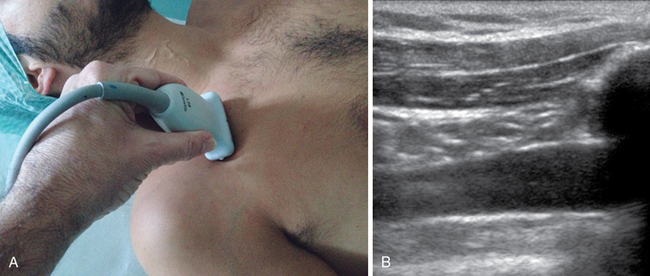
• The transducer is positioned in a transverse plane at the midneck region (Figure 12-1A). This allows evaluation of the internal jugular vein and carotid artery (short axis; Figure 12-1B). This is an ideal position for an internal jugular vein, US-guided approach using either an “in-plane” or an “out-of-plane” technique.
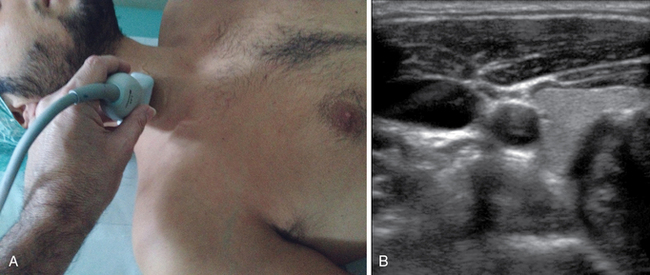
Figure 12-1 First step in the rapid central vein vascular assessment protocol. A, Probe positioned at the midneck. B, Visualization of the internal jugular vein and carotid artery.
• By sliding the transducer down the neck toward the sternum (Figure 12-2A), it is possible to evaluate the internal jugular vein in its lower tract (in the short axis) and visualize the subclavian artery (long axis; Figure 12-2B).
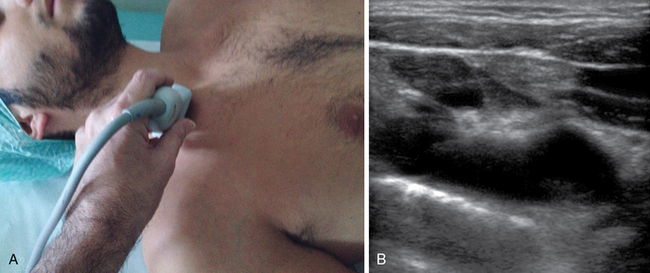
Figure 12-2 Second step. A, Probe sliding down to the sternum. B, Visualization of the lower tract of the internal jugular vein and the subclavian artery.
• By tilting the transducer to achieve an almost frontal plane (Figure 12-3A), the brachiocephalic vein can be visualized (long axis; Figure 12-3B). This is an ideal position for “in-plane” cannulation of the brachiocephalic vein.
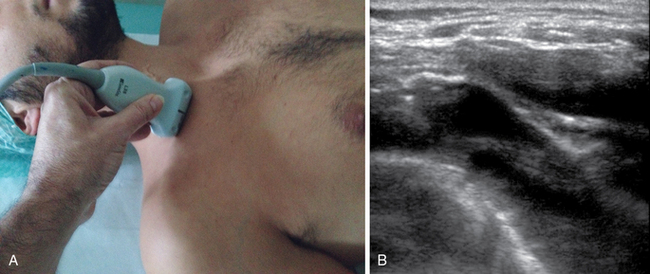
Figure 12-3 Third step. A, Tilting the probe to an almost frontal plane. B, Visualization of the brachiocephalic vein.
• By sliding the transducer laterally, behind the clavicle (Figure 12-4A), the subclavian vein and external jugular vein (long axis; Figure 12-4B) can be visualized, and the subclavian artery can be detected at an even more lateral plane (short axis). In this position the subclavian or the external jugular vein can be cannulated via an “in-plane” approach.
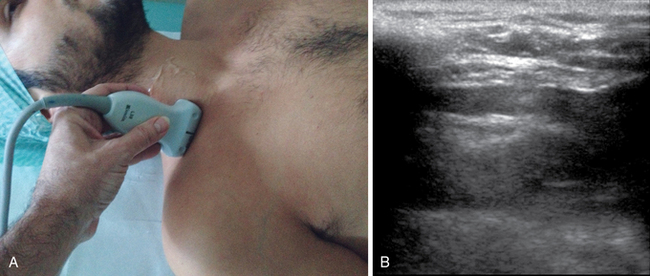
Figure 12-4 Fourth step. A, Sliding the probe laterally above the clavicle. B, Visualization of the subclavian vein and external jugular vein.
• Next, the transducer is positioned below the distal third of the clavicle (Figure 12-5A) for proper visualization of the axillary vein and artery (short axis) and the cephalic vein (long axis; Figure 12-5B). In this position the axillary vein can be cannulated via an “out-of-plane” approach.
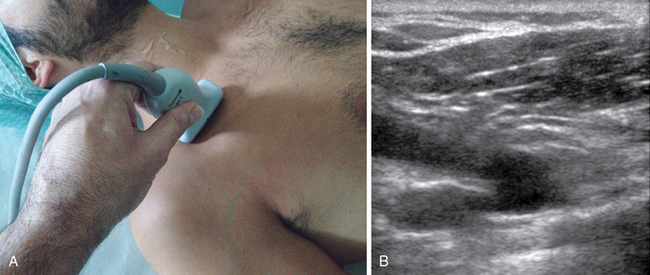
Figure 12-5 Fifth step. A, Probe below the lateral third of the clavicle. B, Visualization of the axillary vein, the axillary artery, and the cephalic vein.
• By rotating the transducer anticlockwise (Figure 12-6A), the axillary vein is visualized (long axis; Figure 12-6B). In this position the vein can be cannulated via an “in-plane” technique.
Criteria for choosing the appropriate vein according to the rapid central vein vascular assessment protocol
• Diameter of the vein. Usually, the largest vein in this area is the brachiocephalic vein. The other three major veins are variable in size. The cephalic vein and the external jugular vein are normally small in adults, although in children and neonates these veins appear to have a relatively larger size than the adjacent venous segments. As a general rule, veins that are too small are difficult to cannulate. When the diameter of the vein is less than three times the caliber of the catheter, the risk for thrombosis might be increased.
• Depth of the vein from the surface of the skin. The axillary vein, for example, may be easy or difficult to cannulate, depending on its depth.
• Possible venous collapse during breathing. This is typically an issue with the internal jugular and axillary veins.
• Compression of the vein by strong arterial pulsation (e.g., compression of the internal jugular vein by the carotid pulse).
• Proximity of the vein to structures that may increase the risk for mechanical complications (e.g., the pleura being constantly “adherent” to the inferior wall of the subclavian vein).
• Easy management of the exit site. For example, when dealing with nontunneled catheters, an exit site in the infraclavicular area is favored over one located in the midneck region because the former is associated with easier nursing care and decreased risk for dislocation and infection.
Pearls and highlights
• The benefit of US is not limited to real-time US-guided venipuncture. US has an even more important role in allowing the operator to choose the safest and easiest approach for central venous access.
• Application of the RaCeVA protocol (which has been introduced by the Italian Group for Venous Access Devices) facilitates systematic scanning of all possible venous targets and enables the operator to make a rational decision about which vein to cannulate by applying specific criteria. Moreover, it is a teaching tool for the different US-guided approaches that may be used to cannulate a central vein.6
• The RaCeVA protocol can be performed rapidly (40 seconds for each side) by expert operators and is easy to teach and learn. It can be used in any patient (adults, children, and neonates) and represents a cost-effective solution that may increase patient safety.7
References
1. Pittiruti, M, Malerba, M, Carriero, C, et al. Which is the easiest and safest technique for central venous access? A retrospective survey of more than 5,400 cases. J Vasc Access. 2000; 1(3):100–107.
2. Lamperti, M, Bodenham, AR, Pittiruti, M, et al. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med. 2012; 38(7):1105–1117.
3. Troianos, CA, Hartman, GS, Glas, KE, et al, Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2011;24(12):1291–1318.
4. American Society of Anesthesiologists Task Force on Central Venous Access, Rupp, SM, Apfelbaum, JL, Blitt, C, et al, Practice guidelines for central venous access: a report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 2012;116(3):539–573.
5. Pittiruti, M, Hamilton, H, Biffi, R, et al. ESPEN guidelines on parenteral nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr. 2009; 28(4):365–377.
6. Davidson, IJ, Yoo, MC, Biasucci, DG, et al. Simulation training for vascular access interventions. J Vasc Access. 2010; 11(3):181–190.
7. Pittiruti, M. Ultrasound guided central vascular access in neonates, infants and children. Curr Drug Targets. 2012; 13(7):961–969.