17 Home Care and Pulmonary Rehabilitation
Note 1: This book is written to cover every item listed as testable on the Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE).
The listed code for each item is taken from the National Board for Respiratory Care’s (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and the WRE, it will simply be shown as: (Code: …). If an item is only testable on the ELE, it will be shown as: (ELE code: …). If an item is only testable on the WRE, it will be shown as: (WRE code: …).
MODULE A
1. Assess a patient’s learning needs (Code: IB6) [Difficulty: ELE: R, Ap; WRE: An]
It is very important to determine what the patient understands about his or her cardiopulmonary condition and its treatment. If the patient is found to need additional teaching in some area, it should be incorporated into the respiratory care plan. See Chapter 1 for more discussion on teaching methods.
2. Explain the planned therapy and goals to a patient in understandable terms to achieve optimal therapeutic outcomes (Code: IIIA6) [Difficulty: ELE: R, Ap; WRE: An]
3. Counsel a patient and family concerning smoking cessation (Code: IIIK6) [Difficulty: ELE: R, Ap; WRE: An]
MODULE B
1. Interview the patient to determine the presence of dyspnea, sputum production, and exercise tolerance (Code: IB5c) [Difficulty: ELE R, Ap; WRE: An]
c. Out-of-home activities
See Chapter 1 for the discussion on interviewing a patient about sputum production. The patient with chronic and severe cardiopulmonary disease may describe a very restricted and limited lifestyle. Extra O2 may have only limited benefit. The patient with chronic, but moderate, cardiopulmonary disease can live a somewhat limited but full lifestyle. Extra O2 may help greatly at times when the patient becomes short of breath. The otherwise healthy patient with an acute cardiopulmonary disease should describe a previously full and enjoyable lifestyle. Extra O2 may be needed now, but it is hoped that it will not be needed upon recovery.
2. Interview a patient to determine his or her social history (e.g., smoking, substance abuse) (Code: IB5e) [Difficulty: ELE: R; WRE: Ap]
The following questions can be asked of the family of a minor child:
3. Interview the patient to determine his or her nutritional status (ELE code: IB5d) [ELE difficulty: R]
4. Instruct the patient and family to assure safety and infection control (Code: IIIK7) [Difficulty: ELE: R, Ap; WRE: An]
Evaluate the following aspects of the patient’s home environment:
5. Home sleep apnea management
b. Interpret the results of overnight pulse oximetry (Code: IB10q) [Difficulty: ELE: R, Ap; WRE: An]
While it less expensive to perform overnight pulse oximetry in the home than polysomnography in the hospital, most patients who are suspected of having sleep-disordered breathing will be evaluated in the hospital. See the discussion on sleep-disordered breathing and overnight pulse oximetry in Chapter 18.
6. Apnea monitoring
b. Perform apnea monitoring (Code: IB9p) [Difficulty: ELE: R, Ap; WRE: An]
Apnea monitoring is indicated in an infant who has documented periods of apnea of prematurity resulting from an immature central nervous system. This condition is most commonly seen in infants younger than 35 weeks’ gestational age. The usual monitoring guidelines include apneic periods that last longer than 20 seconds and are associated with bradycardia with a heart rate of less than 100 beats/min. Hypoxemia is often demonstrated by cyanosis, pallor, or documented desaturation through pulse oximetry. In addition, the infant may show marked limpness, choking, or gagging. Other conditions such as intracranial hemorrhage, patent ductus arteriosus, upper airway obstruction, hypermagnesemia, infection, and maternal narcotic agents, for example, should be ruled out before apnea of prematurity is confirmed. If this is the infant’s problem, it is usually outgrown by the time the infant is 40 weeks’ postconceptional age. Home apnea monitoring is not indicated in normal infants, in preterm infants without symptoms of apnea, or to test for sudden infant death syndrome (SIDS). See Box 17-1 for guidelines on starting and stopping home apnea monitoring.
BOX 17-1 Guidelines for Starting and Stopping Home Apnea Monitoring
Two electrodes are usually placed where the greatest amount of movement occurs during breathing. Most often, this is on the infant’s upper chest between the nipples and armpits (Figure 17-1). With older infants, the electrodes might have to be placed on the sides over the lower ribs. Occasionally one electrode is placed on the chest and the other on the infant’s abdomen. Some monitoring systems require that a Velcro belt be placed around the infant over the electrodes to secure their positions. (Obviously this works only if both electrodes are on the chest.) Other systems employ electrodes with an adhesive. In either case, for best results, the infant’s chest should be washed with mild soap and water and dried before the electrodes are placed. This results in the best electrical conduction. Do not use baby oils, lotions, or powders over the electrode sites. Attach the lead wires to the electrodes. These connect to the patient cable that is then connected to the monitor. Occasionally static electricity causes some interference with the signal. A third chest electrode is then added to act as a ground wire.
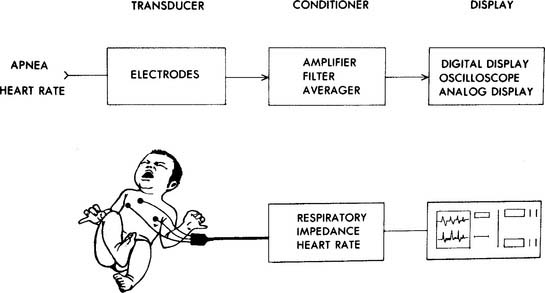
Figure 17-1 Block diagram for impedance apnea and heart rate monitor.
(From Lough MD. In Lough MD, Williams TJ, Rawson JE, editors: Newborn respiratory care, St Louis, 1979, Mosby.)
The monitor should be plugged into a working electrical outlet and turned on. Set the unit to charge the internal battery so that it can be made portable for later use. Confirm that the infant’s respiratory and heart rates are being sensed and displayed. If pulse oximetry is a feature on the unit, the probe should be properly placed on the infant, and an Spo2 value should be displayed. Set the high and low alarm values according to the physician’s orders or established protocols. For example:
7. Modify respiratory care procedures for use in the home (Code: IIIK8) [Difficulty: ELE: R, Ap; WRE: An]
MODULE C
1. Interview the patient to determine the presence of dyspnea, sputum production, and exercise tolerance (Code: IB5c) [Difficulty: ELE: R, Ap; WRE: An]
c. Out-of-home activities
If necessary, review the discussion on sputum production in Chapter 1. The patient with chronic and severe cardiopulmonary disease will describe a very restricted and limited lifestyle. Extra oxygen may have only a limited benefit. The patient with chronic, but moderate, cardiopulmonary disease is able to live a somewhat limited but full lifestyle. Extra oxygen may help greatly at times when the patient becomes short of breath. The otherwise healthy patient who has an acute cardiopulmonary disease should describe a previously full and enjoyable lifestyle. Extra oxygen may be needed now but not on recovery.
2. Timed walk test (e.g., 6-minute walk)
a. Perform a 6-minute walk (Code: IB9h) [Difficulty: ELE: R; WRE: Ap, An]
A 6-minute walk procedure involves the therapist having a patient walk as far as possible in 6 minutes and noting the distance covered. (Or, the distance that can be covered in a 12-minute walk test.) A timed walk test is easy to perform, is generally well tolerated, and directly relates to pulmonary rehabilitation activities. See the discussion on stress testing in Chapter 18 for information on evaluating a patient before a walk test and contraindications to exercise testing that may apply to a patient performing a timed walk.
Ideally, repeated tests should be performed at the same time each day and at least 2 hours after a meal. Basic equipment for the walk test includes a straight hallway at least 100 feet long that is marked at intervals for distance, a stopwatch, and a pulse oximeter. Record the temperature in the hallway. Be aware of two outside factors that can alter a patient’s performance. First, the so-called practice or learning effect can alter performance. The practice effect means that with repeated attempts, the patient will probably walk farther each time. Therefore the patient should perform at least two 6-minute timed walks that are measured and reported. The patient may rest for about 15 minutes between each walk test. Second, positive encouragement and feedback from the respiratory therapist can boost the patient’s walking distance. Therefore when and how encouragement is given need to be standardized with all patients. See Box 17-2 for a recommended 6-minute walk protocol.
BOX 17-2 Suggested Protocol for a 6-Minute Timed Walk Test
* The 10-point Borg Scale allows the patient to assign a numeric value of 1 to 10 to his/her feeling of dyspnea. A large poster of the Borg Scale is placed so the patient can easily see it during the walk test. Before and after the test the patient is asked to rate his/her dyspnea. For example, a score of 1 indicates very slight dyspnea, 5 is severe dyspnea, and 10 is maximal dyspnea.
b. Interpret the results of a 6-minute walk (Code: IB10h) [Difficulty: ELE: R, Ap; WRE: An]
The following indicate that the patient’s health is deteriorating:
c. General considerations in a graded exercise program
The patient’s physical condition must be evaluated before designing an exercise program. Besides chronic obstructive pulmonary disease (COPD), the patient may have other conditions that further limit his or her ability to safely participate in a rehabilitation program. See Box 17-3 for the suggested assessment parameters. If the patient is too ill or too limited in ability, he or she should not be placed into a rehabilitation program.
BOX 17-3 Patient Evaluation before Starting a Pulmonary Rehabilitation Program
See Chapter 4 for information on pulmonary function testing and Chapter 18 for information on cardiopulmonary stress testing.
A graded exercise program is an individually structured sequence of events that is designed to safely increase the patient’s exercise tolerance. It is a critical component of any pulmonary rehabilitation program. In 1942 the Council of Rehabilitation defined rehabilitation as “the restoration of the individual to the fullest medical, mental, emotional, social, and vocational potential of which he/she is capable” (Hodgkin, 1993). In 1974 The American College of Chest Physicians’ Committee on Pulmonary Rehabilitation adopted the following:
The patient with pulmonary disease who is inactive because of his or her condition experiences a slow deterioration in overall body function. It is well-known that physical activity is important for general health. Box 17-4 lists the effects of inactivity.
d. Benefits of an exercise program
Most authors agree with the following general therapeutic goals:
f. Program format
The closed-end format involves the program facilitator setting up a formal schedule of educational topics and exercise sessions. These group events commonly last from 1 to 3 hours and may occur from one to three times per week. The whole program can vary in length from 8 to 16 weeks, depending on the content. These events are attended by a group of patients who share a common problem and have common goals to address. One major advantage of this program is that most patients do better when they have peers to ask for emotional support. The facilitator will probably find that it is easier to schedule speakers when a established time frame can be set. The disadvantages of this program relate to the loss of individual goals and attention. If a patient misses a session, he or she will have to wait for the topic to be repeated at the next program. If the group is too large, the facilitator may not have time to help a patient with an individual goal.
g. Strength training
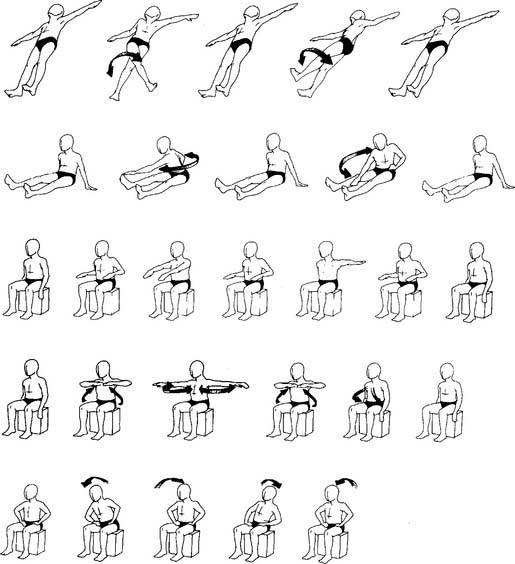
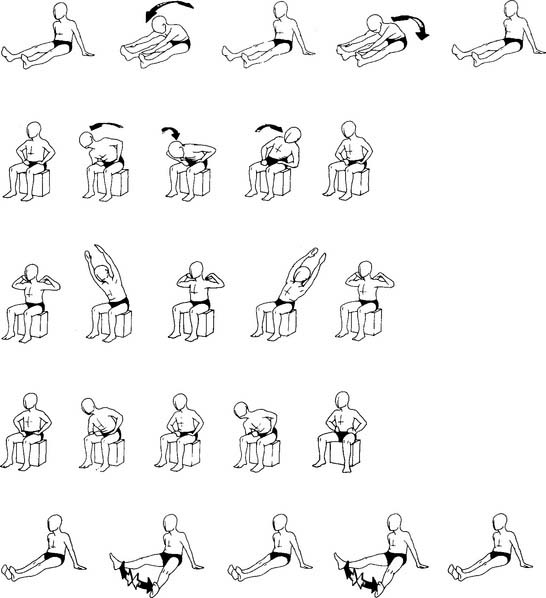
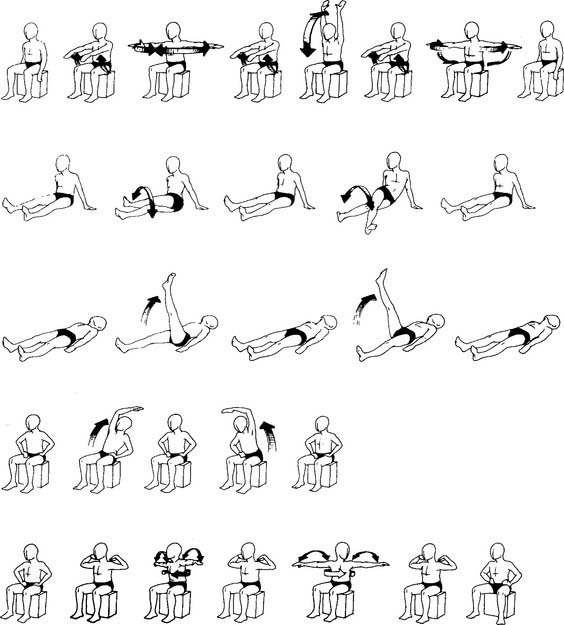
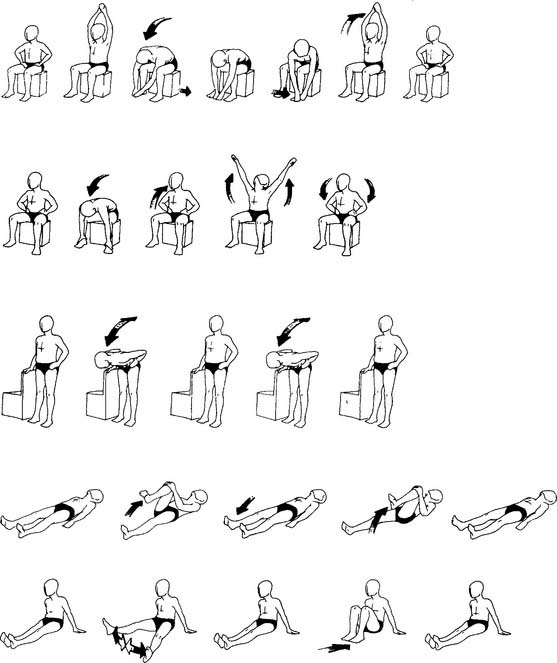
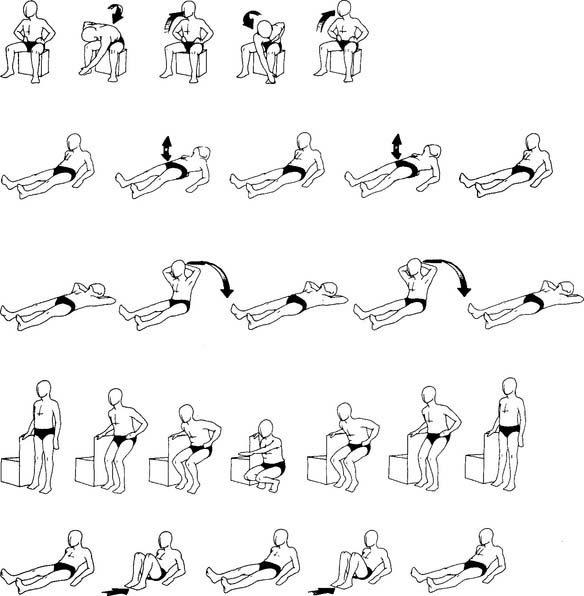
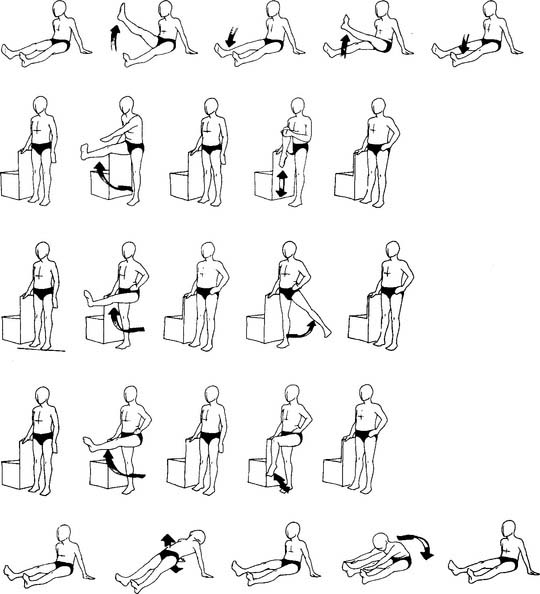
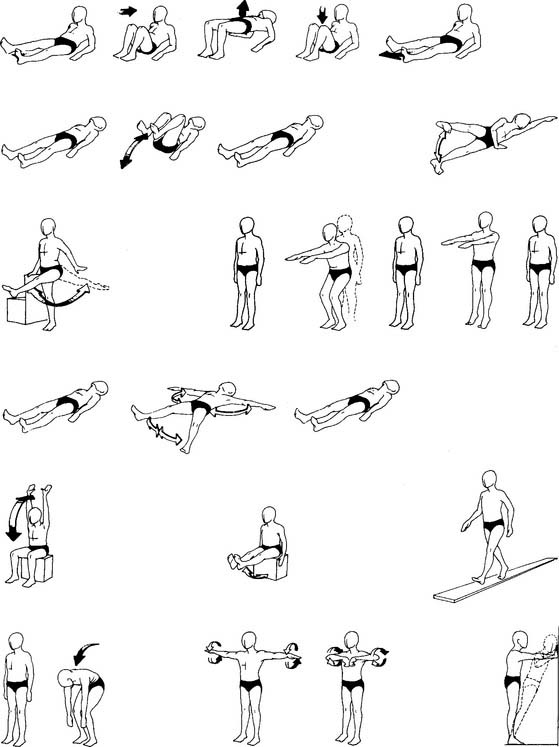
Before beginning strength training, the patient must perform calisthenics for about 10 minutes as a “warm-up.” It is important to stretch the muscles and joints and increase circulation before starting more vigorous activity. See Figure 17-2, groups 1 to 7, for a series of progressively more demanding calisthenic exercises. All patients should at least be able to perform the calisthenics shown in groups 1 and 2 for a warm-up. The patient must focus on breath control (pursed-lip breathing) during the warm-up period to avoid dyspnea.
(From May DF: Rehabilitation and continuity of care in pulmonary disease, St Louis, 1991, Mosby.)
Inspiratory muscle strengthening is done in two ways. First, the patient is told to take in a deep sigh and hold it for a brief time. This both stretches the rib cage and increases the workload of the primary and secondary inspiratory muscles. The deep sigh should be repeated several times. Second, the patient uses a specific inspiratory muscle training device. The PFLEX device is popular because it is inexpensive and can be gradually adjusted to increase the workload as the patient improves. Review the discussion in Chapter 7 and see Figure 7-1.
Finally, the patient should spend about 10 minutes in “cool-down” activities. This may involve more light calisthenics or slow walking. The cool-down period allows the body to return to a slower metabolic rate while still maintaining good circulation to the arms and legs. This helps to eliminate any lactic acid that might have accumulated in the muscles during the more vigorous exercise. Increased lactic acid may cause some muscle aches after exercise. Inform the patient that some muscle soreness may be felt the next day. It can be relieved by taking an antiinflammatory medication such as aspirin if the physician approves. See Box 17-5 for specific guidelines for a strength training program.
h. Endurance training
Endurance training is designed to improve the patient’s stamina to perform essential ADLs. It accomplishes this by improving the functioning of the patient’s cardiopulmonary and cardiovascular systems. When these systems perform better, they can meet the patient’s need for increased oxygen delivery to and carbon dioxide removal from exercising muscles.
Endurance training must be preceded by the patient performing calisthenics for about 10 minutes as a warm-up. Just as in strength training, it is important to stretch the muscles and joints and increase circulation before starting more vigorous activity. See Figure 17-2, groups 1 through 7, for a series of progressively more demanding calisthenic exercises. All patients should be able to at least perform the calisthenics shown in groups 1 and 2 for a warm-up.
The actual endurance exercise that is selected must meet the patient’s needs. He or she can walk, use a treadmill, ride a bicycle ergometer, swim, or do a combination of these. The method that is selected must be both practical and fun for the patient. For this reason, walking is usually the main activity; however, the upper body should not be ignored. An arm ergometer, rowing machine, or barbell weights can be used for upper-body endurance.
Maximum HR = maximum HR determined by either of the following formulas:
Determine the target HR for a 50-year-old patient (of either gender) who is enrolled in an endurance training program. The patient has a resting HR of 80 beats/min. The patient’s maximum heart rate is 170 (220 − 50 for the patient’s age = 170).
Target HR = (% intensity [maximum HR − resting HR]) + resting HR
Finally, as in strength training, the patient should spend about 10 minutes in “cool-down” activities. This may involve light calisthenics or slow walking. As discussed earlier, the cool-down period allows the body to return to a slower metabolic rate while still maintaining good circulation to the arms and legs. This helps to eliminate any lactic acid that may have built up in the muscles during the endurance exercise. See Box 17-5 for specific guidelines for an endurance training program.
MODULE D
1. Analyze available information to determine the patient’s pathophysiologic state (Code: IIIH1) [Difficulty: ELE: R, Ap; WRE: An]
In addition, review the information presented in Chapters 1, 3, 4, and 5. These chapters discuss bedside patient assessment, blood gas interpretation, pulmonary function testing, and hemodynamic monitoring that the NBRC has determined to be testable on the Entry Level Examination and Written Registry Examination. Be prepared to evaluate areas such as vital signs, breath sounds, blood gas values, pulmonary function results, and cardiac study results to determine the patient’s condition.
a. Determine the appropriateness of the prescribed therapy and goals for the patient’s pathophysiologic state (Code: IIIH3) [Difficulty: ELE: R, Ap; WRE: An]
b. Review the planned therapy to establish the therapeutic plan (Code: IIIH2a) [Difficulty: ELE: R, Ap; WRE: An]
Determination of the patient’s ideal therapeutic goals is best accomplished with a team approach. The patient’s physician, nurse, and respiratory therapist should work together. The first consideration should be the patient’s diagnosis. Then, it should be determined whether the patient’s condition is permanent, improving, or worsening. Objective information such as arterial blood gas results, pulmonary function testing results, chest x-ray film findings, sputum production, and vital signs must be evaluated. The patient’s physical capabilities should be considered when establishing therapeutic goals. The therapist must also evaluate the patient’s mental state. Is the patient emotionally prepared to return home and be taught about self-care or start a rehabilitation program? The therapeutic goals for each patient must be individualized. If the patient is not physically or emotionally ready to take care of himself or herself, the family or a paid care provider is needed. Following are common therapeutic goals:
c. Recommend changes in the therapeutic plan when indicated (Code: IIIH4) [Difficulty: ELE: R, Ap; WRE: An]
The following signs indicate that the patient is stable or making progress:
The following indicate that the patient’s health is deteriorating:
d. Educate the patient and family in health management (Code: IIIK4) [Difficulty: ELE: R, Ap; WRE: An]
Effective teaching methods include the following:
e. Terminate the treatment or procedure based on the patient’s response to therapy (Code: IIIF1) [Difficulty: ELE: R, Ap; WRE: An]
2. Develop the home care and pulmonary rehabilitation protocols (Code: IIIH6b) [Difficulty: ELE: R; WRE: Ap, An]
3. Apply the home care and pulmonary rehabilitation protocols (Code: IIIH8) [Difficulty: ELE: R, Ap; WRE: Ap]
4. Monitor the outcomes of home care and pulmonary rehabilitation protocols (Code: IIIH7b) [Difficulty: ELE: R, Ap; WRE: An]
The patient’s physical condition must be evaluated before designing a home care or rehabilitation program. Besides the primary diagnosis, the patient may have other conditions that further limit his or her ability to participate safely. If the patient is too ill or too limited in ability, he or she should not be placed into a home care or rehabilitation program.
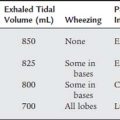
5. Record and evaluate the patient’s response to the treatment(s) or procedure(s), including the following:
a. Record and interpret the following: heart rate and rhythm, respiratory rate, blood pressure, body temperature, and pain level (Code: IIIA1b4) [Difficulty: ELE: R, Ap; WRE: An]
b. Record and interpret the patient’s breath sounds (Code: IIIAb3) [Difficulty: ELE: R, Ap; WRE: An]
6. Communicate information
a. Communicate information regarding the patient’s clinical status to appropriate members of the health care team (Code: IIIA2a) [Difficulty: ELE: R, Ap; WRE: An]
b. Communicate information relevant to coordinating patient care and discharge planning (Code: IIIA2a) [Difficulty: ELE: R, Ap; WRE: An]
c. Interact with a case manager (Code: IIIK5) [Difficulty: ELE: R, Ap; WRE: An]
American Association for Respiratory Care. Clinical Practice Guideline: Oxygen therapy in the home or alternate site health care facility—2007 revision & update. Respir Care. 2007;52:1063.
American Association for Respiratory Care. Clinical Practice Guideline: Discharge planning for the respiratory care patient. Respir Care. 1995;40:1308.
American Association for Respiratory Care. Clinical Practice Guideline: Long-term invasive ventilation in the home. Respir Care. 1995;40:1313.
American Association for Respiratory Care. Clinical Practice Guideline: Providing patient and caregiver training. Respir Care. 1996;41:658.
American Association for Respiratory Care. Clinical practice guideline: Pulmonary rehabilitation. Respir Care. 2002;47(5):617.
American Association for Respiratory Care. Clinical Practice Guideline: Suctioning the patient in the home. Respir Care. 1999;44:99.
American Association for Respiratory Care. Clinical Practice Guideline: Exercise testing for evaluation of hypoxemia and/or desaturation: 2001 revision & update. Respir Care. 2001;44:514.
Bell CW, Blodgett D, Goike C, et al. Home care and rehabilitation in respiratory medicine. Philadelphia: Lippincott, 1984.
Belman MJ, Wasserman K. Exercise training and testing in patients with chronic obstructive pulmonary disease. Basics Respir Dis. 1981;10(2):1-6.
Branson RD, Hess DR, Chatburn RL. Respiratory care equipment, ed 2. Philadelphia: Lippincott Williams & Wilkins, 1999.
Cairo JM, Pilbeam SP. Mosby’s respiratory care equipment, ed 8. St Louis: Mosby, 2009.
Christopher KL. At-home administration of oxygen. In: Kacmarek RM, Stoller JK, editors. Current respiratory care. Toronto: BC Decker, 1988.
Connors G, Hilling L, editors. American Association of Cardiovascular and Pulmonary Rehabilitation: guidelines for pulmonary rehabilitation programs. Champaign, Ill: Human Kinetics, 1993.
Des Jardins T, Burton GG. Clinical manifestations and assessment of respiratory disease, ed 5. St Louis: Mosby, 2006.
Edge RS. Infection control. In: Barnes TA, editor. Respiratory care practice. St Louis: Mosby, 1988.
Eubanks DH, Bone RC. Comprehensive respiratory care, ed 2. St Louis: Mosby, 1990.
Farzan S, Farzan D. A concise handbook of respiratory disease, ed 4. Stamford, Conn: Appleton & Lange, 1997.
Gardner DD, Wilkins RL. Patient education and health promotion. In Scanlan CL, Wilkins RL, Kacmarek RM, editors: Egan’s fundamentals of respiratory care, ed 9, St Louis: Mosby, 2009.
Gilmartin M. Transition from the intensive care unit to home: patient selection and discharge planning. Respir Care. 1994;39:456.
Gourley DA. Respiratory home care. In: Wyka KA, Mathews PJ, Clark WF, editors. Foundations of respiratory care. Albany, NY: Delmar, 2002.
Heuer AJ, Scanlan CL. Respiratory care in alternative sites. In Scanlan CL, Wilkins RL, Kacmarek RM, editors: Egan’s fundamentals of respiratory care, ed 9, St Louis: Mosby, 2009.
Hodgkin JE. Home care and pulmonary rehabilitation. In: Kacmarek RM, Stoller JK, editors. Current respiratory care. Toronto: BC Decker, 1988.
Hodgkin JE, Celli BR, Connors GL. Pulmonary rehabilitation: guides to success, ed 3. Philadelphia: Lippincott Williams & Wilkins, 2000.
Hodgkin JE, Connors GA. Pulmonary rehabilitation. In Burton GG, Hodgkin JE, Ward JJ, editors: Respiratory care: a guide to clinical practice, ed 4, Philadelphia: Lippincott, Williams and Wilkins, 1997.
Holden DA, Stelmach KD, Curtis PS, et al. The impact of a rehabilitation program on functional status of patients with chronic lung disease. Respir Care. 1990;35:332.
Jones PW. Measurement of breathlessness. In: Hughes JMB, Pride NB, editors. Lung function tests: physiological principles and clinical applications. London: W. B. Saunders, 2000.
Kwiatkowski CA, Tougher-Decker R, O’Sullivan-Maillet J. Nutritional aspects of health and disease. In Scanlan CL, Wilkins RL, Stoller JK, editors: Egan’s fundamentals of respiratory care, ed 7, St Louis: Mosby, 1999.
Lewis ML, Hagarty EM, Lawlor B. Home respiratory care. In: Fink JB, Hunt GE, editors. Clinical practice in respiratory care. Philadelphia: Lippincott Williams & Wilkins, 1999.
Lucas J, Golish JA, Sleeper G, et al. Home respiratory care. Norwalk, Conn: Appleton & Lange, 1988.
MacIntyre NR. Pulmonary rehabilitation. In: Hess DR, MacIntyre NR, Mishoe SC, et al, editors. Respiratory care principles and practices. Philadelphia: WB Saunders, 2002.
May DF. Rehabilitation and continuity of care in pulmonary disease. St Louis: Mosby, 1991.
McInturff SL, O’Donohue WJJr. Respiratory care in the home and alternate sites. In Burton GG, Hodgkin JE, Ward JJ, editors: Respiratory care: a guide to clinical practice, ed 4, Philadelphia: JB Lippincott, 1997.
Mulligan SC, Masterson JG, Devane JG, et al. Clinical and pharmacokinetic properties of a transdermal nicotine patch. Clin Pharmacol Ther. 1990;47:331.
Nett LM. The physician’s role in smoking cessation. Chest Suppl. 1990;97(2):28s.
Petty TL. Pulmonary rehabilitation. Basics Respir Dis. 1975.
Petty TL. Pulmonary rehabilitation: better living with new technology. Respir Care. 1985;30:98.
Petty TL, Nett LM. Enjoying life with emphysema. Philadelphia: Lea & Febiger, 1987.
Pulmonary rehabilitation: official American Thoracic Society statement. Am Rev Respir Dis. 1981;124:663.
Rennard SI, Daughton D. Transdermal nicotine for smoking cessation. Respir Care. 1993;38:290.
Sobush D, Dunning M, McDonald K. Exercise prescription components for respiratory muscle training: past, present, and future. Respir Care. 1985;30:34.
Taylor C, Lillis C, LeMond P. Fundamentals of nursing: the art and science of nursing care, ed 2. Philadelphia: JB Lippincott, 1993.
White GC. Equipment theory for respiratory care, ed 4. Albany, NY: Delmar, 2005.
Wilkins RL, Dexter JR. Respiratory disease: a case study approach to patient care, ed 2. Philadelphia: FA Davis, 1998.
Wyka KA. Cardiopulmonary rehabilitation. In Wilkins RL, Stoller JK, Kacmarek RM, editors: Egan’s fundamentals of respiratory care, ed 9, St Louis: Mosby, 2009.
Wyka KA. Pulmonary rehabilitation. In: Wyka KA, Mathews PJ, Clark WF, editors. Foundations of respiratory care. Albany, NY: Delmar, 2002.
SELF-STUDY QUESTIONS FOR THE ENTRY LEVEL EXAM See page 602 for answers
SELF-STUDY QUESTIONS FOR THE WRITTEN REGISTRY EXAM See page 627 for answers