Chapter 8
Holter Monitors, Event Monitors, Ambulatory Monitors, and Implantable Loop Recorders
1. What are the major indications for ambulatory electrocardiography (AECG) monitoring?
AECG monitoring allows the noninvasive evaluation of a suspected arrhythmia during normal daily activities. It aids in the diagnosis, documentation of frequency, severity, and correlation of an arrhythmia with symptoms such as palpitations, lightheadedness, or overt syncope. AECG monitoring can be extremely helpful in excluding an arrhythmia as a cause for a patient’s symptoms if there is no associated event during monitoring. AECG can also be used to assess antiarrhythmic drug response in patients with defined arrhythmias. Occasionally AECG is also used in other situations. The current major indications for AECG monitoring, from the American College of Cardiology/American Heart Association (ACC/AHA), are given in Box 8-1.
2. What are the different types of AECG monitoring available?
 A Holter monitor constantly monitors and records two to three channels of ECG data for 24 to 48 hours. It is ideal for patients with episodes that occur daily.
A Holter monitor constantly monitors and records two to three channels of ECG data for 24 to 48 hours. It is ideal for patients with episodes that occur daily.
 An event monitor constantly monitors two to three channels of ECG data for 30 to 60 days. However, it will only record events when the patient experiences a symptom and presses a button that triggers the event monitor to store ECG data 1 to 4 minutes before and 1 to 2 minutes after the event. Some event monitors will also store arrhythmias that are detected by the monitor itself, based on preprogrammed parameters. An event monitor is appropriate for patients with episodes that occur weekly or monthly.
An event monitor constantly monitors two to three channels of ECG data for 30 to 60 days. However, it will only record events when the patient experiences a symptom and presses a button that triggers the event monitor to store ECG data 1 to 4 minutes before and 1 to 2 minutes after the event. Some event monitors will also store arrhythmias that are detected by the monitor itself, based on preprogrammed parameters. An event monitor is appropriate for patients with episodes that occur weekly or monthly.
 Ambulatory real-time cardiac monitoring has various monikers. it has been termed ambulatory telemetry, real-time continuous cardiac monitoring, or mobile cardiac outpatient telemetry (MCOT). Ambulatory telemetry is a monitoring system that continuously records a 1- to 3-lead strip for 14 to 30 days. Depending on the vendor, the ECG data is either stored for offline interpretation or instantaneously transmitted for interpretation by a monitoring technician. In cases where the rhythm is monitored by a technician in real time, the patient or physician can be contacted immediately after an arrhythmia has been detected, to minimize delays in treatment. No patient action is necessary for an arrhythmia to be stored, and patient compliance can easily be assessed. These features facilitate the detection of silent or asymptomatic arrhythmias.
Ambulatory real-time cardiac monitoring has various monikers. it has been termed ambulatory telemetry, real-time continuous cardiac monitoring, or mobile cardiac outpatient telemetry (MCOT). Ambulatory telemetry is a monitoring system that continuously records a 1- to 3-lead strip for 14 to 30 days. Depending on the vendor, the ECG data is either stored for offline interpretation or instantaneously transmitted for interpretation by a monitoring technician. In cases where the rhythm is monitored by a technician in real time, the patient or physician can be contacted immediately after an arrhythmia has been detected, to minimize delays in treatment. No patient action is necessary for an arrhythmia to be stored, and patient compliance can easily be assessed. These features facilitate the detection of silent or asymptomatic arrhythmias.
 An implantable loop recorder (ILR) is an invasive monitoring device allowing long-term monitoring and recording of a single ECG channel for over a year. It records events similarly to an event monitor, based on patient’s symptoms or automatically based on heart rate. It is best reserved for patients with more infrequent episodes occurring greater than 1 month apart from each other.
An implantable loop recorder (ILR) is an invasive monitoring device allowing long-term monitoring and recording of a single ECG channel for over a year. It records events similarly to an event monitor, based on patient’s symptoms or automatically based on heart rate. It is best reserved for patients with more infrequent episodes occurring greater than 1 month apart from each other.
An ILR is surgically placed subcutaneously below the left shoulder. As discussed earlier, it can continuously monitor bipolar ECG signals for more than 1 year. The patient may use a magnetic activator held over the device to signal an event at the time of symptoms. In addition, the device automatically records episodes of bradycardia and tachycardia (Figs. 8-1A and 8-1B). The device is then interrogated with an external programmer, and recorded events are reviewed (Fig. 8-2) as with a permanent pacemaker. After a diagnosis is obtained, the device is surgically extracted. In patients with unexplained syncope, an ILR yields a diagnosis in more than 90% of patients after 1 year.
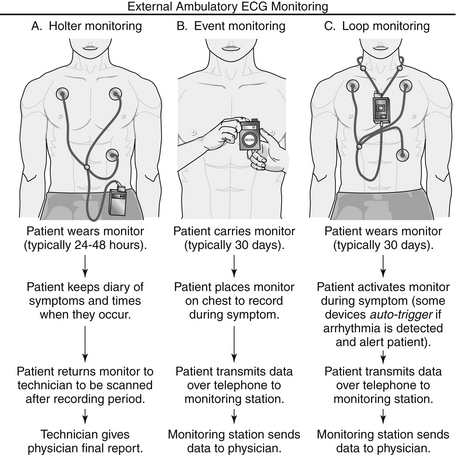
Figure 8-1A Types of ambulatory monitors available in clinical practice. ECG, Electrocardiogram. (From Mittal S, Movsowitz C, Steinberg JS: Ambulatory external electrocardiographic monitoring: focus on atrial fibrillation, J Am Coll Cardiol 58:1741-1749, 2011.)
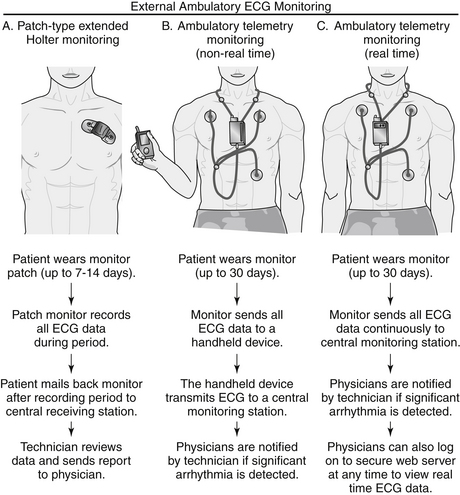
Figure 8-1B Patch-type extended Holter and ambulatory telemetry monitors. ECG, Electrocardiogram. (From Mittal S, Movsowitz C, Steinberg JS: Ambulatory external electrocardiographic monitoring: focus on atrial fi brillation, J Am Coll Cardiol 58:1741-1749, 2011.)
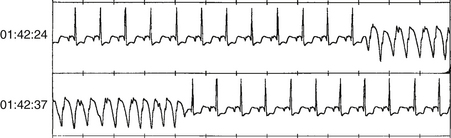
Figure 8-2 Representative printout from an implantable loop recorder demonstrating a run of nonsustained ventricular tachycardia.
4. Do patients with a pacemaker or implantable cardioverter-defibrillators (ICDs) require Holter monitors for detecting atrial arrhythmias?
5. Is every “abnormality” detected during monitoring a cause for concern?
In contrast, often of concern are frequent and complex atrial and ventricular rhythm disturbances that are less commonly observed in normal subjects, including second-degree AV block type II, third-degree AV block, sinus pauses longer than 3 seconds, marked bradycardia during waking hours, and tachyarrhythmias (Fig. 8-3). One of the most important factors for any documented arrhythmia is the correlation with symptoms. In some situations, even some “benign” rhythms may warrant treatment if there are associated symptoms.
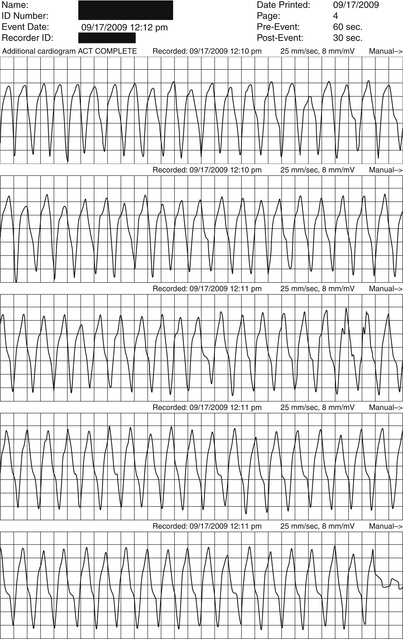
Figure 8-3 Sustained ventricular tachycardia detected by a Holter monitor in a patient with daily episodes of palpitations and lightheadedness.
6. What is the diagnostic yield of Holter monitors, event monitors, and ILRs in palpitations and syncope?
Choosing a Holter monitor, an event monitor, or an ILR depends on the frequency of symptoms. In patients with palpitations, the highest diagnostic yield occurred in the first week, with 80% of patients receiving a diagnosis. During the next 3 weeks, only an additional 3.4% of patients receive a diagnosis. In patients with recurrent but infrequent palpitations (less than one episode per month lasting less than 1 minute), ILR resulted in a diagnosis in 73% of patients. In contrast to palpitations, syncope usually requires a longer monitoring period to achieve a diagnosis, with the highest yield coming from the implantation of an ILR (Fig. 8-4).
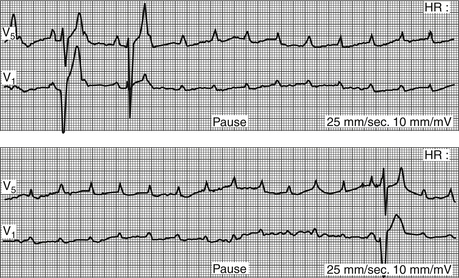
Figure 8-4 Ambulatory monitor tracing in an elderly patient with intermittent syncope. The tracing shows complete heart block with a 9-second pause. (From Jaeger FJ: Cardiac arrhythmias. In: Cleveland Clinic: Current clinical medicine, ed 2, Philadelphia, 2010, Saunders, Philadelphia, pp 114-128.)
7. How often are ventricular arrhythmias identified in apparently healthy subjects during AECG monitoring?
Ventricular arrhythmias are found in 40% to 75% of normal persons as assessed by 24- to 48-hour Holter monitors. The incidence and frequency of ventricular ectopy increases with age, but this has no impact on long-term prognosis in apparently healthy subjects.
8. What is the role of AECG monitoring in patients with known ischemic heart disease?
Although ejection fraction after myocardial infarction (MI) is one of the strongest predictors of survival, AECG monitoring can be helpful in further risk stratification. Ventricular arrhythmias occur in 2% to 5% of patients after transmural infarction in long-term follow-up. In the post-MI patient, the occurrence of frequent premature ventricular contractions (PVCs) (more than 10 per hour) and nonsustained ventricular tachycardia (VT) by 24-hour monitoring is associated with a 1.5- to 2.0-fold increase in death during the 2- to 5-year follow-up, independent of left ventricular (LV) function.
9. Can Holter monitors assist in the diagnosis of suspected ischemic heart disease?
10. What have Holter monitors demonstrated about angina and its pattern of occurrence?
11. What is a signal-averaged ECG?
12. When should a signal-averaged ECG be considered?
The use of SAECG to identify late potentials and those post-MI patients at greatest risk for sudden death has been extensively evaluated. Although an association exists between late potentials and increased risk of ventricular arrhythmias after MI, the positive predictive value of SAECG is low. In the Coronary Artery Bypass Graft (CABG) Patch Trial, patients with an abnormal SAECG and depressed ejection fraction who were to undergo cardiac surgery were randomized to ICD implantation or no implantation and then followed for an average of 32 months. The study could detect no benefit for ICD implantation in this patient population with abnormal SAECGs. A study of SAECG use in patients treated with reperfusion, mainly primary percutaneous coronary intervention (PCI), did not find SAECG to be a useful risk stratification tool in this patient population. In current practice, the test is rarely used for risk stratification.
13. What is microvolt T-wave alternans and does it predict outcomes in certain patients?
14. Does heart-rate variability have predictive value in certain patients?
Bibliography, Suggested Readings, and Websites
1. American College of Cardiology: Signal-averaged electrocardiography. ACC Expert Consensus Document. J Am Coll Cardiol. 1996;27:238–249.
2. Assar, M.D., Krahn, A.D., Klein, G.J., et al. Optimal duration of monitoring in patients with unexplained syncope. Am J Cardiol. 2003;92:1231–1233.
3. Bass, E.B., Curtiss, E.I., Arena, V.C., et al. The duration of Holter monitoring in patients with syncope: is 24 hours enough? Arch Intern Med. 1990;50:1073–1078.
4. Bigger, T.J., Jr. Prophylactic use of implanted cardiac defibrillators in patients at high risk for ventricular arrhythmias after coronary-artery bypass graft surgery. Coronary Artery Bypass Graft (CABG) Patch Trial investigators. N Engl J Med. 1997;337:1569–1575.
5. Chow, T., Kereiakes, D.J., Bartone, C., et al. Microvolt T-wave alternans identifies patients with ischemic cardiomyopathy who benefit from implantable cardioverter-defibrillator therapy. J Am Coll Cardiol. 2007;49:50–58.
6. Crawford, M.H., Bernstein, S.J., Deedwania, P.C., et al. ACC/AHA guidelines for ambulatory electrocardiography: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the Guidelines for Ambulatory Electrocardiography). J Am Coll Cardiol. 1999;34:912–948.
7. Dixit, S., Marchlinski, F.E. Role of continuous monitoring for optimizing management strategies in patients with early arrhythmia recurrences after atrial fibrillation ablation. Circ Arrhythm Electrophysiol. 2011;4:791–793.
8. Epstein, A.E., Hallstrom, A.P., Rogers, W.J., et al. Mortality following ventricular arrhythmia suppression by encainide, flecainide, and moricizine after myocardial infarction. The original design concept of the Cardiac Arrhythmia Suppression Trial (CAST). JAMA. 1993;270(20):2451–2455.
9. Kadish, A.H., Reiffel, J.A., Clauser, J., et al. Frequency of serious arrhythmias detected with ambulatory cardiac telemetry. Am J Cardiol. 2010;105(9):1313–1316.
10. Kennedy, H.L., Whitlock, J.A., Sprague, M.K., et al. Long-term follow-up of asymptomatic healthy subjects with frequent and complex ventricular ectopy. N Engl J Med. 1985;312:193–197.
11. Maggioni, A.P., Zuanetti, G., Franzosi, M.G., et al. Prevalence and prognostic significance of ventricular arrhythmias after acute myocardial infarction in the fibrinolytic era. GISSI-2 results. Circulation. 1993;87:312–322.
12. Mittal, S., Movsowitz, C., Steinberg, J.S. Ambulatory external electrocardiographic monitoring: focus on atrial fibrillation. J Am Coll Cardiol. 2011;58:1741–1749.
13. Narayan SM: T-Wave (Repolarization) Alternans: Clinical Aspects. In Basow, DS, editor: UpToDate, Waltham, MA, 2013, UpToDate. Available at: http://www.uptodate.com/contents/t-wave-repolarization-alternans-clinical-aspects. Accessed March 26, 2013 www.utdol.com.
14. Narayan SM, Cain ME: Clinical Applications of the Signal-Averaged Electrocardiogram: Overview. In Basow, DS, editor: UpToDate, Waltham, MA, 2013, UpToDate. Available at: http://www.uptodate.com/contents/clinical-applications-of-the-signal-averaged-electrocardiogram-overview. Accessed March 26, 2013.
15. Zeldis, S.M., Levine, B.J., Michaelson, E.L., et al. Cardiovascular complaint. Correlation with cardiac arrhythmias on 24 hour electrocardiographic monitoring. Chest. 1980;78:456–461.
16. Zimetbaum, P., Goldman, A. Ambulatory arrhythmia monitoring: choosing the right device. Circulation. 2010;122:1629–1636.
17. Zipes, D.P., Camm, A.J., Borggrefe, M., et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. J Am Coll Cardiol. 2006;48:1064–1108.





















