CHAPTER 1 Historical Overview of Neurosurgery
Those which are Masters and Professors chosen to performe the like operation, ought indeede to have a Lyons heart, a Ladies hand, and a Haukes eye, for that it is a worke of no small importance.1
The father of medicine even further detailed this concept when he stated: Nullum capitis vulnus contemnendum est (No head injury should be considered trivial)—Hippocrates.2
Neurosurgery in the Prehistoric Period
Neurosurgery is in many ways one of the most ancient of professions. Early man clearly recognized that to bring down the enemy, a blow to the head was the quickest means. To accomplish this goal a number of weapons, in particular, clubs, were fashioned to inflict these injuries. In a number of anthropologic collections around the world are examples of skulls with head injuries, and more remarkable are a number of skulls with successful trephinations (i.e., meaning that the patient clearly survived surgical opening of the skull) (Fig. 1-1).3–5 In some cultures, for example, the early Peruvians, there exist many skulls that show evidence of trephinations and in most cases for reasons that remain unknown. There has been speculation that this procedure was performed for religious or medical reasons, but because of the lack of any documentation, we have no understanding today why these procedures were done. Figure 1-1 illustrates examples of trephinated skulls from the early Chimu culture in Peru.
Ancient Egyptian Neurosurgery
The earliest known written documents that relate to early neurosurgery date from the ancient Egyptian period. This period covers some 30 successive dynasties and produced the earliest known practicing physician—Imhotep (1300 BC). This period of history provided the earliest known medical and surgical material. Today, there are three existing documents available that have relevance to medicine. These papyri, which are named after their early owners, are the Ebers, Hearst, and Edwin Smith papyri.6–8
The oldest medical text dates from this early civilization and was written some 500 years after Hammurabi. This text, now called the Ebers papyrus, includes 107 pages of hieratic writing and is of interest for its extensive discussions of contemporary surgical practice. Included are discussions of the removal of tumors, as well as recommendations for the surgical drainage of abscesses.6
The oldest work that deals extensively with surgical techniques is the Edwin Smith papyrus. This work appears to have been intended to be a surgical textbook. It was originally written sometime after 1700 BC in the time of the New Kingdom. This papyrus scroll is 15 ft in length and 1 ft in width. The surviving text consists solely of a list of 48 cases, including those dealing with injuries to the spine and cranium. The format is such that each case is discussed with a diagnosis, followed by a formulated prognosis. As a result of the scholarly research of James Breasted, this papyrus has now been translated from the original hieroglyphics. The original document is currently in the possession of the New York Academy of Medicine.8,9 We provide two cases to show the insight and some of the techniques illustrated in this early historical papyrus.
Case Five
Title: Instructions concerning a gaping wound in his head, smashing his skull.
Other than the isolated cases found in these remaining papyri, little can be gleaned from them on the actual practice of neurosurgery.9 It is evident from these writings that the Egyptian physician recognized head injury and would elevate a skull fracture if necessary. At the same time, if the injury appeared too be too severe, no treatment was advocated. The early “neurosurgeon” had to wait until the development of the Greek schools of medicine, for it was then that the management and codification of head injury were first formulized.
Classical Period—Greek and Byzantine Neurosurgery
Hippocratic School
The intellectual evolution of neurological surgery originated in the golden age of Greece with the founding of the Alexandrian school in 300 BC. For the first time, open anatomic dissection was incorporated into formal lectures,10 and the concept of a surgeon performing surgery on the head and spine became formalized. Because of both sporting injuries, in particular, gladiator injuries, and wars, head injuries appear to have been plentiful and provided opportunities to develop the early skills of neurosurgery.
The earliest medical writings from this period are those of Hippocrates (460-370 BC), the most celebrated of the Asclepiadeans (Fig. 1-2).11–13 Classical philologists think that many of the writings attributed to Hippocrates, however, were composed by members of the Hippocratic school. The Hippocratic collection presents clinical cases based mainly on observation, and in most cases only the simplest of theories are offered. There are a number of neurological cases within the Hippocratic corpus. In reviewing these cases one finds a rather sophisticated understanding of head injury. Hippocrates was the first to describe a number of neurological injuries, most resulting from battlefield injuries. The vulnerability of the brain to injury was categorized by location, from lesser to greater, with injury to the bregma being represented as a higher risk than one to the temporal region, which in turn was more dangerous than an injury to the occipital region.14–16 Hippocrates devoted a full chapter to injuries of the head, De Capitis Vulneribus, a work that deals with the diagnosis and management of head injuries. The work divides head injuries into five categories based on details of the skull fracture and is the first systematic work devoted to head injuries. Five types of fractures are described: linear fracture, contusion, depressed fracture, hedra (or dent) occurring with and without fracture, and contrecoup fracture.14 There is nothing to suggest that the neurological condition of the patient had any bearing on the surgical indications. Surgery was advised according to the type of fracture. The greater the injury to the skull, the less the need for trephination. The technical aspects of the process of trephination are presented in a curious mixture of sound advice and incomprehensible admonitions.
FIGURE 1-2 Title page from the first printed edition of the writings of Hippocrates—1525.
(From Panourias JG, Skiadas PK, Saklas DE, et al. Hippocrates: a pioneer in the treatment of head injuries. Neurosurgery. 2005;37:181-189.)
These Hippocratic writings contain numerous anatomic descriptions, even though human dissection appeared to not be routinely practiced. The Greeks were also without an anatomic vocabulary, which was not introduced until Galen standardized use of the Latin language in medicine. These deficiencies retarded the development of standardized anatomic procedures and the practice of surgery. Despite these drawbacks, there are within the Hippocratic writings a number of interesting neurological case studies that reflect a view of the early practice of neurosurgery (Fig. 1-3).
One of earliest descriptions of subarachnoid hemorrhage appears in the Aphorisms:
Herophilus of Chalcedon (ca. 300 BC)
From the region of the Bosporus, among the crowded schools of Alexandria, came Herophilus, a pupil of Praxagoras and Chrisippus and a member of the educated dynasty of Ptolemy. According to his writing, Herophilus performed dissection on humans, not on animals as was the common practice then.18–20 Herophilus and Galen later were key figures in the task of developing an anatomic nomenclature and in forming a much needed language of anatomy. In examining the nervous system, Herophilus’ neurological contributions included anatomically following the origin of nerves to the spinal cord. He was the first to recognize the difference in motor and sensory tracts. He made a further important differentiation between nerves and tendons, thereby correcting a common earlier error. Herophilus was the first to detail the anatomy of the brain ventricles and venous sinuses. The description of the “confluens of the sinuses,” or torcular Herophili (torcula means wine press), comes from his early investigations. The first description and naming of the choroid plexus (plexus choroides) come from Herophilus, and it was so named because of its resemblance to the vascular membrane of the fetus. He gave the first detailed account of the fourth ventricle and of that peculiar arrangement at its base, which he called the calamus scriptorius because it “resembles a pen in writing”—Aναγλυϕη τχ χαλαµχ. Among his many other contributions was recognition of the brain as the central organ of the nervous system and the seat of intelligence.19
Herophilus was not without errors in his writings. Perhaps the worst was his introduction into the anatomic literature of one of the longest-standing errors—that of the rete mirabile, a structure present in ungulates but notably lacking in higher primates. In ungulates this structure acts as an anastomotic network at the base of the brain, a structure that the Greeks incorporated into the early physiologic theories of brain function.21 The rete mirabile was later elaborated in further detail by Galen of Pergamum and codified by Islamic and medieval writers. This anatomic error remained firmly embedded in the anatomic literature until the 16th century, when it finally became challenged in the accounts of Andreas Vesalius (1514-1564) and Giacomo Berengario da Carpi (1460-1530).22–24 Both these writers, who performed their own human dissections, clearly recognized that the rete mirabile did not exist in humans. It is possible that the human cavernous sinus confused the early writers and they in turn thought that this represented the rete mirabile.
Aulus Aurelius Cornelius Celsus (25 BC–50 AD)
Celsus (Fig. 1-4A) was neither a physician nor a surgeon, but rather an intellectual patrician and a medical encyclopedist who attempted to compile all the important writings of his time. His writings had an important early influence on medicine and surgery. As counselor to the emperors Tiberius and Caligula, Celsus was held in great esteem. His book on medicine titled De Medicina25,26 (Fig. 1-4B) is now considered one of the most important early medical documents after the Hippocratic writings. As a result of this work originally being lost, Celsus was one of the few major authors not transcribed by the Islamic/Arabic writers. This changed in 1443, when an early Celsus manuscript was uncovered by Thomas Sarazanne (later Pope Nicolas V) and reintroduced to the medical community. With the introduction of movable type, Celsus’ work became the first medical manuscript to be printed (1478), even preceding the writings of Hippocrates and Galen. In Book 4, Chapter 10, we find his classic description of inflammation: notae vero inflammationes sunt quattuor, rubor, et tumor, cum calore et dolore.
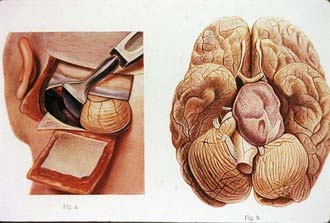
Celsus made a number of interesting early observations related to neurosurgery. Book VIII, Chapter 4 contains one of the earliest descriptions of an epidural hematoma resulting from a ruptured middle meningeal artery.25 In head-injured patients, Celsus recommended that the surgeon always operate on the side of greater pain. The trephine should always be placed at the point where the pain is best localized. Celsus described a technique for a craniotomy that involved drilling a number of holes and then connecting them with a hammer and chisel. The chisel had a protective blade that separated the dura from the bone and prevented injury to it during the surgical dissection. However, he regarded the operation of trephination as the ultimum refugium, to be used only when all conservative measures had been exhausted.
Galen of Pergamum (129-200 AD)
Galen of Pergamum, whose name comes from “galenos,” meaning calm or peaceful, is remembered as a powerful personality, an original investigator, and a leading proponent of the doctrines of the Hippocratic and Alexandrian schools (Fig. 1-5). Galen began his writing career at the age of 13 and continued to add to the literature until his death at the age of 70. In the end, his writings remained the most extensive in size, scope, and influence in early antiquity. Galen’s prodigious output accounts for  of all the surviving medical writings of antiquity (Fig. 1-6).27
of all the surviving medical writings of antiquity (Fig. 1-6).27
FIGURE 1-6 Title page from the collected works of Galen.
(From Galen of Pergamum. Omnia Quae Extant Opera in Latinum Sermonem Conversa (Quinta ed). Venice: Apud Juntas; 1576-1577.)
Galen’s life and activity fortunately occurred during the reigns of two of the greatest Roman emperors, Antonius Pius (86-161 AD) and Marcus Aurelius (121-180 AD). Galen became the physician to the gladiators of Pergamum and as a result saw and treated many traumatic injuries. From both his surgical experiences and anatomic studies, he made contributions to the fields of neurology, neurosurgery, and neuroanatomy. In his writings Galen differentiated between the pia mater and the dura mater and gave one of the earliest accurate descriptions of the corpus callosum, the ventricular system, the pineal and pituitary glands, the infundibulum, and what we now call the aqueduct of Sylvius. Nearly 1600 years before the Scottish anatomist Alexander Monro (Secundus) (1733-1817), Galen described the structure now called the foramen of Monro. He performed a number of anatomic experiments, including early studies on the effects of transection of the spinal cord.28,29 From these studies Galen was able to describe the specific loss of function below the level of transection. In a now classic experiment he sectioned the recurrent laryngeal nerve in the dog and found that hoarseness occurred (discussed further in Chapter 7, see also De Usu Partium, Book VII, Chapter 11 ,Chapter 12, Chapter 13, Chapter 14, Chapter 15, Chapter 16, Chapter 17, Chapter 18).28 Galen was the first to provide an early classification of the cranial nerves. In his original classification he described 11 of the 12 cranial nerves; however, by combining several, he arrived at a total of only 7. In his descriptions he regarded the olfactory nerve as merely a prolongation of the brain and hence did not considered it a cranial nerve.28 Galen published a number of interesting views on higher cortical functions and embraced the concept that the brain was responsible for intelligence, fantasy, memory, and judgment. These views were original and represented an important departure from the cardiocentric teachings of the earlier medical and philosophical schools such as Aristotle’s. Galen challenged Hippocrates’ view that that the brain was only a gland and instead attributed to the brain the powers of voluntary action and sensation (encephalocentric), this last being a remarkable advance in thinking for the period.
From a series of anatomic studies, Galen provided some of the earliest observations on cervical spine injury and the resulting disturbance in arm function. Further study of spinal cord injury led to his elegant description of what we now call “Brown-Séquard” syndrome (i.e., hemiplegia with contralateral sensory loss in a hemisection of the spinal cord).29 Galen provided one of the earliest clinical descriptions of hydrocephalus and clearly recognized its poor prognosis. Using his extensive experience with head injuries, he provided innovative arguments for elevation of depressed skull fractures, fractures with hematomas, and comminuted fractures. Galen was more aggressive in his treatment by recommending the removal of bone fragments, particularly those pressing into the brain. In describing surgical techniques, he detailed a safer and more reliable use of the trephine and in particular argued for continuous irrigation during trephination to avoid delivering excessive heat and injury to the underlying brain. Galen, following or adapting earlier Hippocratic views, reiterated the concept the dura should never be violated by the trephine.
Paulus of Aegineta (Paul of Aegina, 625-690?)
Illustrated in Figure 1-7A, Paul of Aegina was a brilliant 7th century Byzantine Greek physician and surgeon who also trained in the Alexandrian school. He was an influential compiler of works in both the Latin and Greek schools; his writings, especially the Medical Compendium in Seven Books (Fig. 1-7B), was being consulted until well into the 17th century, with a translation in English appearing in the 19th century.30,31 His skill as a surgeon, described in Book VI, clearly details an unusual understanding of surgical principles. His skills became contemporary legend, which brought him patients from far and wide. Although Paul venerated the teachings of the ancients as tradition required, he introduced his own techniques with good results. His classic work The Seven Books of Paulus Aegineta contains an excellent section on head injury and use of the trephine.30,31 Paul of Aegina classified skull fractures into several categories: fissure, incision, expression, depression, arched fracture, and in infants, dent (what we now call a ping-pong fracture). In dealing with fractures he used an interesting skin incision: two incisions intersecting one another at right angles and forming the Greek letter χ, with one leg of the incision incorporating the scalp wound. For the comfort of the patient undergoing trephination, he stuffed the patient’s ear with wool so that the noise of the trephine would not cause undue distress (see Book VI, Section XC).31
The hydrocephalic affection occurs in infants, owing to their heads being improperly squeezed by midwives during parturition, or from some other obscure cause; or from the rupture of a vessel or vessels, and the extravasated blood being converted into an inert fluid [see Book VI, Section III, page 250].31
Islamic/Arabic Medicine—Prescholastic Period
One of the most beneficial teaching methods, and a quite modern one, did arise during the Islamic/Arabic period—the concept of bedside medical care and teaching. The paucity or lack of anatomic dissection, along with the prevalent view of the practice of surgery as an occupation done only by individuals of inferior status, reduced any preoccupation with surgical art. Another unfortunate surgical practice that occurred during this period was reintroduction of the Egyptian technique of using hot cautery for control of bleeding. Hot cautery was also used in lieu of the scalpel to create a surgical incision, the results of which often proved unfortunate for the surgical patient (Fig. 1-8).
We will review some of the writings of the significant scholars of this period, starting with those of Rhazes (Abu Bakr Muhammad Ibn Zakariya, 865-925). Rhazes was a scholarly physician, learned in diagnosis and exclusively loyal to Hippocratic teachings. Rhazes developed a considerable reputation that led him to becoming a court physician. He was not a surgeon, although he wrote on surgical topics.32 Rhazes was an early believer in the concept of “concussion” and advocated surgery for penetrating injuries of the skull in a period when surgical outcomes were almost always fatal. Rhazes believed that head injuries were among the most devastating of all injuries. In the case of skull fractures, which could be permanently damaging to the patient as a result of compression of the brain, his surgical advice would be that depressed fractures needed to be elevated.
Among the most influential physicians of this period was Avicenna (980-1037), physician and philosopher of Baghdad and known as the chief or “second doctor,” the first being Aristotle (Figs. 1-9 and 1-10). Avicenna’s writings and translations clearly extended the original Greek influence with a force so persuasive and durable that it remained the dominant scholarship until well into the 18th century. His greatest contribution is the detailed translation of Galen’s collected works, the Opera Omnia. Avicenna’s major work, Canon Medicinae, was an encyclopedic effort founded and clearly based on the writings of Galen and Hippocrates.33 The Greek word Canon refers to a straight rod, a carpenter rule, or standard of measurement. Accordingly, Avicenna’s work became the “rule,” the codification of Galen and Greek medicine. In reviewing the Canon, a number of interesting neurological discussions are found. Avicenna provides an early and accurate clinical understanding of epilepsy, for which his treatment consisted of administering various medicaments and herbals, with good results. It appears that Avicenna conducted anatomic studies, although he does not discuss this directly. He gives a correct anatomic commentary on the vermis of the cerebellum and the “tailed nucleus,” now known as the caudate nucleus. Recent reviews of Avicenna’s writings on the treatment of spine injuries and stabilization reveal remarkably modern views for this era.34–36
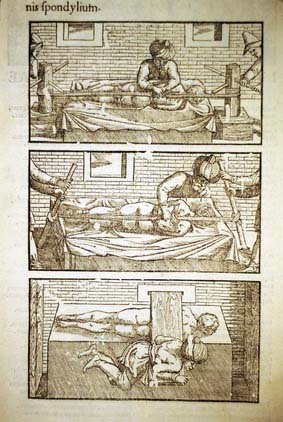
FIGURE 1-10 Title page of Avicenna’s Canon.
(From Avicenna. Liber canonis, de medicinis cordialibus, et cantica. Basel: Joannes Heruagios; 1556.)
Although Avicenna was clearly the “second doctor,” it was Albucasis (Abu Al-Qasim or Al-Zahrawi, 936-1013), a learned Islamic Moorish Spaniard, who was clearly the surgeon of the times (Fig. 1-11). In the Islamic tradition, Albucasis was both a great compiler and a serious scholar whose writings (some 30 volumes) were focused on surgery, dietetics, and materia medica. Albucasis’ insights into the importance of surgery are clearly revealed in his introduction to the Compendium.33 In the introduction he discusses the question why the Arabs had made so little progress in surgery. He attributed this lack of progress to a lack of anatomic study and inadequate knowledge of the classics. He clearly believed that anatomic studies were the key to learning and certainly key in performing surgical interventions. Although his thoughts on anatomic studies were excellent, Albucasis unfortunately popularized the frequent use of emetics as prophylaxis against disease, a form of barbaric medical treatment that survived in the form of “purging” until well into the 19th century. So influential were Albucasis’ surgical writings that they remained in use in the schools of Salerno and Montpellier for 500 years and had an enormous influence on medicine in the Middle Ages.
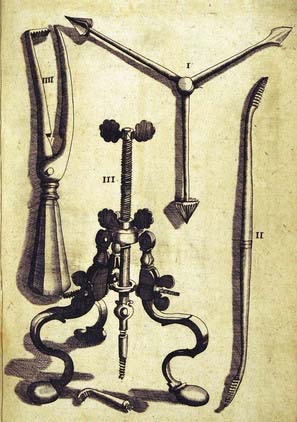
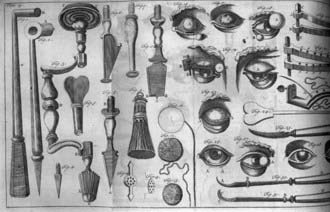
In the final section of the Compendium there is a lengthy summary of contemporary surgical practice.38–40 Also included in this part of Albucasis’ work is a unique collection of illustrations of surgical instruments. Their appearance here had lasting influence, with his style of instruments being used extensively in the schools of Salerno and Montpellier and later having important influence in the medieval period. Many of the instruments illustrated in the Compendium appear to have been designed by Albucasis. He clearly describes their design along with technical aspects of their use. Following on the earlier writings of the Greeks, he provides a novel design for a “nonsinking” trephine. The description of this instrument and others became classic and formed the template for many later instruments. An early and apparently unique technical innovation involved placing a collar on the trephine in a circular fashion, an ingenious design to prevent plunging into the brain. Some of the instruments were clearly copied from those described earlier by Paul of Aegina, but their practical use was further enhanced by their inclusion in the Compendium.
This is a fracture due to a fall or a blow from a stone and the like, making a dent in the surface of the bone and a hollow at the site as occurs in a bronze bowl when a blow falls on it and a portion of it is pushed in. This mostly occurs in heads who bones are soft, as those of children.38
The treatment of hydrocephalus was a vexing problem for surgeons and physicians because its outcome was almost always fatal. Albucasis recommended drainage of cerebrospinal fluid (CSF) in patients with hydrocephalus via a series of drains and wicks. He designed a lenticular-shaped surgical tool to make the puncture, which was performed over the anterior fontanelle. Having nicely detailed the technique, he blithely notes that the outcome is almost always fatal. What is interesting to note is that he attributed the poor outcomes not to the surgery but rather to “paralysis” of the brain from relaxation. Albucasis is clever in pointing out to the reader that one must pick the site for drainage carefully. Never cut over an artery because the potential hemorrhage can rapidly lead to death. In recent years, some authors have advocated treatment of hydrocephalus by “binding” the head with tight wraps. Albucasis was advocating this form of treatment more than a thousand years ago. For a child with hydrocephalus, he would “bind” the head with a wrap and then put the child on a “dry diet,” with limited fluid intake to dehydrate the child—in looking back, a rather progressive and reasonable treatment plan for this disorder.38,39
Middle Ages—The Age of Medieval Medical Scholasticism
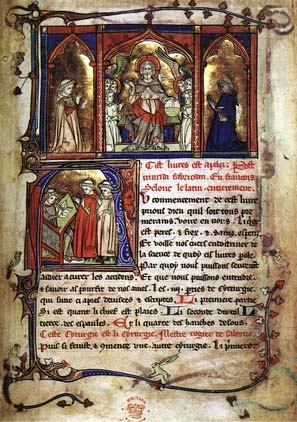
In the early Middle Ages, the influence of the Islamic/Arabic schools on medicine was beginning to lessen, along with a geographic switch in which intellectual centers for medicine were now returning to Europe. With the advent of medieval scholasticism, a new school of thought developed in which philosophical and metaphysical explanations and dialectic interpretations became prominent. One of the preeminent schools proposing this view was the School of Salerno in what is now Italy (Figs. 1-12 and 1-13).41 In much of Europe, despite the fact that barbarians were still in control, physicians were being trained and libraries were being built and expanded. At the School of Salerno, an early leader in developing medical scholasticism was Constantinus Africanus—magister orientis et occidentis (1020-1087).42 Constantine, a Magistri Salernitani, provided an important bridge in medicine by introducing the scholarship of Islamic/Arabic medicine there and eventually to all of Europe. Constantine received his medical education in Baghdad, where he learned the prevalent views of Islamic medicine. He moved to a monastery at Monte Cassino, where in the tradition of this period he translated Arabic manuscripts into Latin. Modern scholars believe that his translations included inaccuracies and introduced errors into the medical literature. Recent studies suggest that Constantine was a plagiarist and unreliable translator. Nonetheless, one cannot underestimate his contributions by providing the earliest transfer of Arabic/Islamic medical literature to Europe. In looking back, what we see are Greek texts originally translated into Arabic and now being translated into Latin, with the legacy of Galen and other early writers remaining firmly entrenched as dogma. Rather than providing or developing new ideas, the classical texts in medicine remained fully in control of medical dogma. One can only imagine how much medical and surgical knowledge was lost or distorted by inaccuracies in these successive translations. Constantine did make a key contribution to medieval medicine when he reintroduced anatomic dissection with an annual dissection of a pig, but the findings were compared with those recorded in the Greek classics. If the prosector’s findings did not match the ancient texts, they were simply ignored! Constantine was clearly a learned man, but his style of teaching became typical of the Medieval Ages; extensive compilations and translations were undertaken, but original thought or advances in knowledge were absent. In the Middle Ages the School of Salerno lead the way and was followed by the great medical schools at Naples, Bologna, Paris, and Montpellier, the early pillars of medieval medicine.
FIGURE 1-13 Title page from a collection of the works of Constantine the African—1536.
(From Constantinus Africanus. Constantini Africani Post Hippocratem et Galenum. Basel: Henricus Petrus; 1536.)
An unusual and remarkable book was produced during this period—Regimen Sanitatis Salernitum, a work that first appeared in the 12th century and was later republished in 140 different editions extending well into the 19th century.41 This book summarizes the Salernitan school directions for maintenance and care of patients in medicine. In Europe a strong educational system was being developed, but medicine remained cloaked in the literature of the classical Greeks and Islamic writing; for the most part, surgical education and surgical practice continued to be treated as an avocation limited to uneducated barber-surgeons and apprentices. However, there were talented surgeons who escaped the norm and produced original surgical works and practices.
Roger of Salerno (Ruggiero Frugardi, fl. 1170) is considered the first learned medieval European writer on surgery (Figs. 1-14 and 1-15). Roger was educated in the Salerno tradition and followed many of its teachings. His book on surgical practice, Practica Chirurgiae,43 offers techniques of interest to neurosurgeons. An example was his technique for checking for a tear of the dura and leakage of CSF in a patient with a skull fracture. To detect a leak, Roger would have the patient hold his breath and strain (i.e., Valsalva maneuver) and then look for air bubbles around the fracture site, a clear sign of a leak. He was a pioneer in the techniques of managing peripheral nerve injury. In a severed nerve, he argued for reanastomosis of the nerve ends with close attention paid to their alignment. In dealing with the large bleeding veins of the neck, he urged direct ligation with suture rather than cautery. Several chapters of his text are devoted to the treatment of skull fractures. Much of the technique described mirrors the views of earlier classical writers, but the style is clearer and more succinct. An example of this style is seen in this short description of the management of various skull fractures:
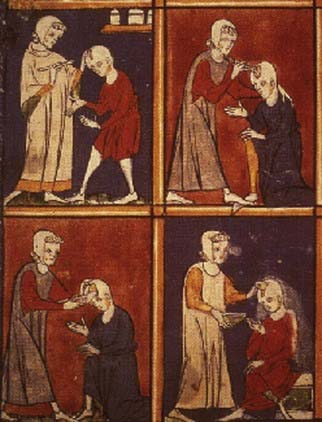
FIGURE 1-14 Roger of Salerno’s demonstration of brain and skull surgery.
(From the Sloane manuscript, 1977—Courtesy of the British Museum.)
When a fracture occurs it is accompanied by various wounds and contusions. If the contusion of the flesh is small but that of the bone great, the flesh should be divided by a cruciate incision down to the bone and everywhere elevated from the bone. Then a piece of light, old cloth is inserted for a day, and if there are fragments of the bone present, they are to be thoroughly removed. If the bone is unbroken on one side, it is left in place, and if necessary elevated with a flat sound (spatumile) and the bone is perforated by chipping with the spatumile so that clotted blood may be soaked up with a wad of wool and feathers. When it has consolidated, we apply lint and then, if it is necessary (but not until after the whole wound has become level with the skin), the patient may be bathed. After he leaves the bath, we apply a thin cooling plaster made of wormwood with rose water and egg.43,44
A 12th century manuscript owned by Harvey Cushing and attributed to Roger of Salerno has recently been translated. It contains an early description of a soporific for pain relief for use in surgery. Roger was particularly fond of citing the writings of Albucasis and Paul of Aegina. He strongly favored therapeutic plasters and salves but was not a strong advocate of the popular application of grease to injuries of the dura. He advocated the use of trephination for the treatment of epilepsy, although he is not clear why this technique would work. Chapters 1, Chapter 2, Chapter 3, Chapter 4, Chapter 5, Chapter 6, Chapter 7, Chapter 8, Chapter 9, Chapter 10, Chapter 11, Chapter 12, Chapter 13 (capita 1-13) detail contemporary surgical treatment of scalp wounds and fractures of the skull. One of his most significant errors in surgical practice was the concept that provoking suppuration of pus in a wound encouraged healing. This introduced the concept of “laudable pus” in wound healing and delayed good wound care until Lister and 19th century antisepsis.
For it is not necessary, as Roger and Roland have written, as many of their disciples teach, and as all modern surgeons profess, that pus should be generated in wounds. No error can be greater than this. Such a practice is indeed to hinder nature, to prolong the disease, and to prevent the conglutination and consolidation of the wound.45,46
Theodoric’s surgical work, which was first written in 1267, provides one of the best reviews of contemporary medieval surgery.45 He is also remembered as one of the earliest writers to include illustrations of his techniques. His recommendations called for meticulous (almost Halstedian) techniques with gentle handling of surgical tissues. Theodoric believed that aspiring surgeons should train only under competent masters. In the field of head injury, he argued that parts of the brain could be removed through a wound with little effect on the patient. In the treatment of skull fractures, he strongly argued for elevating depressed fractures. He advocated avoiding punctures of the dura because they could lead to abscess, convulsions, and bad outcomes. For pain relief during surgery, he developed his own “soporific sponge” that contained opium, mandragora, hemlock, and other less important ingredients applied to the nostrils, and once the patient fell asleep, he began surgery. Opium was probably the key ingredient.
William of Saliceto (Guglielo da Saliceto, 1210-1277) was a uniquely skilled Italian surgeon of the 13th century and a professor at the University of Bologna. His book on surgery, Chirurgia (or Cyrurgia), was completed in 1275, and in it we find highly original concepts that are not totally based on previous classical writings but in which the influence of Galen and Avicenna are clearly present.47 This book was written by William for his son Bernardino. The observations offered are based on his own surgical cases. Book IV contains the earliest known treatise on surgical and regional anatomy. His most significant contribution for this era was probably his decision to replace cautery with the surgical knife.
De anathomia in communi et de formis membrorum et figures que sunt considerande in incision et cauterizatione.47
Leonard of Bertapalia (1380?-1460) was a prominent 15th century Italian surgeon and writer. Leonard established an extensive and lucrative practice in the area of Padua and in neighboring Venice. At a time when anatomic dissection was rarely practiced in Europe, he became one of the earliest proponents of the study of anatomy. In 1429 he offered a course of surgery that included the dissection of an executed criminal. He devoted a third of his book to surgery on the nervous system and head injuries.48,49 He considered the brain the most precious of organs and regarded it as the source of voluntary and involuntary functions. In reviewing his treatment of skull fractures, he would always avoid materials that might generate pus. He argued for never placing a compressive dressing that might drive bone into the brain and proposed that if a piece of bone pierces the brain, the surgeon should remove it.
The first task to become a good surgeon should be to use his eyes.
Fourth, you must insure that your instruments be sharp and unrusted whenever you cut anywhere.
Seventh, you must never refuse anything brought you as a fee, for the sick will respect you more.
Eighth, you must never argue about fees with the sick, or indeed demand anything unless it be previously agreed upon, for avarice is the most ignoble of vices and should you be so inflicted, you will never achieve the reputation of a good doctor.49
Lanfranchi of Milan (d. 1306) was a pupil of William of Saliceto and often referred to as the father of French surgery. Lanfranchi advocated his teacher’s use of the knife in place of the burning cautery. Although born and educated in Italy, he had to leave Italy for France to avoid political strife. In his Cyrugia Parva we find a number of interesting surgical techniques. Lanfranchi perfected the use of suture for primary wound repairs.50 He was among the first to relate the direct effect of head injury to brain function. Hippocrates was the first to articulate the concept of commotio cerebri, but it is to Lanfranchi that we owe the first modern characterization of what is now called a cerebral concussion. For surgeons he developed a series of guidelines for trephination in skull fractures and “release of irritation” of the dura. Because of the dangers of skull surgery, Lanfranchi argued for using the trephine only when absolutely necessary; otherwise, he evoked the skills of the “Holy Ghost” to provide cure. Among his innovative surgical techniques was the development of esophageal intubation during surgery, a technique not commonly practiced until the 19th century. As an educated surgeon and a “Surgeon of the Long Robe” (i.e., academic), he attempted to elevate the art and science of surgery above the mediocre level of the menial barber-surgeon (“Surgeons of the Short Robe”). Lanfranchi also argued against the separation of surgery and medicine, advocated since the time of Avicenna, for he thought that a good surgeon should also be a good physician.
After Lanfranchi came another important figure in the history of French medicine and surgery—Henri de Mondeville (d. 1317). Educated in Paris and Montpellier, Henri later went on to become a professor at Montpellier. He was strongly motivated to elevate the profession of the surgeon and clearly detested the barber-surgeon: “Most of them were illiterates, debauchees, cheats, forgers, alchemists, courtesans, procuresses, etc.”46
In 1306 Henri undertook the task of developing a new treatise on surgery for the education of his students at Montpellier. Unfortunately, because of tuberculosis and ill health, the manuscript was never completed. Ironically, the edited portions were not published until 1892, when Professor Julius Pagel of Berlin completed the task.51 Henri adopted and followed a number of the views of Lanfranchi. He was a believer in clean wounds and avoiding “laudable pus.” Unfortunately, Henri would be the last surgeon in this era to argue for avoiding “laudable pus”; after him, surgeons returned to the older belief of pus developing in a wound being a good sign of healing. Henri offered originality in wound management by advocating for healing by primary intention—”modus novus noster.” In the surgical treatment of wounds, he encouraged the removal of foreign bodies and the use of wine dressings in wound care. Henri was clever in designing a number of surgical instruments. He is remembered for the design of a needle holder and also a forceps-type instrument for extraction of arrowheads. He argued against elevating skull fractures if there was no injury to the overlying soft tissues. He believed that nature would do a better job at healing the fracture by natural union. It was his opinion that unnecessary exploration and probing of the wound would only cause more injury than natural healing—in retrospect a rather brilliant insight into wound care (Fig. 1-16).46
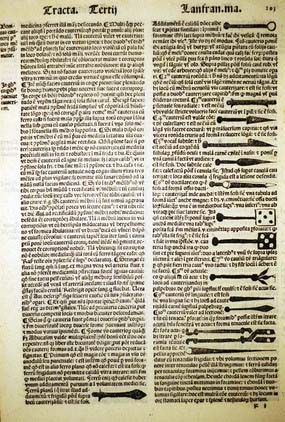
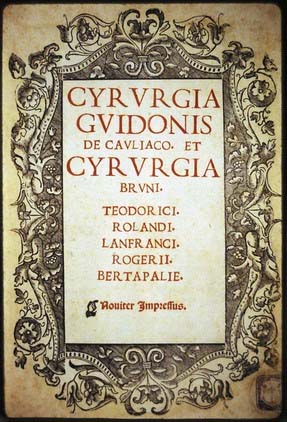
FIGURE 1-16 Surgical instruments designed by Lanfranchi are illustrated here in this early 1519 book.
(From Lanfranchi of Milan. Chirurgia. In: Guy de Chauliac Cyrurgia et Cyrurgia Bruni, Teodorici, Rolandi, Lanfranci, Rogerii, Bertapalie. Venice: Bernardinus Venetus de Vitalibus; 1519.)
No history of surgery can be complete without a discussion of the contributions of Guy de Chauliac (1300-1368) (Fig. 1-17).52 This surgeon was clearly the most influential European surgeon of the 14th and 15th centuries. He was so highly respected that he became the physician for three popes at Avignon (Pope Clement VI, Innocent VI, and Urban V) and leading surgeon and educator at the school of Montpellier. Guy was educated at Toulouse, Paris, Montpellier, and Bologna. He was an early proponent of anatomic dissection of a human cadaver. He states: “In these two ways we must teach anatomy on the bodies of men, apes, swine, and divers other animals, and not from pictures, as did Henri de Mondeville who had 13 pictures for demonstration of anatomy.”53 His writings were popular and continued to exert an influence on surgery until well into the 17th century. His principal didactic surgical text was scribed in 1363 and titled the Collectorium Cyrurgie.53 There are 34 known manuscripts of this work, with the first printed edition appearing in 1478, and more than 70 editions followed. In promoting surgeons as more skilled individuals (versus “mechanics,” i.e., barber-surgeons), he stated four conditions that must be satisfied for a practitioner to be a good surgeon: (1) the surgeon should be learned; (2) he should be an expert; (3) he must be ingenious; and (4) he should be able to adapt himself (from the introduction of Ars Chirurgica). For the modern neurosurgeon, Guy provides an interesting discussion of techniques that he devised for the treatment of head injuries. Before beginning surgery the head needs to be shaved. Shaving of the hair will prevent hair from getting into the wound and interfering with primary healing. For depressed skull fractures, Guy preferred to put wine-soaked cloths into the injured site to assist healing. He categorized head injuries into seven types and discussed the management of each in detail. Scalp wounds required only cleaning and débridement, whereas a compound depressed skull fracture must be treated by means of trephination and elevation. Skin closure was done by primary repair and for which he claimed good results. To help control excessive bleeding and provide hemostasis, he used egg albumin.
As England was moving away from the barbarian invasions and into the Middle Ages, university education in England began to become comparable to the European model. The leading surgeon of this period in England was John of Arderne (Arden, 1307-1380), who trained as a military surgeon and saw much war experience. In 1370 he came to London and joined the Guild of Military Surgeons. He adopted the phase “chirurgus inter medicos,” or a surgeon among physicians. His manuscript on surgery was written about 1412.54 This manuscript, De Arte Phisicali et de Cirurgia, was translated into English by D’Arcy Power in 1922, a valuable addition to the English literature on early surgery.55 His writings suggest that he was a skilled surgeon and had a number of practical insights into what could or could not be done surgically. He was a firm believer in clean hands and well-shaped nails for surgery, although some writers have thought that this was more for social reasons than for surgery.56 In addition, he would bathe his open wounds with an irrigation fluid that contained turpentine, a useful surgical antiseptic for keeping wounds clean. Most importantly, John of Arderne was a firm believer in education and learning. The surgeon must also “always be sober during any surgery as drunkenness destroys all virtue and brings it to naught.”46
Origins of Neurosurgical Practice in the Renaissance
Any discussion of Renaissance surgery and anatomy has to begin with Leonardo da Vinci (1452-1519), the quintessential Renaissance man (Figs. 1-18 to 1-20). Multitalented and recognized as an artist, an anatomist, and a scientist, Leonardo went to the dissection table to better understand surface anatomy and its relationships to art and sculpture. From his studies Leonardo is now recognized as the founder of iconographic and physiologic anatomy.57–59 For the neurosurgeon, Leonardo provided the earliest, albeit crude, diagrams of the cranial nerves, the optic chiasm, and the brachial and lumbar plexuses. He developed a wax-casting technique that allowed him to understand the anatomy of the ventricular system. To do this he took a fresh brain and poured liquid wax into the ventricles; a hollow tube was inserted to allow egress of the air. Leonardo’s experimental studies included sectioning a digital nerve and noting that the affected finger no longer had sensation, even when placed in a fire. Leonardo was not a surgeon, but he gave an important impetus to the study of anatomy and defining correct anatomic relationships—vital concepts for any surgeon. Unfortunately, Leonardo’s great opus on anatomy, which was to be published in some 120 volumes, never appeared.60 His anatomic manuscripts circulated among the artists in Italy throughout the 16th century, only to be lost and then discovered in the 18th century by William Hunter. These anatomic works had a profound influence on artists and physicians and subsequently on the development of modern anatomic studies. Leonardo, as a founder of modern anatomy, provided a creative spark to re-explore the human body by hands-on dissection.

FIGURE 1-18 Leonardo Da Vinci drawing showing the “cell doctrine.”
(Courtesy of Windsor Castle Collection, Edinburgh, Scotland—Her Majesty the Queen of England.)
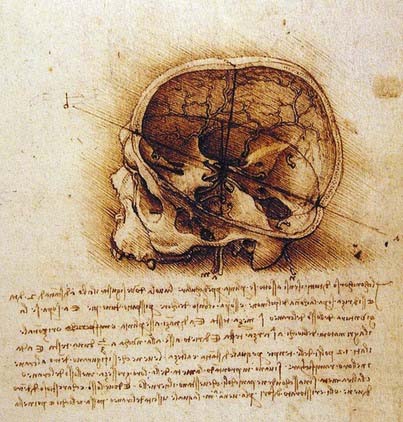
FIGURE 1-19 Leonardo Da Vinci’s “three-dimensional” drawing of the anatomy of the skull.
(Courtesy of Windsor Castle Collection, Edinburgh, Scotland—Her Majesty the Queen of England.)
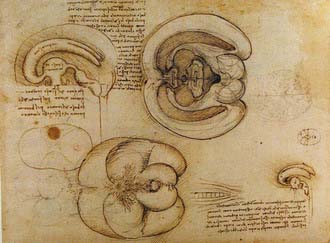
FIGURE 1-20 Leonardo Da Vinci’s “wax casting” modeling of the ventricular system.
(Courtesy of Windsor Castle Collection, Edinburgh, Scotland—Her Majesty the Queen of England.)
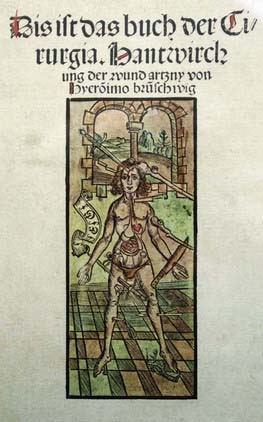
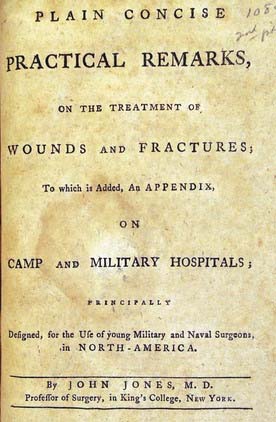
The earliest printed surgical work that contained illustrations was authored by Hieronymus Brunschwig (ca. 1450-1512) in Buch der Cirurgia and published in Strasbourg in 1497 (Fig. 1-21).61 Although the images have nothing to do with specific surgical procedures, the book is the first to discuss the management of gunshot wounds; gunpowder had recently been introduced for the weapons of war. This work was considered to be valuable enough to be plagiarized and published in a pirated edition the same year and appeared in many other editions throughout the 16th century. In the 1513 edition, the first illustration of a patient with a head injury undergoing treatment was added to the work.
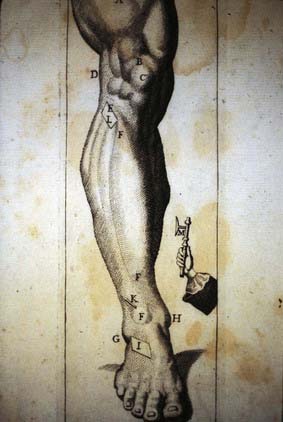
An early Renaissance surgeon who incorporated some of the recently revealed anatomic concepts in his publication was Hans von Gersdorff (1455-1529). In his surgical book Feldtbuch der Wundartzney, published in 1517, are some of the earliest illustrations on surgical technique (Fig. 1-22).62 Gersdorff was a military surgeon and, with more than 40 years of war experience, became adept at handling battlefield injuries. This handbook for surgeons was divided into four parts: anatomy, surgery, leprosy, and a glossary of anatomic terms, diseases, and medications. The section on anatomy was based on his own extensive experience, as well as the earlier Islamic writings and the works of Guy de Chauliac. The surgical portion deals with military surgery, mostly on how to extract foreign objects, tourniquet techniques to control bleeding, and amputation techniques. For the neurosurgeon, there are several woodcuts dealing with surgical technique and surgical instrumentation. In one illustration, a third nerve palsy on the side of a depressed skull fracture and a facial paralysis on the opposite side are clearly demonstrated. Included in this work is also the first plate showing dissection of the human brain. This surgical work became very popular and, because of its practical presentation of surgery and the illustrations in the text, went through several editions.
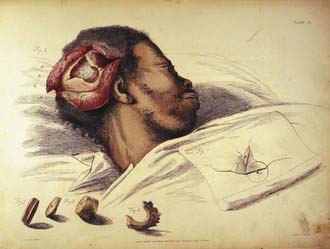
One of the greatest figures in the history of surgery remains Ambroise Paré (1510-1590), a poorly educated humble Huguenot and an individual whom today many historians consider the father of modern surgery (Figs. 1-23 and 1-24). After an extensive military surgical experience, Paré organized and published a substantial body of practical knowledge along with innovative instrument designs. At this time most physicians and surgeons published their writings in Latin. Nevertheless, Paré preferred to publish in the vernacular (i.e., French) rather than in Latin.63–66 By this transition Paré’s books gained wider dissemination and appreciation. As his reputation grew, he became a valued surgeon to the European royal courts. One of Paré’s most famous cases was a head injury sustained by Henri II of France. Paré attended the King and was also present at the autopsy. Henri II suffered a subdural hematoma after a joust during the marriage celebration of Elizabeth of France to Philip, King of Spain. When Paré described the clinical findings of Henri II, he noted that the patient complained of a headache and blurred vision, with vomiting, lethargy, and signs of decreased respiration eventually developing. Paré postulated that the injury was due to a tear in one of the bridging cortical veins, and he was clearly describing signs of increased intracranial pressure. His remarkable clinical observations and clinical history were confirmed at autopsy. Thus, despite humble beginnings, Paré became one of the giants in this formative period of surgery.
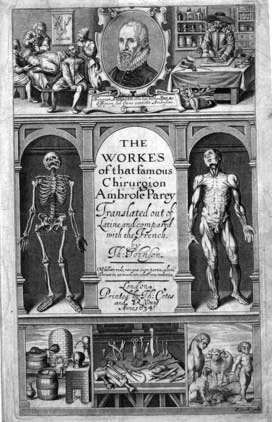
FIGURE 1-23 Title page of Ambroise Paré’s collected works on surgery published in English.
(From Paré A, Johnson T, trans. The Workes of That Famous Chirurgion Ambroise Parey. London: Richard Coates; 1649.)
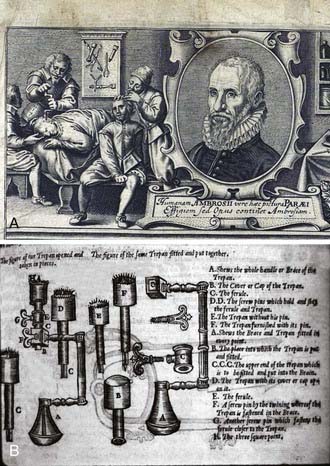
FIGURE 1-24 A, Trephination plate from Paré’s surgical works. B, Neurosurgical tools from Paré’s surgical works.
(From Paré A, Johnson T, trans. The Workes of That Famous Chirurgion Ambroise Parey. London: Richard Coates; 1649.)
Among Paré’s surgical works, his writings on the brain remain the most remarkable.64,65 Book X is devoted to the diagnosis and management of skull fractures. Although not original to Paré, he popularized the technique of elevating a depressed skull fracture with a Valsalva maneuver:
For a breath driven forth of the chest and prohibited passage forth, swells and lifts the substance of the brain and meninges where upon the frothing humidity and sanies sweat forth.64
By doing this, both blood and pus can be expelled from the fracture site. Paré’s surgical techniques demonstrated unusual and unique advances over previous writers. He provides extensive discussion on the use of trepans, shavers, and scrapers. He was skilled at removing osteomyelitic bone, incising the dura, and evacuating blood clots and pus, procedures that surgeons had previously done only with trepidation. He advocated débridement of wounds for good healing and emphasized that foreign bodies must be removed from the injury site. Paré’s most significant change in contemporary surgical practice was the serendipitous discovery that boiling oil, a then common surgical practice, should not be used in gunshot wounds. Substituting a dressing of egg yolk, rose oil, and turpentine provided improved wound healing and led to a dramatic reduction in morbidity and mortality. Paré also discarded the older Islamic technique of hot cautery for control of bleeding, instead substituting the use of ligatures and thereby reaping the benefits of enhanced healing and reduced blood loss.65 The improvement in his results was a source of wonder to Paré and gave rise to his famous aphorism:
Among the Renaissance giants of anatomy and surgery there arose the great Italian surgeon and anatomist Berengario da Carpi (1470-1550). In 1518, Berengario da Carpi wrote the second monograph devoted solely to treating injuries of the head, the first being by Hippocrates (Figs. 1-25 to 1-27).67,68 This book was motivated by Berengario’s successful treatment of a serious head injury in Lorenzo dé Medici, Duke of Urbino. In a dream shortly after he had treated Lorenzo, Berengario was visited by a man wearing a cap adorned with a rooster feather and golden-winged sandals (i.e., Hermes Trismegistus, or the Third Mercury). This individual encouraged Berengario to a write a treatise on skull fractures and head injuries. As a result of this dreamy intervention a marvelous tractatus appeared, the first printed work devoted solely to head injuries. In this text we find discussions of original surgical techniques along with the earliest illustrations of cranial instruments designed for the surgical treatment of head injuries. As an anatomist, Berengario, like Leonardo da Vinci, provided one of the earliest and most complete discussions of the ventricular system. Berengario presented some of the earliest descriptions of the pineal gland, choroid plexus, and lateral ventricles.67 His anatomic illustrations are among the first published from actual anatomic dissections. Berengario was a believer in anatomic dissection because that was the only way one could learn the anatomy; he believed that using only the written word was useless and added that the earlier writings were full of anatomic errors. His anatomic writings were among the first to challenge the medieval writings of Galen and others.
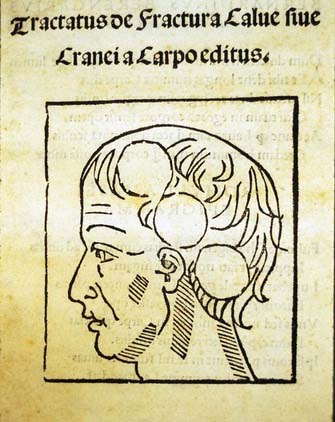
FIGURE 1-25 Title page from Berengario’s treatise on head injury—1518.
(From Berengario da Carpi J. Tractatus de Fractura Calvae Sive Cranei. Bologna: Hieronymus de Benedictus; 1518.)
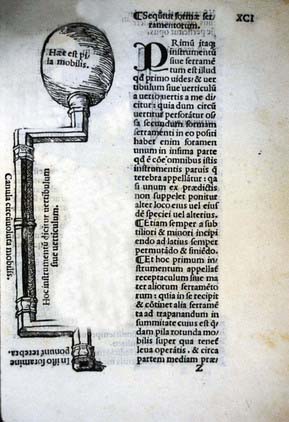
FIGURE 1-26 Neurosurgical trephine (hand brace) designed by Berengario.
(From Berengario da Carpi J. Tractatus de Fractura Calvae Sive Cranei. Bologna: Hieronymus de Benedictus; 1518.)
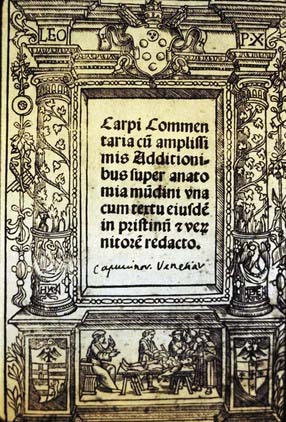
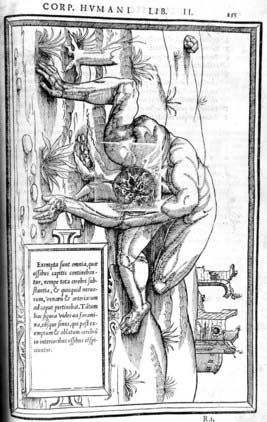
FIGURE 1-27 Title page with allegorical anatomic dissection scene from Berengario’s work on anatomy—Isagogae, 1522.
(From Berengario da Carpi J. Isagogae Breves perlucide ac ubertine in Anatomiam Humani Corporis. Bononiae, Italy: B. Hectoris; 1522.)
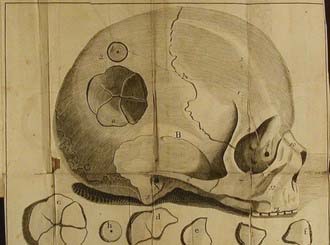
A not so well-known writer and anatomist of the Renaissance was a Marburg professor by the name of Johannes Dryander (Johann Eichmann, 1500-1560). In 1536 (expanded version in 1537) Dryander published an illustrated work on the brain and skull (Figs. 1-28 and 1-29).69,70 Within this remarkable work are 16 plates of the brain showing successive layered dissections of the scalp, dural coverings, and brain. The drawings on the anatomy of the cerebellum and the posterior fossa are particularly striking. There are inaccuracies in the text because of the prevailing influence of Galen and medieval scholasticism, but this book can be considered the first textbook of neuroanatomy. Despite Dryander’s allegiance to Galen and his teaching, he advocated public anatomic dissections, the results of which led to these remarkable neuroanatomic drawings.
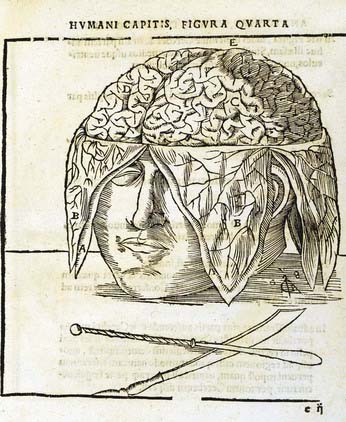
FIGURE 1-28 Scalp and skull dissection illustrations from Dryander—1537.
(From Dryander J. Anatomiae. Marburg: Eucharius Ceruicornus; 1537.)
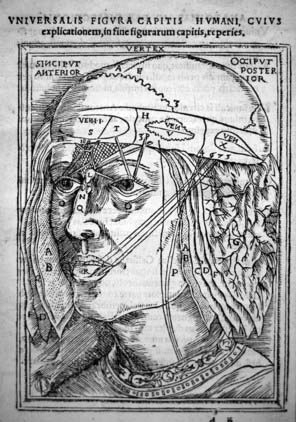
FIGURE 1-29 “Cell doctrine” theory illustrated here within the ventricular system as illustrated by Dryander—1537.
(From Dryander J. Anatomiae. Marburg: Eucharius Ceruicornus; 1537.)
Military surgery has always been a great educator of surgeons, and one of those particularly influenced by his military service was Volcher Coiter (1534-1576). Coiter was an army surgeon and city physician in Nuremberg who had the good fortune to study under several contemporary giants, including Fallopius, Eustachius, and Aldrovandi. From their teachings and education, Coiter was able to undertake unique and original anatomic and physiologic investigations.71 Among his anatomic descriptions are the first anatomically correct details of the anterior and posterior spinal roots. He was the first to distinguished gray from white matter in the spinal cord. Coiter had a particularly strong interest in the spine, which led him to conduct a number of anatomic and pathologic studies of the spinal cord, including an early model of decerebrate posturing. Coiter also provided a number of details on how to trephine the skulls of birds, lambs, goats, and dogs.71 He was the first to associate the pulsation of the brain with the arterial pulse. As an early neurosurgeon and investigator, he reported on opening the brain and removing parts of it with no ill effects noted—an early, surprising precursor of cerebral localization.
One of the most skilled of Renaissance surgeons was a Venetian by the name Andreae della Croce (1509?-1580). Croce was a follower and believer in Paré and used many of his techniques (Figs. 1-30 and 1-31). A combination of surgical skill and a Renaissance flair for design led Croce to produce a remarkable book on surgery in 1573.72 Within this monograph are some of the most beautifully engraved scenes of neurosurgical operations. As was typical of the period, surgical operations were performed in family homes, usually in the bedroom with the occasional dog lying at the foot of the bed. Croce textually and in drawings describes techniques for performing trephinations. Several illustrations show the various types of arrows, spears, and bullets used in warfare, and techniques for their removal are detailed. A series of plates are added showing his instrument designs for performing neurosurgical procedures. A concept difficult to comprehend for the modern reader is bloody trephination being performed with minimal anesthesia in a beautifully appointed noble’s bedroom.
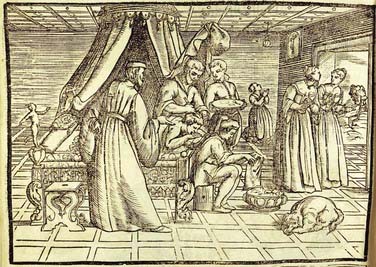
FIGURE 1-30 An elegant trephination scene being performed in a noble’s bed chambers—from Croce.
(From della Croce GA. Chirurgiae Libri Septem. Venice: Jordanus Zilettus; 1573.)
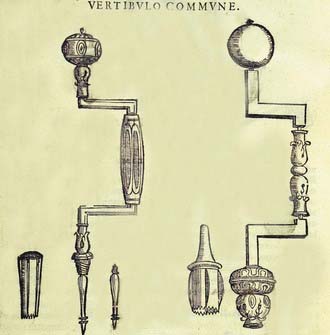
FIGURE 1-31 Neurosurgical instruments designed and illustrated by Croce.
(From della Croce GA. Chirurgiae Libri Septem. Venice: Jordanus Zilettus; 1573.)
A figure in surgery and anatomy that typified the great strides of learning in the Renaissance was Andreas Vesalius (1514-1564). Vesalius was educated at Louvain, Montpellier, and Paris, all staunch schools of Galenic orthodox teaching (Figs. 1-32 and 1-33). Rejecting the views of his Galenic-enthralled professors, Vesalius provided an innovative and dramatic approach to anatomic dissection. Following on the theme of earlier 16th century anatomists such as Leonardo da Vinci and Berengario da Carpi, Vesalius argued that anatomic dissections had to be done by the teacher, not by an ignorant prosector being guided by the professor who sat at the lectern reading from a Galenic monograph on anatomy.
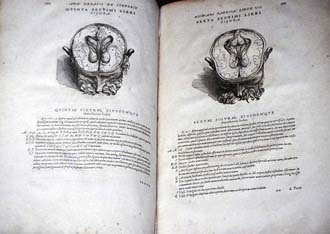
FIGURE 1-33 Two anatomic views of the cross-sectional anatomy of the brain as illustrated by Vesalius in 1543.
(From Vesalius A. De Humani Corporis Fabrica Libri Septem. Basel: Joannes Oporinus; 1543.)
Vesalius was appointed professor of anatomy at Padua at the young age of 23. At the age of 28, in 1543, he produced his great magnum opus, De Humani Corporis Fabrica.73 In Book VII is an extensive discussion on the anatomy of the brain. Included in the chapter are detailed anatomic discussions with excellent illustrations. Following his anatomic caveats, Vesalius noted that the “heads of beheaded men are the most suitable [for study] since they can be obtained immediately after execution with the friendly help of judges and prefects.”74
Vesalius was also trained as a surgeon. In the Fabrica is a section of text on the brain and the dural coverings in which Vesalius discusses mechanisms of brain injury and how the various membranes and bone have been designed to protect the brain. Vesalius, in the second edition of his major work, also provided an early case of a child with hydrocephalus and remarked on the pathology as originating from CSF but was unable to offer surgical treatment: “in ipsius cerebri cavitate, adeoque in dextro sinistroque illius ventriculis: quorum cavitas amplitudoque ita increverat, ipsumque cerebrum ita extensum fuerat, ut novem fere aquae libras continuerint.”75 A close examination of several of the illustrated initial letters in the text shows little cherubs performing trephinations!
A contemporary of Vesalius and another leader in Renaissance anatomic studies was a Paris anatomist—Charles Estienne (1504-1564). In 1546, a book with striking neuroanatomic plates appeared in a work on anatomy by Charles Estienne (Figs. 1-34 and 1-35).76 This book had been completed in 1539, thereby predating Vesalius’ work by 4 years, but legal problems delayed its publication until 1546. The book is notable for its wealth of beautiful anatomic plates dealing with neuroanatomy. This work contains representations of a series of anatomic figures with the subjects posed against sumptuous and imaginative Renaissance backgrounds. However, in reviewing the text the anatomic details are not as original as Vesalius’. In addition, in the text many of the errors of Galen and his followers are repeated. Regardless, the plates on the nervous system are graphic and among the most illustrative of this period. An important work, albeit with errors, it details the anatomy of the skull and brain more accurately than in previous works.
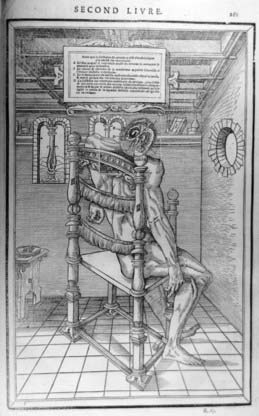
FIGURE 1-34 Estienne’s anatomy of the brain.
(From Estienne C. De Dissectione Partium Corporis Humani Libri Tres. Paris: Simon Colinaeus; 1546.)
Surgeons of the Insurgency—17th Century
A distinctive figure of this period is Thomas Willis (1621-1675), an early describer of the eponymous “circle of Willis” familiar to every physician (Figs. 1-36 and 1-37). Willis was educated at Oxford and became a fashionable London physician. He published a number of important monographs, but the one that stands out is his Cerebri Anatomie published in London in 1664.77,78 With methodical attention to detail, this book became the most accurate anatomic study of the brain to date. Willis was assisted in this work by Richard Lower (1631-1691) in demonstrating that when parts of the “circle” were tied off, the anastomotic network still provided blood to the brain. The superb and anatomically accurate brain engravings were done by the prominent London personality Sir Christopher Wren (1632-1723).
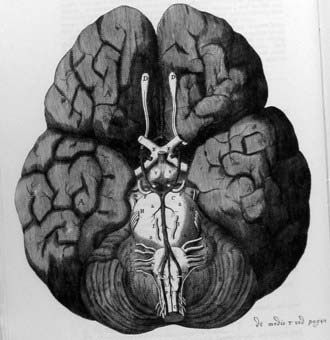
FIGURE 1-37 The “circle of Willis” as described by Willis and drawn by Sir Christopher Wren.
(From Willis T. Cerebri Anatome: Cui Accessit Nervorum Descriptio et Usus. London: J Flesher; 1664.)
To Willis we owe introduction of the concept of “neurology,” or the doctrine of neurons. Willis used the term in a purely anatomic sense inasmuch as the concept of “neurological” disease had not yet been introduced. Neurology as a noun did not enter general use until Samuel Johnson defined it in his dictionary of 1755.79 At this point neurology came to be understood as encompassing the entire field of anatomy, function, and physiology. The “circle of Willis” was not uniquely described by Willis; other anatomic descriptions of this circle were provided in other contemporary anatomic publications: Vesling,80 Casserius,81 Fallopius,82 and Humphrey Ridley.83
A prominent anatomist at this time and one often overlooked by contemporary writers is Humphry Ridley (1653-1708). Ridley was educated at Merton College, Oxford, England, and at the University of Leyden, where he received his doctorate in medicine in 1679. Ridley produced an important anatomic work on the brain, written in the English vernacular, a work that became widely circulated and influential (Figs. 1-38 and 1-39).
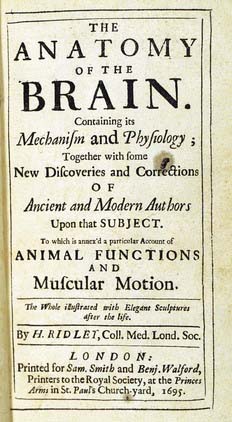
FIGURE 1-38 Illustrated here is the title page from Ridley’s work on brain anatomy.
(From Ridley H. The Anatomy of the Brain, Containing Its Mechanisms and Physiology: Together with Some New Discoveries and Corrections of Ancient and Modern Authors upon That Subject. London: Samuel Smith; 1695.)
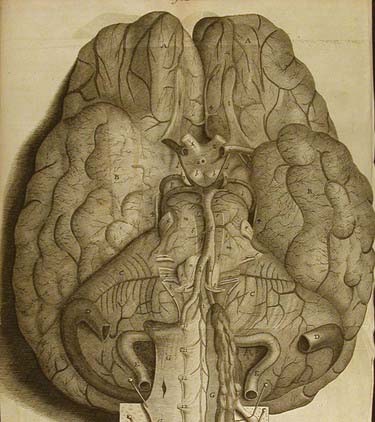
FIGURE 1-39 Ridley’s illustration of the anastomotic network at the base of the brain—the “circle of Willis.”
(From Ridley H. The Anatomy of the Brain, Containing Its Mechanisms and Physiology: Together with Some New Discoveries and Corrections of Ancient and Modern Authors upon That Subject. London: Samuel Smith; 1695.)
The Anatomy of the Brain. Containing Its Mechanism and Physiology; Together with Some New Discoveries and Corrections of Ancient and Modern Authors upon That Subject was published in London in 1695.83 As a personality, Ridley remains most elusive. At the time that his work on the brain appeared, many of the classical Greek views of the brain were in vogue. In reviewing 17th century anatomy and medicine we find a movement away from the earlier cell doctrine theory; anatomists were now recognizing the brain as a distinct anatomic entity. By rejecting the “cell doctrine” in which brain function was considered to reside within the ventricles, cerebral function now came to be viewed as a property of the brain.84,85
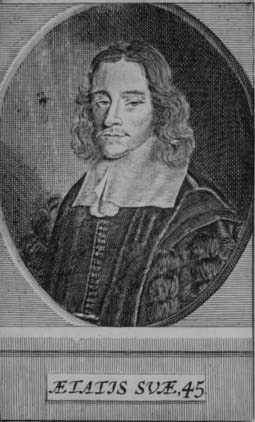
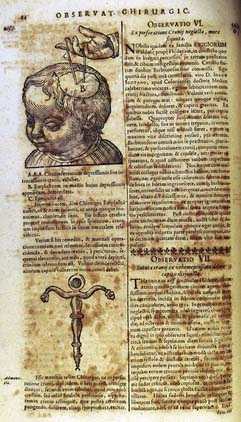
Fabricius produced one of the most important surgical works of the 17th century, titled Observationum et Curationum, a monograph that included more than 600 surgical cases, along with a number of important and original observations on the brain (Figs. 1-40 and 1-41).86 Fabricius’ observations on the brain and surgery included congenital malformations, skull fractures, and techniques for bullet extraction, along with original designs for field surgical instruments. He describes operations for intracranial hemorrhage (with cure of insanity), vertebral displacement, congenital hydrocephalus, and an occipital tumor of the newborn (probably an encephalocele). Fabricius carried out trephinations for the treatment of a brain abscess and cure of an old aphasia. He even removed a splinter of metal from the eye with a magnet, a cure that greatly enhanced his reputation.
FIGURE 1-40 Allegorical title page from Fabry’s collected works.
(From Fabry W. Observationum et Curationum Chirurgicarum Centuriae. Basle: Frankfurt, & Lyons, 1606-1641. A later collected works also contains a number of neurosurgical cases. Opera Observation et Curationum. Frankfurt: Joannis Beyerj; 1646.)
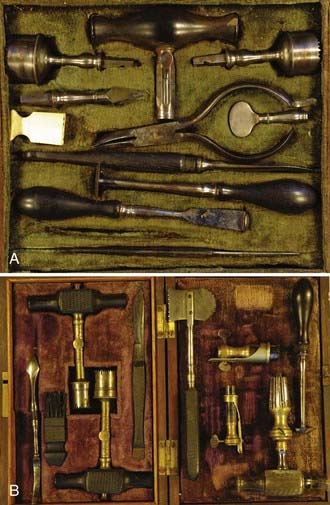
A monograph in which early and skillfully designed neurosurgical instruments appear is a work by Johann Schultes (Scultetus) of Ulm (1595-1645). With Armamentarium Chirurgicum XLIII, Scultetus, also known as Schultes, provides unique and graphic details of neurosurgical instruments, clearly the finest to appear since those published by Berengario in 1518 and Croce in 1573.37 The illustrations (Figs. 1-42 and 1-43) graphically reveal surgical techniques for treating fractures and dislocations, as well as a variety of bandaging techniques for wounds. The popularity of this surgical work led it to be translated into many languages, including English, and it had a considerable influence on surgery throughout Europe for more than 2 centuries. In reviewing the surgical plates and various operations we find exacting details described, including concepts from antiquity to the present. Interestingly, many of the instruments illustrated by Scultetus remain in use today. His details of surgical operations for injury to the skull and brain are remarkable plebiscite.
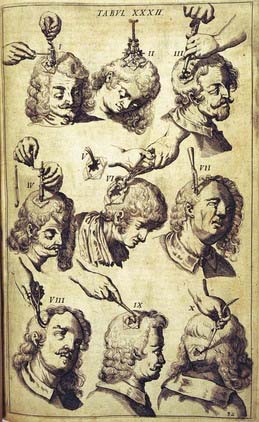
FIGURE 1-42 Surgical techniques designed by Scultetus for trephining the skull.
(From Scultetus J.  . Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.)
. Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.)
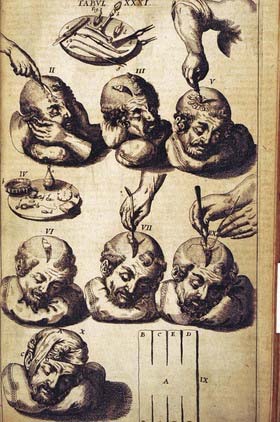
FIGURE 1-43 Scultetus’ techniques for dealing with skull fractures.
(From Scultetus J.  . Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.)
. Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.)
Neurosurgical practice continued to evolve in the 17th century. A surgeon who offered interesting technical advances on developing neurosurgical operating skills was John Woodall (ca. 1556?-1643). Woodall was a military surgeon by training and surgeon-general for the East India Company. For the surgeons of the East India Company he compiled a surgical monograph called the Surgeon’s Mate (1617).87 In his collected works, published in 1639, he provided a list of surgical instruments and sound advice for a surgical practice.88 He fabricated a trephine with the unique design of a crown that included a center pin, an innovation that prevented the crown from slipping on a bloody skull (Fig. 1-44). This trephine had a brace added that could be placed against the surgeon’s chest for additional support and driving force. This allowed the surgeon to drive the trephine with one hand while the other held the head, all of which could be accomplished on a rolling ship’s deck. Woodall, recognizing the ignorance of his contemporary German surgical colleagues, believed that a surgeon should practice trephining on sheep or calf skulls first before performing one on a human head. He comments:
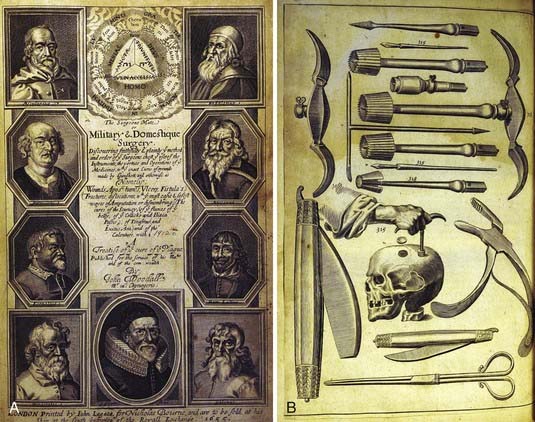
FIGURE 1-44 A, Title page from Woodall’s book on military and domestic surgery.87 B, Woodall designed a hand trephine with a series of interchangeable burs along with bone rongeurs. The trephine center pin, Woodall’s design, was especially useful on a rolling ship deck when applied to a bloody skull.
(From Woodall J. The Surgeons Mate. London: E. Griffin; 1617.)
The Germane Surgeons use no Trapan, that ever I could see my eight years living among them, though they both speak and write of it. But for as much as it is apparent, the work of a Trapan is very good, I therefore would advise a young Artist to make some experience first upon a calves head, or a sheep’s head, till he can well and easily take out a piece of the bone; so shall he the more safely do it to a man without error when occasion is [see page 4].88
An Englishman and Plymouth naval surgeon, James Yonge (1646-1721) was among the first to argue emphatically that “wounds of the brain are curable”; Galen had earlier announced, “I have seen the wounded brain heal.”27 Yonge’s first surgical text was a small monograph titled Wounds of the Brain Proved Curable.89 He provides a surgical account of a brain operation on a 4-year-old child with extensive compound fractures of the skull from which brain tissue issued forth. The surgery was successful and the child survived, which led Yonge to publish the account. Yonge also reported on more than 60 cases of brain wounds cured that he was able to locate in the older literature, beginning with Galen. The bibliography records the earlier cases that he was able to locate. He comments that this work was written in defense of surgery on the skull and the brain. From the preface,
I had the good fortune to be a successful chirurgeon to the child, whose case is contained in the following narrative: but I had scarcely wiped my instruments, and put up my plaister-box, before a physician of this town, sneakingly and maliciously endeavor to stifle [my] reputation insinuating that it was impossible to [cure brain wounds] because Wounds of the brain were absolutely mortal.89
Other technical innovations for treating head injuries also occurred in this period. Augustin Belloste (1654-1730) describes a technique for repairing “holes in the head” as a result of trauma or trephination with the use of lead plates. Keeping the brain from being exposed to “corrupt air” led to better outcomes in brain surgery.90
Eighteenth Century—An Enlightened Period for Neurosurgery
Judgment in distinguishing, and ability in treating diseases, are not to be attained by a transient cursory view of them; merely running round an Hospital for a few months, or reading a general system of surgery, will not form a compleat practitioner: the man, who aims at that character, must take notice of many little things, which the inattentive pass over, and which cannot be remarked by writers; he must accustom himself to see, and to think for himself; and must regard the rules laid down by authors, as the outlines only of a piece, which he is to fill up and finish: books may give general ideas, but practice, and medication, must make him adroit and discerning; without these, his reading may possibly keep him clear of very gross blunders, but he will still remain injudicious, and inexpert [from preface x-xi, Observations, London 1760].91
One of the giants in surgery was Percivall Pott (1714-1788), considered by many historians to be the greatest English surgeon of the 18th century. His list of contributions, several of which apply to neurosurgery, is enormous. His work Remarks on That Kind of Palsy of the Lower Limbs Found to Accompany a Curvature of the Spine (London, 1779) describes the disease entity now known as Pott’s disease (i.e., tuberculous caries of the spine).92 His clinical descriptions clearly describe the gibbus and tuberculous infection of the spine. Surprisingly, Pott failed to associate the relationship between the deformity and paralysis. An osteomyelitic infection of the scalp and skull in which pus collects under the pericranium is now called Pott’s puffy tumor. Pott argued that these lesions should be opened and drained (Figs. 1-45 and 1-46).
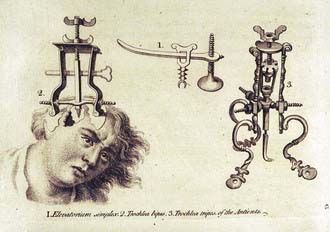
FIGURE 1-46 Trephination instrumentation as designed by Pott.
(From Pott P. Remarks on That Kind of Palsy of the Lower Limbs Found to Accompany a Curvature of the Spine. London: J. Johnson; 1779.)
Eighteenth century surgeons generated much discussion over the surgical practice of trephination. To trephine or not to trephine—Pott was a strong proponent of intervention. In his classic work on head injury (London, 1760), he clearly appreciated that the clinical findings of head injury were due to injury to the brain and not the skull.93 Pott studied head injuries and began to differentiate between “compression” and “concussion” injury of the brain. The following clinical description from his head injury book outlines some of his views:
In the mere fracture without depression of bone, or the appearance of such symptoms as indicate commotion, extravasation, or inflammation, it is used as a preventative, and therefore is a matter of choice, more than immediate necessity.93
The most significant development in 18th century writings on neurosurgical topics was the gradual recognition of the effects of trauma on brain function rather than just the skull. Several French surgeons drew a clear-cut distinction between the loss of consciousness accompanying a blow to the head and the drowsiness that appeared later. The former came to be recognized as a direct result of cerebral concussion, and the latter, after a lucid interval, came to be accepted as being due to a collection of blood producing compression of the brain. This idea was introduced by Jean Louis Petit (1674-1750), the leading surgeon in Paris in the first half of the 18th century, in a series of lectures that he gave in Paris.94 The realization that delayed loss of consciousness could serve as an indication for surgical intervention is one of the epochal events that mark the origins of neurosurgery as a discipline dealing with alterations in brain function and not just superficial injuries to the skull. It was a major conceptual change in an approach that had been followed for 2000 years and marks an important turning point in surgical thinking.
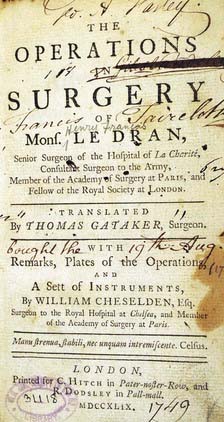
One of the earliest descriptions of the “lucid interval” in head injury was provided by Henri Francosi Le Dran (1685-1770). Le Dran was both an anatomist and surgeon who amassed a large surgical experience by serving as the chief surgeon to the French Army. Le Dran established a very popular school of anatomy in Paris that attracted students from all over Europe. Observations de Chirurgie 95 (Fig. 1-47) reveals a skilled surgeon with a wide variety of surgical talents. This work became Le Dran’s most popular surgical text and was reprinted several times and translated into English in 1749. It is a broad review of surgery, but most important to us are his views on surgery on the head. Le Dran details the concept of the “lucid interval” after a head injury and then attributes it most commonly to an epidural hematoma.
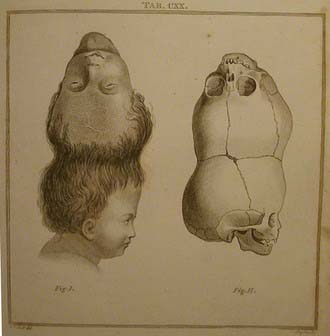
A remarkable and talented figure in English medicine and surgery and a student of Percivall Pott’s was John Hunter (1728-1793). Many writers consider Hunter equally as skilled as Pott, but his additional work in anatomy, pathology, physiology, and surgery led him to make a number of important contributions.96 Hunter, often referred to as the founder of experimental and surgical pathology, spent most of his career at St. George’s Hospital in London. He was trained in the apprentice style and had minimal formal education. He began his training under his older brother William Hunter and spent time with William Cheselden, talented mentors. As a surgeon, Hunter was an atypical figure for this time in that he approached the field of surgery in a more practical manner and at the same time added a bench side experimental touch. In A Treatise on the Blood, Inflammation, and Gun-Shot Wounds (London, 1794),97 Hunter drew on his years of military experience and wrote an important work on the management of gunshot wounds. He did not offer much on neurosurgery; the section on skull fractures occupied only one paragraph. In understanding vascular disorders, Hunter described the concept of collateral circulation. His circulation studies were conducted on a buck whose carotid artery was tied off to see the effect on the antler, but no ill effect was noted; the explanation was the development of collateral circulation, which he had now determined anatomically. Hunter later applied these concepts to the treatment of popliteal aneurysms, previously treated by amputation; he tied off the artery and realized that collateral circulation would develop. He was adroit at posing questions raised by his clinical experience, performing animal experiments to answer the questions, and integrating his clinical and scientific results into the best available treatment. He anatomically dissected a case of craniopagus parasiticus, a set of twins from India in which one child was fully formed and the other twin had only the head. The incomplete twin would show emotion and move the lip and mouth during eating (Fig. 1-48).98 Hunter is also remembered as a devoted student of anatomic curiosities and would go to great lengths, sometimes nefariously, to obtained specimens. The most famous case was an Irish giant whom Harvey Cushing later determined had acromegaly. The Irish giant knew of Hunter’s interest in him and went to great lengths to avoid his laboratory after death. However, the Irish giant became part of the Hunterian museum, which contained more than 13,000 specimens and is now part of the Royal College of Surgeons pathologic collection, a direct donation by Hunter.
Following Hunter was a pupil of his, John Abernethy (1764-1831), who was also a talented anatomist and surgeon. For American surgeons, Abernethy is remembered for publishing the first book in America devoted to a neurosurgical topic.99 So popular was Abernethy as a lecturer that the governors of St. Bartholomew’s Hospital built an anatomic theater for him, a place of training sought out by the brighter students of the period. Abernethy eventually went back to Scotland, his country of birth, and settled in Edinburgh to establish a general practice. He continued to develop a large apprenticeship program with students coming from far and wide. His contributions to neurosurgery included one of the earliest treatments of neuralgia of the arm; he performed a neurectomy in 1793 that provided instant relief to the patient.100 Later, the patient regained sensation in the hand, thus showing that there had been successful reunion of the nerve. Abernethy was an early advocate of ligating the common carotid artery for a cerebral hemorrhage. He later published his writings on the brain in an important work called Pathological and Practical Researches on Diseases of the Brain and Spinal Cord (1828).101 This work contains more than 150 cases of various neurological and neuropathologic conditions of the brain, spinal cord, and peripheral nerves (Figs. 1-49 and 1-50).
A contemporary of Abernethy was Benjamin Bell (1749-1806), among the most prominent and successful surgeons in 18th-century Edinburgh. Bell was a compassionate surgeon and among the first to emphasize the importance of reducing pain during surgery. Bell published a popular textbook of surgery, A System of Surgery.102 This book was widely read because of its clarity and precision. In reviewing his section on head injury, there is an important discussion on the differentiation of concussion, compression, and inflammation of the brain—each requiring different modes of treatment.103 Bell was a remarkably aggressive surgeon when it came to the brain; he stressed the importance of relieving compression (i.e., by trephination) of the brain whether it be caused by a depressed skull fracture or pressure from pus or blood. The concept of an epidural hematoma and its symptoms were appreciated by Bell; he argued for rapid and prompt evacuation.
Affections of the Brain from external violence, often induce a very complicated set of symptoms; are attended with imminent danger, and give much embarrassment to practitioners: Accordingly, both with respect to the hazard with which they are attended, and the difficulty that we meet with in the cure, there is perhaps no class of diseases to be compared with them. Wounds and bruises of the head, which at first exhibit no marks of danger, often induce a train of symptoms which elude the skill of the most experienced practitioner; and, without admitting of any mitigation, proceed to a fatal period, ending only the death of the patient [Volume 3, Chapter X, Section I].104
His discussion of the symptoms of brain compression from external violence is classic.
A great variety of symptoms indicating a compressed state of the brain [with] the most frequent, as well as the most remarkable, are the following: Giddiness; dimness of sight; stupefaction; lots of voluntary motion; vomiting; an apoplectic stertor in the breathing; convulsive tremors in different muscles; a dilated state of the pupils, even when the eyes are exposed to a clear light; paralysis of different parts, especially of the side of the body opposite to the injured part of the head; involuntary evacuation of the urine and faeces; an oppressed, and in many case an irregular pulse [Volume 3, Chapter X, Section III].105
In 1709 a small monograph by Daniel Turner (1667-1741) appeared.106 The book was titled A Remarkable Case in Surgery: Wherein an Account is Given of an Uncommon Fracture and Depression of the Skull, in a Child about Six Years Old; Accompanied with a Large Abscess or Aposteme upon the Brain. This monograph provides a contemporary view of an 18th century surgeon and the concerns of trephining the brain (Fig. 1-51).
An American surgeon who made an interesting contribution to neurosurgery was John Jones (1729-1791). In his monograph published in New York in 1775, this Revolutionary War surgeon provided the first American textbook on surgery (Fig. 1-52).107 Jones was educated in Europe; studied under Pott, Hunter, Monro, Petit, and Le Dran; and carried this education back to the United States. Jones was among the first faculty to form the first medical school in America, the University of Pennsylvania, Philadelphia. Jones was also one of the founders of New York Hospital. His monograph on surgery became the handbook of surgery for Revolutionary War surgeons. His views and techniques on trephination clearly reflect the views of his European teachers, especially Pott, Le Dran, and Petit.
One of the most popular surgical textbooks of this century was published by a German surgeon—Lorenz Heister (1683-1758) (Fig. 1-53). Heister was educated as both a surgeon and anatomist, a now common theme. He began his lectures in Latin, but because his students were so ignorant, he changed them to German. He went on to publish his first textbook in the vernacular German.108 So popular was the text that it was subsequently translated into a number of languages, including English, and circulated widely in Europe and England.109 The wide range of surgical knowledge that it communicated and its many practical surgical illustrations, bandaging techniques, and surgical techniques made it a well-used text. Heister would treat a head injury, but in accordance with earlier, more conservative views, he thought that trephination should be restricted to cases of fracture associated with depression. In wounds involving only concussion and contusion, he thought that trephination was too dangerous. When one realizes that Heister was practicing during the pre-Lister era, a period of very high risk for infection and injury to the brain, he might have been the more pragmatic surgeon.
XXVII. But when the Cranium is so depressed, whether in Adults or Infants, as to suffer a Fracture, or Division of its Parts, it must instantly be relieved: the Part depressed, which adheres, after cleaning the Wound, must be restored to its Place, what is separated must be removed, and the extravasated Blood be drawn off through the Aperture [he goes on to argue against the use of “sneezing”, i.e., the Valsalva maneuver, in elevating depressed fractures]—the ill Consequences that attend this Practice are so grievous, that in my Opinion it ought to be rejected [Book I, Chapter XIV, page 100].110
An early and successful treatment of a brain abscess was accomplished by François-Sauveur Morand (1697-1773). In Morand’s patient, a monk, otitis and subsequently mastoiditis developed and led to a temporal brain abscess.111 Morand trephined over the carious bone and discovered pus. He placed a catgut wick into the open surgical wound, but it continued to drain. He reopened the wound, opened the dura through a cruciate incision, and found a brain abscess. He explored the abscess with his finger, removed as much of the contents as he could, and then instilled balsam and turpentine into the cavity. He placed a silver tube for drainage, and as the wound healed, he slowly withdrew the tube. The abscess healed, the patient survived, and he reported this case as successful treatment of a brain abscess.
The Neapolitan physician Domenico Cotugno (1736-1822) published a small monograph of 100 pages, De Ischiade Nervosa Commentarius (Naples, 1764), in which are given the first descriptions of CSF and sciatica (Fig. 1-54).112 Cotugno performed a number of experiments on the bodies of 20 adults. Using a lumbar puncture technique, he was able to demonstrate the characteristics of CSF. In De Ischiade Nervosa Commentarius, he demonstrated the “nervous” origin of sciatica and differentiated it from arthritis, the common explanation prevalent at that time. He discovered the pathways of CSF and showed that it circulated in the pia-arachnoid interstices and flowed throughout the brain and spinal cord via the aqueducts and convexities. Cotugno also described hydrocephalus ex vacuo, the type of hydrocephalus seen with cerebral atrophy.
A popular and skilled French military surgeon, Louis Sebastian Saucerotte (1741-1814) (also listed as Nicolas) was at one time surgeon for the King of Poland and then a surgeon in various French Army units. As has often been the case in the history of neurological surgery, the occasion to deal with war injuries provided the most training and insight into the management of head injury. Saucerotte reintroduced the concept of the contrecoup injury, lost since antiquity. In his surgical textbook Mélanges de Chirurgie (Paris 1801),113 he describes in detail a series of intracranial injuries and their symptoms, including compression of the brain by blood clot. Saucerotte described a case of ataxia caused by a cerebellar lesion, including opisthotonos and rolling of the eyes. He divided the brain into “areas” of injury and pointed out that areas of severe injury are those at the base of the brain whereas injuries to the forebrain are the best tolerated. He also contributed one of the earliest clinical descriptions of acromegaly.
Nineteenth Century—Incunabula Period of Modern Neurosurgery
A medical and surgical giant in this period was Sir Charles Bell (1774-1842), a Scottish surgeon and anatomist. Bell was educated at the University of Edinburgh and spent most of his professional career in London. He is remembered for his many contributions to the neurosciences, including differentiation of the motor and sensory components of the spinal nerve root. Bell wrote a number of works on surgery, many of which were beautifully illustrated with his own drawings. These surgical drawings remain unrivaled in detail, accuracy, and beauty (Figs. 1-55 and 1-56).
If a drawing of all that we see in an operation, be an imperfect demonstration, so is the lesson of an operation performed on the dead body imperfect, for the circumstances most essential to know, cannot be presented there: so is the actual operation on the living body an imperfect demonstration, from the partial and rapid view which the spectator obtains. And, finally, as to description, words alone will never inform the young Surgeon of the things most necessary to a safe operation.114
Bell provided a skillful contemporary account of trephination as practiced in 1821:
Let the bed or couch on which the patient is lying be turned to the light—have the head shaved—put a wax-cloth on the pillow—let the pillow be firm, to support the patient’s head. Put tow [sic] or sponge by the side of the head—let there be a stout assistant to hold the patient’s head firmly, and let others put their hands on his arms and knees. The surgeon will expect the instruments to be handed to him in this succession—the scalpel; the rasparatory; the trephine; the brush, the quill, and probe, from time to time; the elevator, the forceps, the lenticular.115
Over the previous centuries surgeons tried various methods of reducing sensibility to pain but had minimal success. The use of mandrake, Cannabis, opium and other narcotics, the “soporific sponge” (saturated with opium), and alcohol had all been tried. In 1844, Horace Wells (1815-1848), a dentist in Hartford, Connecticut, introduced the use of nitrous oxide for dental procedures and for the first time had a good anesthetic result.116 Unfortunately, the death of one of his patients from what was probably an overdose of the anesthetic stopped him from investigating further. In Boston, another early investigator, W. T. G. Morton (1819-1868), also a dentist and early collaborator with Wells, persuaded a surgeon, Dr. J. C. Warren (1778-1856), to use ether to induce anesthesia. On October 16, 1846, Warren did so and produced a state of insensibility in a patient during which a vascular tumor of the submaxillary region was removed.117 In the United Kingdom, another surgeon, James Y. Simpson (1811-1870), was using chloroform, which had just been introduced in 1847 as an anesthetic agent.118 The contemporary literature was full of arguments on which was the best agent. Morton patented the ether technique and then approached the U.S. Congress to seek compensation for his discovery of ether and its use in surgery. The result of this advance was the first opportunity for a surgeon to operate on a patient without the need for heavy restraints or the necessity of operating at breakneck speed. Patients gained freedom from pain during the procedure, as well as now a lack of fear of surgery—developments whose importance cannot be overestimated in a surgical practice and in particular in the treatment of brain lesions.
One can easily appreciate the great trepidation with which the early surgeon approached either a skull or brain injury. Even with the best surgical technique, the surgeon would have the patient die postoperatively of suppuration and infection. Fevers, purulent material, brain abscesses, and draining wounds all led the best surgeons to suffer defeat. No surgeon could hope to invade or open the dura mater without inviting disaster until the risk for operative infection could be reduced. The first significant change came about when Lord Lister (1827-1912), using concepts developed by medical practitioners, introduced antisepsis into the operating room.119,120 In a different operating arena, Oliver Wendell Holmes (1809-1894) and I. G. Semmelweis (1818-1865) first showed that it was the contaminated hands of the obstetrician that spread puerperal fever, a devastating infection occurring in women during delivery.121,122 Holmes and Semmelweiss argued for hand washing between cases, a concept that was bitterly debated at the time. It is beneficial to examine the typical mid-19th century obstetrician. The obstetrician typically entered an operating room wearing with pride a black cloth coat soaked in old blood and the grime from earlier deliveries. The table on which the soon to be born baby was to be delivered was rarely cleaned, must less sterilized. These conditions led to the spread of multiple organisms on hands, instruments, and table surfaces, and many women died in childbirth of puerperal fever. The infection and contagion concepts developed by Louis Pasteur (1822-1895) and Robert Koch (1843-1910) and their introduction of antisepsis and aseptic technique revolutionized surgery. By adopting these sterile techniques, a surgeon operating on the brain or the skull, or both, with aseptic technique in a clean operating theater could complete the surgery with a significant reduction in surgical infection.
To diagnose a brain lesion or to localize a brain injury was not meaningful until the concept of neurological localization was formulated. In the 1860s, several investigators, including G. T. Fritsch (1838-1891) and E. Hitzig (1838-1907), as well as Paul Broca (1824-1880), first introduced the concept that each part of the brain corresponded to a particular function.123–125 In monitoring a patient with an expressive aphasia, Broca clarified localization of speech in the brain at an autopsy in 1861.124 Later, Carl Wernicke (1848-1904) identified a different area of the brain where speech was associated with conduction defects.126 These studies led to an explosion of research on the brain, with brain function being further investigated with the use of electrical stimulation in work pioneered by David Ferrier (1843-1928)127 and John Hughlings Jackson (1835-1911).128 Jackson is considered the founder of modern neurology. Both these physicians demonstrated important anatomic areas of brain function by electrical studies and developed an understanding of epilepsy. The field of neurology received its greatest impetus in this period. The neurological examination now became a rigorous study designed to uncover subtle anatomic and physiologic findings, which in turn provided a surgical map for surgeons to plan incisions and exploration.
The surgical personalities of the 19th century were varied and talented. Until the end of the 19th century, neurosurgery was not specialized, with operations still being performed by general surgeons. By the middle of the 19th century, we find the distinction between brain concussion and compression gradually being accepted. In 1841, William Sharp (1805-1896) published a short monograph titled Practical Observations on Injuries of the Head.129 He provides a modern definition of concussion as “a loss of function without change in structure.” Sharp advises against trephining in patients with concussion because there is no extravasation of blood to remove and it will not prevent inflammation. He notes that the middle meningeal artery is the usual source of an epidural hematoma and concludes his monograph with a review of Percivall Pott’s earlier surgical experience with head injuries; in Pott’s 43 reported cases, 29 were operated on with 17 recoveries and 12 deaths, whereas in the 14 patients who were not operated on, 2 recovered and 12 died.
Sir Jonathan Hutchinson (1828-1913) provided an important chapter in the acceptance of neurological signs and symptoms as indicators for surgical intervention. In 1867, the same year that Lister published his first papers on the role of antisepsis in surgery, Hutchinson published a series of papers on brain compression that introduced a new diagnostic sign for head injury.130 His recognition of third nerve paralysis remains one of the most useful signs of head injury and increased intracranial pressure. Coupled with the recognition of a lucid interval after head trauma, it provided an important neurological sign that enabled surgeons to recognize the need for trephining. Hutchinson also argued that the finding of a fixed and dilated pupil was likely to be on the side of the hematoma. For the first time in 350 years, since a 16th century artist (Gerzdorf,62 1517) recorded this observation, the mechanism and significance of this finding were established.
He went on modestly to note: “nor can we boast of having learnt much which may aid us in the diagnosis of future cases, with the one exception of having discovered the meaning of the one dilated pupil. This point we will store up carefully for future use.”130
Sir Rickman Godlee (1849-1925) removed one of the most celebrated brain tumors, the first to be successfully diagnosed by cerebral localization, in 1885.131 The patient had suffered for 3 years from focal motor seizures (Fig. 1-57). They started as focal seizures of the face and proceeded to involve the arm and then the leg. For 3 months before surgery the patient also experienced weakness and eventually had to give up his work. Working with a neurologist, Alexander H. Bennett (1848-1901), Godlee was able to localize the tumor and remove it. This case was an important landmark in neurosurgery. For the first time a neurologist, basing his conclusions on the findings from a neurological examination, localized a brain tumor and recommended removal to a surgeon. Godlee made an incision over the rolandic area and through a small cortical incision removed the tumor. The patient survived the surgery with mild weakness and did well only to die of a wound infection 1 month later. Added to the importance of the surgery itself was the presence in the operation room of three important gentlemen: Hughes Bennett, a prominent English physician, and J. Hughlings Jackson and David Ferrier, two local neurologists. These gentlemen were extremely interested in whether cerebral localization studies could provide good results in the operating theater. This operation was the impetus that truly moved neurosurgery forward, a landmark operation.
Three years later, in 1888, Victor Horsley (1857-1916) performed the first removal of a spinal cord tumor, a tumor that had been diagnosed and localized by William Gowers (1845-1915) (Fig. 1-58).132 Horsley performed a laminectomy on Gower’s patient, Captain Golby. Golby was slowly losing function in his legs from a spinal cord tumor. Gowers localized the tumor by examination and suggested to Horsley where to operate; the tumor was successfully removed. A postoperative photograph of the patient with a healed midline thoracic scar is included in the original paper.
William Gowers (1845-1915) was one of an extraordinary group of English neurologists of that era. Using some of the recently developed techniques in physiology and pathology, he made great strides in refining the concept of cerebral localization. Gowers was noted for the clarity and organization of his writing, works that remain classics in the field.133,134 Studies such as these allowed surgeons to consider operating on the central nervous system (CNS) for other than heroic circumstances. Godlee and Horsley were trained general surgeons who had the ambition and fortitude to surgically explore the CNS now that their neurology colleagues could localize the lesion.
The successful removal of a spinal tumor brought Sir Victor Alexander Haden Horsley (1857-1916) to the forefront in the development of neurosurgery during its birthing period (Fig. 1-59). Horsley began his experimental studies on the brain in the early 1880s, at the height of the cerebral localization controversies. Using faradic stimulation he worked with Sharpey-Schäfer in analyzing and localizing motor functions in the cerebral cortex, internal capsule, and spinal cord of primates.135 In a classic study with Gotch (1891) using a string galvanometer, he showed that electrical currents originate in the brain.136 These experimental studies showed Horsley that localization was possible and that operations on the brain could be conducted safely by using techniques adapted from general surgery.
Horsley made a number of technical contributions to neurosurgery, including the use of beeswax to stop bone bleeding.137,138 He performed one of the earliest operations for craniostenosis and relief of increased intracranial pressure. He pioneered the technique of sectioning the posterior root of the trigeminal nerve for trigeminal neuralgia, the first effective treatment of this relentless condition.139 Using his technical gifts, he helped Clarke design the first useful stereotactic unit for brain surgery. Although the unit was used only on animals, the Horsley-Clark stereotactic frame remains the standard from which all subsequent designs have derived (Fig. 1-60).140
William Macewen (1848-1924), a Scottish surgeon and pioneer in the field of neurosurgery, successfully accomplished one of the early brain operations on July 29, 1879.141 Macewen operated on a 14-year-old child and removed a periosteal tumor over the right eye (Figs. 1-61 and 1-62). Using meticulous technique and the recently developed neurological examination, he localized the tumor and removed it. After surviving for 8 years, Bright’s disease developed and the patient died; at autopsy no tumor was detected. By 1888, Macewen had operated on 21 neurosurgical cases with only 3 deaths and 18 successful recoveries—a remarkable turnabout from earlier experience. When Macewen published his monograph in 1893 on pyogenic infections of the brain and their surgical treatment, a revolution occurred in neurosurgery.142 This monograph was the earliest to deal with the successful treatment of brain abscess. His morbidity and mortality statistics, reflecting the application of localization techniques and effective antisepsis, were not inferior to those in any series reported today. Without good surgical results, the neurologist of that era was hesitant to recommend surgery; Macewen helped immensely to make the case for soundly conducted operations on the brain.
Though not sharing the hopelessness of the opinion expressed in 1883 by a distinguished neurologist as to the inutility of operations on the brain undertaken for abscess, the author was then inclined to take a more sombre view of the prospects of recovery from such operations than his subsequent experience has proven to be necessary. He now regards an uncomplicated cerebral abscess, early recognized, accurately localized, and promptly operated on, as one of the most satisfactory of all intracranial lesions, the patient being at once relieved from a perilous condition, and usually restored to sound health [from the preface to Pyogenic Infective Diseases of the Brain and Spinal Cord].142
In the United States, among the earliest pioneers in neurosurgery was William W. Keen (1837-1924), professor of surgery at Jefferson Medical College in Philadelphia. Keen was one of the strongest American advocates for use of the recently introduced Listerian antiseptic techniques in surgery (Fig. 1-63).143 The concept of surgical bacteriology, along with those of asepsis and antisepsis, was aggressively discussed in his writings.144 He prepared one of the earliest American monographs on neurosurgery, a book titled Linear Craniotomy.143 He developed a technique for the treatment of spastic torticollis involving division of the spinal accessory nerve and the posterior roots of the first, second, and third spinal nerves (Fig. 1-64).145 For treatment of the excoriating pain associated with trigeminal neuralgia he devised a technique for resection of the gasserian ganglion.146 Keen exercised a rare inventiveness in surgical technique; he used bent spoons from his kitchen as brain retractors! Keen was also the first to introduce the Gigli saw to American surgeons, a technical advance in performing a craniotomy.147
A professor of surgery in Berlin, Fedor Krause (1857-1937) was an early general surgeon who developed a keen interest in neurosurgery. Krause’s three-volume atlas on neurosurgery, published in the first decade of the 20th century, was among the first to graphically detail the techniques of neurosurgery. Digital extirpation of a meningioma is described.148 A number of neurosurgical techniques are reviewed, including resection of scar tissue for the treatment of epilepsy. Krause was an early pioneer in the extradural approach to the gasserian ganglion for the treatment of trigeminal neuralgia (Figs. 1-65 and 1-66).
The first American monograph devoted to brain surgery was written not by a neurosurgeon but by a New York neurologist, Allen Starr (1854-1932).149 Starr was professor of nervous diseases at Columbia University and an American leader in neurology. He trained in Europe and worked in the laboratories of Erb, Schultze, Meynert, and Nothnagle—experiences that provided him with a strong foundation in neurological diagnosis (Fig. 1-67). Working closely with Charles McBurney (1845-1913), a New York City general surgeon, he came to the realization that not only could brain surgery be done safely but also was clearly necessary in the treatment of certain neurological problems.149–151 Starr summarized his views in the preface:
Brain surgery is at present a subject both novel and interesting. It is within the past five years only that operations for the relief of epilepsy and of imbecility, for the removal of clots from the brain, for the opening of abscesses, for the excision of tumors, and the relief of intra-cranial pressure have been generally attempted. Brain surgery has as its essential basis the accurate diagnosis of cerebral lesions, which was impossible until the localization of cerebral functions had been determined. And this diagnosis must be made by the physician before the surgeon is called in to remove the disease. It is the object of this book to state clearly those facts regarding the essential features of brain disease which will enable the reader to determine in any case both the nature and situation of the pathological process in progress, to settle the question whether the disease can be removed by surgical interference, and to estimate the safety and probability of success by operation. The facts have been reached by a careful study of the literature of the subject and by a considerable personal experience. It is my hope that this work may aid the physician to diagnosticate brain diseases with more accuracy, and to select such cases as are properly open to surgical treatment by trephining, and also that may enable the surgeon to perform his delicate task with more precision and with a fuller knowledge of those principles of local diagnosis which should form this constant guide.149
Harvey William Cushing (1869-1939) was the founder of American neurosurgery (Figs. 1-68 and 1-69). Cushing had the good fortune to be alive and in training during the formative years of neurosurgery. Educated at Johns Hopkins under one of the premier general surgeons, William Halsted (1852-1922), Cushing learned meticulous surgical technique from his mentor. As was standard then, Cushing spent time in Europe; he worked in the laboratories of Theodore Kocher in Bern, where he investigated the physiology of CSF. These studies led to his important monograph in 1926 on the third circulation.152 It was during this period of experimentation that the cerebral phenomenon of increased intracranial pressure in association with hypertension and bradycardia was defined; it is now referred to as the Cushing phenomenon. While traveling through Europe, he met several important surgical personalities, including Macewen and Horsley. These individuals provided the impetus for Cushing to consider neurosurgery as a full-time endeavor.
Cushing’s contributions to the literature of neurosurgery are too extensive for this brief chapter. Among his most significant is a monograph on pituitary surgery published in 1912.153 This monograph was to inaugurate a sterling career in pituitary studies. Cushing’s syndrome was defined in his final monograph on the pituitary gland published in 1932.154 In a monograph written with Percival Bailey in 1926, Cushing introduced the first rational approach to the classification of brain tumors.155 Cushing’s monograph on meningioma, written in collaboration with Louise Eisenhardt in 1938, remains the standard for the profession.156
Cushing retired as Moseley Professor of Surgery at Harvard in 1932. When he completed his 2000th brain tumor operation, he had unquestionably made one of the most important contributions to the field of neurosurgery—a contribution comprising meticulous, innovative surgical techniques and a career-long attempt to understand brain function from both a physiologic and a pathologic perspective.157 An ardent bibliophile, Cushing spent his final years in retirement as Sterling Professor of Neurology at Yale, where he put together his extraordinary monograph on Andreas Vesalius.158 Cushing’s life was faithfully recorded by his close friend and colleague John F. Fulton (1946)159 and in a recent biography by Michael Bliss.160
If Harvey Cushing is the father of American neurosurgery, his prodigal son is Walter Dandy (1886-1946) (Fig. 1-70), who trained under Cushing at Johns Hopkins Hospital. Dandy made a number of important contributions to neurosurgery. Using the serendipitous finding of Luckett,161 the presence of air in the ventricles after a skull fracture, Dandy developed the technique of pneumoencephalography (PEG).162–164 The introduction of PEG provided the neurosurgeon, for the first time, the opportunity to localize a tumor by analyzing the displacement of air in the ventricles. Dandy was an innovative neurosurgeon, considerably more aggressive in style and technique than Cushing. Dandy was the first to show that acoustic neuromas could be removed in their totality.165,166 He devoted much effort to the treatment of hydrocephalus.167,168 He first introduced the technique of ablating and removing the choroid plexus to reduce the production of CSF.169 Dandy was among the first to surgically deal with cerebral aneurysms by obliterating them with snare ligatures or metal clips.170 His monograph on the third ventricle and its anatomy remains a textbook standard to this day, with illustrations that are among the best ever produced.171
In the field of spine surgery, two important American figures appeared in the first quarter of the 20th century: Charles Elsberg (1871-1948), professor of neurosurgery at the New York Neurological Institute, and Charles Frazier (1870-1936), professor of surgery at the University of Pennsylvania. Work in the 19th century by J. L. Corning (1885) had shown that lumbar puncture can be safely performed.172 This procedure was popularized by H. Quincke, who used it for the treatment of hydrocephalus, and from this procedure spine surgery developed.173,174 When Charles Frazier’s book on spine surgery appeared in 1918, the most comprehensive work on spine surgery yet to be written became available.175 Frazier summarized much of the spine surgery literature to that point. He established that spine surgery could be performed with minimal morbidity and mortality. Frazier’s experience in World War I led him to devote his career to neurosurgery. A gracious person, he followed a heavy work schedule. It was not uncommon for Frazier to sweep the operating room at the completion of a case just to relax his shoulder muscles, only then discussing the operation just completed with his colleagues.
Charles Elsberg (1871-1948), a pioneer in spine surgery, had surgical technique that was described as impeccable and consistently led to excellent outcomes. In 1912 Elsberg published a landmark paper in which he reported on a series of 43 laminectomies.176 In 1916 he published the first of what were to be three monographs on surgery on the spine.177 One of Elsberg’s seminal contributions was a staged technique to allow the delivery of an intramedullary spinal cord tumor.176 It consisted of first a myelotomy, which in theory allowed an intramedullary tumor to deliver itself over time into the laminectomy. Then at a second operation the tumor could be removed after having extruded through myelotomy. Elsberg was known as a driven worker who approached the practice of neurosurgery with a fierce intensity, always looking for new techniques. Working with Cornelius Dyke (1900-1943), a neuroradiologist at the New York Neurological Institute, he treated spinal glioblastomas with directed radiation in the operating room after the tumor had been exposed! Procedures such as these were performed with the patients receiving only local anesthesia. During the  -hour therapy, while the radiation was being delivered, the surgeon and assistants stood off in the distance behind a glass shield.178
-hour therapy, while the radiation was being delivered, the surgeon and assistants stood off in the distance behind a glass shield.178
Conclusion
The 19th century brought the introduction of anesthesia, antisepsis, and cerebral localization. The later half of the 19th century produced strong surgical personalities, surgeons adventurous enough to perform surgery on the formidable cranial vault and spine. In the first half of the 20th century, formalization of the field of neurosurgery occurred. Besides the pioneering techniques of Dandy, Cushing, and others, a number of diagnostic techniques were introduced that made it easier for the neurosurgeon to localize lesions. One technique, myelography with opaque substances, was brought forward by Jean Athanase Sicard (1872-1929).179 Using radiopaque iodized oil, the spinal cord and its elements could be outlined on radiographs. Antonio Caetano de Egas Moniz (1874-1955), professor of neurology in Lisbon, Portugal, perfected arterial catheterization techniques and the cerebral angiogram in animal studies.180,181 This procedure, in combination with PEG, offered the neurosurgeon a detailed view of the intracranial contents. Moniz was awarded the Nobel Prize in 1949 for his work on prefrontal lobotomy for psychiatric disorders.
In 1929 Alexander Fleming (1881-1955) published a report on the first observation of a substance that appeared to block a bacterium from growing.182 This substance, identified as penicillin, introduced a new era of medicine and surgery. With the World War II experience, antibiotics for the treatment of bacterial infection were perfected, thereby even further reducing the risk for infection during brain and spine surgery.
, Bakay L. An Early History of Craniotomy. From Antiquity to the Napoleonic Era. Springfield. Ill: Charles C Thomas; 1985.
, Bakay L. Neurosurgeons of the Past. Springfield, III: Charles C Thomas; 1987.
, Castiglioni A. A History of Medicine. Translated from the Italian and Edited by E.B. Krubhaar. revised and enlarged. 2nd ed. New York: A.A. Knopf. 1947.
, Clarke ES, Dewhurst K. An Illustrated History of Brain Function. Oxford. 1972. Reprinted in 1992 by Norman Publishing, San Francisco
, Clarke E, OMalley CD. The Human Brain and Spinal Cord. A historical study illustrated by writings from antiquity to the twentieth centry. Berkeley: University of California Press; 1968. Reprinted in 1992 by Norman Publishing, San Francisco
, DeJong RN. A History of American Neurology. New York: Raven Press; 1982.
, Garrison FH. An Introduction to the History of Medicine. revised and enlarged. 4th ed. Philadelphia: Saunders. 1929.
, Gurdjian ES. Head Injury from Antiquity to the Present with Special Reference to Penetrating Head Injury. Springfield, III: Charles C. Thomas; 1973.
, Haymaker W, Schiller F. The Founders of Neurlogy, 2nd ed. Springfield, III: Charles C. Thomas; 1970.
, Leonardo RA. History of Surgery. New York: Froben Press; 1943.
, McHenry LC. Garrison’s History of Neurology Revised and Enlarged with a Bibliography of Classical, Original and Standard Works in Neurlogy. Springfield, III: Charles C. Thomas; 1969.
, Mettler CC, editor. History of Medicine. A Correlative Text, Arranged According to Subjects. Philadelphia: Blakiston, 1947.
, Meyer A. Historical Aspects of Cerebral Anatomy. London: Oxford University Press; 1971.
, Norman JM, editor. Norton’s Medical Bibliography, 5th ed, Cambridge, UK: Scholar Press, 1991.
, Poynter FNL, editor. The History and Philosophy of Knowledge of the Brain and its Functions. Springfield, III: Charles C. Thomas, 1958.
, Rose FC, Bynum WF. Historical Aspects of the Neurosciences. A Festschrift for Macdonald Critchley. New York: Raven Press; 1982.
, Sachs E. The History and Development of Neurological Surgery. New York: Paul Hoeber; 1952.
, Soury J. Le Système Nerveux Centrale Structure et Fonctions. Histoire Critique des Théories et des Doctrines. Paris: Georges Carré & Naud; 1899.
, Spillane JD. The Doctrine of the Nerves. Chapters in the History of Neurology. London: Oxford University Press; 1981.
, Walker AE. A History of Neurological Surgery. Baltimore, Md: Williams and Wilkins; 1951.
, Wilkins RH. Neurosurgical Classics. Compiled by Robert H. Wilkins. New York: Johnson Reprint Co; 1965.
1 Clowes W. A right frutefull and approved treatise, for the artificiall cure of that malady called in Latin Struma, and in English, the evill, cured by kinges and queens of England. Very necessary for all young practizers of chirurgery. Written by William Clowes, one of her Maiesties chyrurgions, in the yeare of our Lord 1602. London: Edward Allde; 1602.
2 Hippocrates. TOY MEΓAΛOY IΠΠOKPATOYΣΠANTΩN TΩN IATPΩN Magni Hippocratis Medicorvm Omnivm Facile Principis, Opera Omnia quae extant nunc denuo Latina Interpretations & Annotatioibus illustrata Anutio Foesio. Genevae: S. Chouet; 1657-1662.
3 Tyson RA, Dyer Alcauskas ES, editors. Catalogue of the Hrdlicka Paleopathology Collection. San Diego, CA: San Diego Museum of Man, 1980.
4 Marino R, Gonzales-Portillo M. Preconquest Peruvian neurosurgeons: A Study of Inca and Pre-Columbian trephination and the art of medicine in ancient Peru. Neurosurgery. 2001;49:477-478.
5 Gurdjian ES. Head Injury from Antiquity to the Present with Special Reference to Penetrating Head Injury. Springfield, IL: Charles C Thomas; 1973.
6 Papyrus Ebers. The papyrus Ebers. The greatest Egyptian medical document. Translated by B. Ebbell. Copenhagen: Levin & Munksgard. 1937.
7 Reisner G. The Hearst Medical Papyrus. The Bancroft Library Collection. University of California at Berkeley; 1905.
8 Breasted JH. The Edwin Smith Papyrus. Published in Facsimile and Hieroglyphic Transliteration with Translation and Commentary. Chicago: University of Chicago Press; 1930.
9 Feldman RP, Goodrich JT. The Edwin Smith Papyrus. Childs Nerv Syst. 1999;15:281-284.
10 Chapman P. The Alexandrian Library: Crucible of a Renaissance. Neurosurgery. 2001;49:1-14.
11 Hippocrates. Coi Medicorvm Omnivm longe Principia, octoginta Volumina, quibus maxima ex parte, annorum citciter duo millia Latina catruit lingua, Craciuero, Arabes & Prafcinostri, scripta sua illustrarunt. latuita te donata, CLEMENT LVII, Pont. Ax rome. Rome: Franciscus Minutius Calvus; 1525.
12 Hippocrates. TOY MEΓAΛOY IΠΠOKPATOYΣΠANTΩN TΩN IATPΩN Magni Hippocratis Medicorvm Omnivm Facile Principis, Opera Omnia quae extant nunc denuo Latina Interpretations & Annotatioibus illustrata Anutio Foesio. Genevae: S. Chouet; 1657-1662.
13 Hippocrates. Aphorismi, cum Galeni commentariis, Nicolao Leoniceno interprete, Praedictiones, cum Galeni commentariis, Laurentio Laurentiano interprete. Paris: Simon Sylvius; 1525.
14 Hippocrates. The Genuine Works of Hippocrates translated from the Greek by Francis Adams. London: Sydenham Society; 1849. pp 421-466 for “Injuries on the head”. De capitis vulneribus
15 Dimopoulos VG, Machinis TG, Fountas KN, et al. Head injury management algorithm as described in Hippocrates’ “Peri ton en cephali traumation.”. Neurosurgery. 2005;57:1303-1305.
16 Panourias JG, Skiadas PK, Saklas DE, et al. Hippocrates: a pioneer in the treatment of head injuries. Neurosurgery. 2005;37:181-189.
17 Hippocrates. The Genuine Works of Hippocrates. Translated from the Greek by Francis Adams with a preliminary discourse and annotations. New York: William Wood & Co; 1925.
18 Marx KFH. Herophilus. ein Beitrag sur Geschichte der Medicin. Carlsruhe und Baden: Verlag DR. Marr’schen; 1838.
19 Herophilus. Medicae Artis Principes post Hippocratem et Galenum. In:. Geneva: Henri Estienne. 1567.
20 Acar F, Nadar S, Guvencer M, et al. Herophilus of Chalcedon: a pioneer of neurosurgery. Neurosurgery. 2005;56:861-867.
21 Viale G. The rete mirabile of the cranial base: a millenary legend. Neurosurgery. 2006;58:1198-1208.
22 Vesalius A. De Humani Corporis Fabrica. Basel: Oporinus; 1543.
23 Bataille B, Wager M, Lapierre F, et al. The significance of the rete mirabile in Vesalius’ work: an example of the dangers of inductive inference in medicine. Neurosurgery. 2007;60:761-768.
24 Berengario da Carpi Jacobi. Isagoge Breves, Perlucide ac Uberime, in Anatomia Humani Corporis. Bologna: Impressum per Benedictum Hectoris; 1522.
25 Celsus AAC. De Medicina. Florentiae: Nicolaus Laurentius; 1478.
26 Celsus AAC. De Medicina. With an English translation by W.G. Spencer. London: W. Heinemann. 1935-1938.
27 Galen of Pergamum. Omnia Quae Extant Opera in Latinum Sermonem Conversa (Quinta ed). Venice: Apud Juntas; 1576-1577.
28 Galen. De Usu Partium. See May MT, Galen on the Usefulness of the Parts of the Body. Ithaca and London: Cornell University Press; 1968.
29 Galen C. Experimental section and hemisection of the spinal cord (Taken from De Locis affectibus). Ann Med Hist. 1917;1:367-370.
30 Aeginetes Paulus. Opus de Re Medica Nunc Primum Integrum. Köln: Joannes Soter; 1534.
31 Aeginetes Paulus. The Seven Books of Paulus Aegineta. Adams F, trans. London: Sydenham Society. 1844-1847.
32 Rhazes L. Opera Parva. Lyons: Gilbertus de Villiers, Johannis de Ferris; 1511.
33 Avicenna. Liber canonis, de medicinis cordialibus, et cantica. Basel: Joannes Heruagios; 1556.
34 Sabuncunoglu, Serefeddin. Imperial surgery (translated from Arabic). Ottoman Empire circa 15th century. From a later copied manuscript in the author’s collection, circa 1725.
35 Naderi S, Acar F, Mertol T, et al. Functional anatomy of the spine by Avicenna in his eleventh century treatise Al-Qanun fi al-Tibb (The Canons of Medicine). Neurosurgery. 2005;52:1449-1454.
36 Aciduman A, Belen D, Simsek S. Management of spinal disorders and trauma in Avicenna’s Canon of Medicine. Neurosurgery. 59, 2006. 397–303
37 Scultetus J. ρ πη. Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.
πη. Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.
38 Albucasis. Liber Theoricae Necnon Practicae Alsaharavii. Augsburg: Sigismundus Grimm & Marcus Vuirsung; 1519.
39 Albucasis, Spink MS, Lewis GL. Albucasis on Surgery and Instruments. transl-ed. Berkeley, CA: University of California Press. 1973.
40 Al-Rodhan NRF, Fox JL. Al-Zahrawi and Arabian neurosurgery, 936-1013 AD. Surg Neurol. 1986;25:92-95.
41 Divitiis E, Cappabianca P, Divitiis O. The “Schola Medica Salernitana”: the forerunner of the modern university medical schools. Neurosurgery. 2005;55:722-745.
42 Africanus Constantinus. Constantini Africani Post Hippocratem et Galenum. Basel: Henricus Petrus; 1536.
43 Roger of Salerno. Practica Chirurgiae. In: Guy de Chauliac Cyrurgia et Cyrurgia Bruni, Teodorici, Rolandi, Lanfranci, Rogerii, Bertapalie. Venice: Bernardinus Venetus de Vitalibus; 1519. Illustrations from Livre de Chirurgie, France 13th century. Courtesy of British Museum, London, England. Manuscript Sloane 1977
44 Corner G. The Bamberg Surgery. Bull Inst Hist Med. 1937;5:1-32.
45 Theodoric Bishop of Cervia. The Surgery of Theodoric, ca. A.D. 1267. Campbell E, Colton J, transl. New York: Appleton-Century-Crofts. 1955-1966. See Book II, ch 27
46 Leonardo RA. History of Surgery. New York: Froben Press; 1943. 110-116
47 William of Saliceto. Chirurgia. Venice: F di Pietro; 1474. See also Leonardo RA, History of Surgery. New York, Froben Press; 1943:111
48 Leonard of Bertapalia. Chirurgia. In: Guy de Chauliac Cyrurgia et Cyrurgia Bruni, Teodorici, Rolandi, Lanfranci, Rogerii, Bertapalie. Venice: Bernardinus Venetus de Vitalibus; 1519.
49 Leonard of Bertapalia. On Nerve Injuries and Skull Fractures. Ladenheim JC, transl. Mount Kisco, NY: Futura. 1989. 53-55
50 Lanfranchi of Milan. Chirurgia. In: Guy de Chauliac Cyrurgia et Cyrurgia Bruni, Teodorici, Rolandi, Lanfranci, Rogerii, Bertapalie. Venice: Bernardinus Venetus de Vitalibus; 1519.
51 Pagel JL, editor. Die Chirurgie des Heinrich von Mondeville (Hermondaville). Berlin: Hirschwald, 1892.
52 Guy de Chauliac. Chirurgia magna. In: Guy de Chauliac Cyrurgia et Cyrurgia Bruni, Teodorici, Rolandi, Lanfranci, Rogerii, Bertapali. Venice: Bernardinus Venetus de Vitalibus; 1519. See also Leonardo, RA: History of Surgery. New York, Froben Press, 1943:116
53 Guy de Chauliac. Guy de Chauliac (A.D. 1363) on Wounds and Fractures. Chicago: Published by translator. 1923. See also reference 46, Leonardo History of Surgery, p 116
54 Powers D’Arcy. De arte phisicali et de cirurgia Or Master John Arderne, Surgeon of Newark Dated 1412. London: John Bale, Sons & Danielsson, Ltd.; 1922.
55 Wangensteen OH, Wangensteen SD. The Rise of Surgery. From Empiric Craft to Scientific Discipline. Minneapolis: University of Minnesota Press; 1978. 702
56 Singer CS. A medical compendium of the first half of the twelfth century. Manuscript 17, St. Johns College, Oxford about A.D. 1110. Bull Soc Med Hist. 1917-1922;11:53-96.
57 Leonardo da Vinci. Quaderni d’Anatomia. Christiania: Jacob Dybwad; 1911-1916.
58 Hopstock H. Leonardo as an anatomist. In: Singer C, editor. Studies in the History of Medicine. Oxford: Clarendon Press, 1921.
59 Leonardo da Vinci, Keele KD, Pedretti C. Corpus of the Anatomical Studies in the Collection of Her Majesty the Queen at Windsor Castle. New York: Harcourt Brace Jovanovich, 1979.
60 Goodrich JT. Sixteenth century Renaissance art and anatomy: Andreas Vesalius and his great book—a new view. Med Heritage. 1985;1:280-288.
61 Brunschwig H. Dis ist das Buch der Cirurgia. Strassbourg: J Grüninger; 1497.
62 Gersdorff HF. Feldtbuch der Wundartzney Strassbourg. J Schott. 1517. See also Flamm ES. The dilated pupil and head trauma. Med Hist. 1972;16:194-199
63 Paré A, Johnson T. The Workes of That Famous Chirurgion Ambroise Parey. trans. London: Richard Coates. 1649.
64 Paré A. Opera A docto viro plerisque locis recognita: et Latinitate donata, Jacobi Guillemeau. Paris: Apud Jacobum Du-Puys; 1582. —see Book X
65 Paré A. Dix livres de la chirurgie avec le magasin des instruements necessaries à icelle. Paris: Jean Le Royer; 1564. First description of the use of the ligature instead of cautery
66 Paré A. La methode Curative des Playes et Fractures de la Teste Humanin. Paris: Jean le Royer; 1561.
67 Berengario da Carpi J. Tractatus de Fractura Calvae Sive Cranei. Bologna: Hieronymus de Benedictus; 1518.
68 Berengario da Carpi J. Isagogae Breves perlucide ac ubertine in Anatomiam Humani Corporis. Bononiae, Italy: B. Hectoris; 1522.
69 Dryander J. Anatomiae. Marburg: Eucharius Ceruicornus; 1537.
70 Hanigan WC, Ragen W, Foster R. Dryander of Marburg and the first textbook of neuroanatomy. Neurosurgery. 1990;26:489-498.
71 Coiter V. Externarum et Internarum Principalium Humani Corporis Partium Tabulae Atque Anatomicae Exercitationes Observationesque Variae. Nürnberg: Theodoricus Gerlatzenus; 1573.
72 della Croce GA. Chirurgiae Libri Septem. Venice: Jordanus Zilettus; 1573.
73 Vesalius A. De Humani Corporis Fabrica Libri Septem. Basel: Joannes Oporinus; 1543.
74 Vesalius A. Vesalius on the Human Brain. Singer C, trans-ed. London: Oxford University Press. 1952.
75 Vesalius A. De Humani Corporis Fabrica. Basel: Oporinus; 1555.
76 Estienne C. De Dissectione Partium Corporis Humani Libri Tres. Paris: Simon Colinaeus; 1546.
77 Willis T. Cerebri Anatome: Cui Accessit Nervorum Descriptio et Usus. London: J Flesher; 1664.
78 Grand W. The Anatomy of the Brain by Thomas Willis. Neurosurgery. 1999;45:1234-1236.
79 Johnson S. A Dictionary of the English Language. London: W. Strahan for J. & P. Knaptonm; 1755.
80 Vesling J. Syntagma Anatomicum, 2nd ed. Padua, Italy: Paulus Frambottus; 1651.
81 van de Spiegal A, Casserius G. De Humani Corporis Fabrica Libri Decem, Tabulis XCIIX Aeri Incisis Elegantissimis. Venice: Evangelista Deuchinus; 1627.
82 Fallopius G. Observationes Anatomicae. Venice: Marcus Antonius Ulmus; 1561.
83 Ridley H. The Anatomy of the Brain, Containing Its Mechanisms and Physiology: Together with Some New Discoveries and Corrections of Ancient and Modern Authors upon That Subject. London: Samuel Smith; 1695.
84 Clarke E, O’Malley CD. The Human Brain and Spinal Cord. A Historical Study Illustrated by Writings from Antiquity to the Twentieth Century. Berkeley, CA: University of California Press; 1968. Reprinted in 1992 by Norman Publishing, San Francisco, CA
85 Clarke ES, Dewhurst K. An Illustrated History of Brain Function. Oxford: Sandford Publications; 1972.
86 Fabry W. Observationum et Curationum Chirurgicarum Centuriae. Basle: Frankfurt, & Lyons; 1606-1641. A later collected works also contains a number of neurosurgical cases. Opera Observation et Curationum. Frankfurt: Joannis Beyerj; 1646
87 Woodall J. The Surgeons Mate. London: E. Griffin; 1617.
88 Woodall J. The Surgeons Mate or Military and Domestique Surgery Discouering faithfully & plainly ye method and order of the Surgeons chest, ye uses of the instruments. London: Rob Young for Nicholas Bourne; 1639.
89 Yonge J. Wounds of the Brain Proved Curable, Not Only by the Opinion and Experience of Many (the Best) Authors, but the Remarkable History of a Child Four Years Old Cured of Two Very Large Depressions, with the Loss of a Great Part of the Skull, a Portion of the Brain Also Issuing thorough a Penetrating Wound of the Dura and Pia Mater. London: Henry Faithorn and John Kersey; 1682.
90 Belloste A. Le chirurgien d’hopital, enseignant une maniere douce & facile de guerit promptement toutes sortes de playes. Paris: Laurent d’Houry; 1696.
91 Pott P. Observations on the Nature and Consequences of Wounds and Contusions of the Head, Fractures of the Skull, Concussions of the Brain. London: C. Hitch and L. Hawes; 1760. See preface x-xi
92 Pott P. Remarks on That Kind of Palsy of the Lower Limbs Found to Accompany a Curvature of the Spine. London: J. Johnson; 1779.
93 Pott P. Observations on the Nature and Consequences of Wounds and Contusions of the Head, Fractures of the Skull, Concussions of the Brain. London: C. Hitch and L. Hawes; 1760.
94 Petit JL. Traité des Maladies Chirurgicales, et des operations qui leur convienent. Ouvrage posthume. Paris: P. Fr. Didot; 1774.
95 Le Dran HF. Observations de Chirurgie. Paris: Charles Osmont; 1731.
96 Stone JL, Goodrich JT, Cybulski GR. John Hunter’s contributions to neuroscience. In: Boller F, Finger S, Tyler K, editors. History of Neurology. A Volume in the Handbook of Clinical Neurology Series, 3(rd) series. Edinburgh: Elsevier, 2008.
97 Hunter J. A Treatise on the Blood, Inflammation, and Gun-Shot Wounds. London: J. Richards; 1794.
98 Home E. Lectures on Comparative Anatomy; in Which Are Explained the Preparations in the Hunterian Collection. London: G & W Nichol; 1814-1828.
99 Abernethy J. Surgical Observations on Injuries of the Head and on Miscellaneous Subjects. Philadelphia: Thomas Dobson; 1811.
100 Leonardo RA. History of Surgery. New York: Froben Press; 1943. 236
101 Abernethy J. Pathological and Practical Researches on Diseases of the Brain and Spinal Cord. Edinburgh: Waugh and Innes; 1828.
102 Bell B. A System of Surgery. Edinburgh: C. Elliot; 1783-1788.
103 Bell B. A System of Surgery. Edinburgh: C. Elliot; 1783-1788. see Volume 3, Chapter X, Section II
104 Bell B. A system of surgery. Edinburgh: C. Elliot; 1783-1788. see Volume 3, Chapter X, Section I
105 Bell B. A system of surgery. Edinburgh: C. Elliot; 1783-1788. see Volume 3, Chapter X. Section III
106 Turner D. A Remarkable Case in Surgery: Wherein an Account is Given of an Uncommon Fracture and Depression of the Skull, in a Child about Six Years old; Accompanied with a Large Abscess or Aposteme upon the Brain. With Other Practical Observations and Useful Reflections Thereupon. Also an exact Draught of the Case, annex’d. And for the Entertainment of the Senior, but Instruction of the Junior Practitioners, Communicated. London: R. Parker; 1709.
107 Jones J. Plain Concise Practical Remarks, on the Treatment of Wounds and Fractures; to Which Is Added, an Appendix, on Camp and Military Hospitals; Principally Designed, for the Use of Young Military and Naval Surgeons, in North-America. New York: John Holt; 1775.
108 Heister L. Chirurgie in welcher alles was zur Wund-Artzney gehöret, nach der neuesten und besten Art. Nümberg: J. Hoffmann; 1718.
109 Heister L. A General System of Surgery in Three Parts. London: W. Innys; 1743.
110 Heister L. A General System of Surgery in Three Parts. London: W. Innys; 1743. see Book I, Chapter XIV, page 100
111 Morand FS. Opuscules de Chirurgie. Paris: Guillaume Desprez; 1768-1772. 161-168
112 Cotugno D. De Ischiade Nervosa Commentarius. Neapoli, apud Frat. Simonios. 1764.
113 Saucerotte LS. Mélanges de Chirurgie. Neapoli: Gay; 1801.
114 Bell C. Illustrations of the Great Operations of Surgery. London: Printed for Longman; 1821. et. al. see preface leaf iv
115 Bell C. Illustrations of the Great Operations of Surgery. London: Printed for Longman; 1821. et. al. see page 6
116 Wells H. A History of the Discovery of the Application of Nitrous Oxide Gas, Ether and Other Vapours to Surgical Operations. Hartford, CT: J.G. Wells; 1847. See also Wells EA. The Discoverer of Anaesthesia: Dr. Horace Wells of Hartford Tercentenary Commission. Yale University Press, 1933
117 Morton WT. Circular Morton’s Letheon. Boston: Dutton & Wentworth; 1846.
118 Simpson JY. Discovery of a new anaesthetic agent, more efficient than sulphuric ether. Lond Med Gaz. 1847;5:934-937. ns.
119 Lister J. On a new method of treating compound fractures, abscess, etc., with observations on the conditions of suppuration. (Baron Lister). Lancet. 1867;1;:326-329. 357-359, 387-389, 506-509; 2:95-96
120 Lister J. Collected Papers. Oxford, England: Clarendon Press; 1909.
121 Holmes OW. The contagiousness of puerperal fever. N Engl Q J. 1843;1:503-530. See pp. 530 for quote
122 Semmelweis IF. Die Aetiolgie, der Begriff unde die Prophylaxis des Kindbettfiebers. Vienna, and Leipzig: C.A. Hartleben’s Verlags-Expedition, Pest; 1861.
123 Fritsch GT, Hitzig E. Über die Elektrische Erregbarkeit des Grosshirns. Arch Anat Physiol Wiss Med. 1870:300.
124 Broca P. Remarques sur le Siège de la faculté du language articulé suivie d’une observation d’aphémie (perte de la parole). Bull Soc Anat Paris. 1861;36:330-337.
125 Broca P. Perte de la parole; ramollissement chronique et destruction partielle du lobe antérieur gauche du cerveau. Bull Soc Anthrop Paris. 1861;2:235-243.
126 Wernicke C. Der aphasische Symptomenkomplex. Breslau: M. Cohn & Weigert; 1874.
127 Ferrier D. The Functions of the Brain. London: Smith, Elder; 1876.
128 Jackson JH. Selected Writings. In: Taylor J, editor. Selected Writings of John Hughlings Jackson. New York: Basic Books, 1958.
129 Sharp W. Practical Observations on Injuries of the Head. London: John Churchill; 1841.
130 Hutchinson J. Four lectures on compression of the brain. Clinical Lectures and Reports of the London Hospital. 1867-1868;4:10-55.
131 Bennett AH, Godlee RJ. Case of cerebral tumor. Medical-Chirurgical Trans. 1885;68:243-245.
132 Gowers WR, Horsley V. A case of tumour of the spinal cord. Removal, recovery. Med Chirurg Trans. 1888;71:377-428.
133 Gowers WR. The Diagnosis of Diseases of the Spinal Cord. London: J and A. Churchill; 1880.
134 Gowers WR. Lectures on the Diagnosis of Diseases of the Brain. London: J. and A. Churchill; 1886-1888.
135 Horsley VAH, Sharpey-Schäfer EA. A record of experiments upon the functions of the cerebral cortex. Phil Trans R Soc Series B. 1889;179:1-25.
136 Gotch F, Horsley VAH. On the mammalian nervous system, its functions, and their localisation determined by an electrical method. Phil Trans R Soc Series B. 1891;182:267-275.
137 Tan TC, Black P. Sir Victor Horsley (1857-1916): Pioneer of neurological surgery. Neurosurgery. 2002;50:606-612.
138 Vilensky JA, Sinish PR, Stone JL, et al. The Publications of Sir Victor Horsley: a listing and an assessment. Neurosurgery. 2005;57:576-583.
139 Horsley VAH, Taylor J, Colman WS. Remarks on the various surgical procedures devised for the relief or cure of trigeminal neuralgia (tic douloureux). Br Med J. 1891;2:1240-1252.
140 Horsley V, Clarke RH. The structure and functions of the cerebellum examined by a new method. Brain. 1908;31:45-124.
141 Macewen W. Localization of cerebral lesions and antiseptic trephinning. Lancet. 1881;2:581-582.
142 Macewen W. Pyogenic Infective Diseases of the Brain and Spinal Cord. Glasgow: J. Maclehose & Sons; 1893.
143 Keen WW. Linear Craniotomy. Philadelphia: Lea Bros; 1891. Published a year earlier as a paper. Keen WW. Craniectomy for microcephalus. Med News. November 29, 1890
144 Keen WW, White JW. An American Textbook of Surgery for Practitioners and Students, 3rd ed. Philadelphia: WB Saunders; 1899.
145 Keen WW. A new operation for spasmodic wry neck, namely, division or exsection of the nerves supplying the posterior rotator muscles of the head. Ann Surg. 1891;13:44-52.
146 Keen WW, Spiller WG. On resection of the gasserian ganglion with a pathological report on seven ganglia. AJMS. 1898;116:503-532.
147 Keen WW. On the use of the Gigli wire saw to obtain access to the brain. Phila Med J. 1898;1:32-33.
148 Krause F. Surgery of the Brain and Spinal Cord Based on Personal Experiences. Translated by H. Haubold and M. Thorek. New York: Rebman Co; 1909-1912.
149 Starr MA. Brain Surgery. New York: William Wood and Co; 1893.
150 Starr MA. Discussion on the present status of the surgery of the brain. 2. A contribution to brain surgery, with special reference to brain tumors. Trans Med Soc New York. 1896;18:119-134.
151 McBurney C, Starr MA. A contribution to cerebral surgery. Diagnosis, localization and operation for removal of three tumors of the brain: with some comments upon the surgical treatments of brain tumors. Am J Med Sci. 1893;105:361-387.
152 Cushing H. Studies in Intracranial Physiology & Surgery. H. Milford, Oxford University Press; 1926.
153 Cushing H. The Pituitary Body and Its Disorders, Clinical States Produced by Disorders of the Hypophysis Cerebri. Philadelphia: JB Lippincott; 1912.
154 Cushing H. Papers Relating to the Pituitary Body, Hypothalamus, and Parasympathetic Nervous System. Springfield, IL: Charles C Thomas; 1932.
155 Bailey P, Cushing H. A Classification of the Tumors of the Glioma Group on a Histogenetic Basis with a Correlated Study of Prognosis. Philadelphia: JB Lippincott; 1926.
156 Cushing H, Eisenhardt L. Meningiomas, Their Classification, Regional Behavior, Life History and Surgical End Results. Springfield, IL: Charles C Thomas; 1938.
157 Cushing H. Intracranial Tumors. Notes upon a Series of Two Thousand Verified Cases with Surgical Mortality Percentages Pertaining Thereto. Springfield, IL: Charles C Thomas; 1932.
158 Cushing H. A Bio-Bibliography of Andreas Vesalius. New York: Schuman; 1943.
159 Fulton JF. Harvey Cushing. A Biography. Springfield, IL: Charles C Thomas; 1946.
160 Bliss M. Harvey Cushing. A Life in Surgery. New York: Oxford University Press; 2005.
161 Luckett WH. Air in the ventricles, following a fracture of the skull. Surg Gynecol Obstet. 1913;17:237-240.
162 Dandy WE. Ventriculography following the injection of air into the cerebral ventricles. Ann Surg. 1918;68:5-11.
163 Dandy WE. Röntgenography of the brain after the injection of air into the spinal canal. Ann Surg. 1919;70:397-403.
164 Dandy WE. Localization or elimination of cerebral tumors by ventriculography. Surg Gynecol Obstet. 1920;30:329-342.
165 Dandy WE. An operation for the total extirpation of tumors in the cerebellopontine angle. A preliminary report. Bull Johns Hopkins Hosp. 1922;33:344-345.
166 Dandy W. An operation for the total removal of cerebello-pontine (acoustic) tumors. Surg Gynecol Obstet. 1925;41:129-148.
167 Dandy WE, Blackfan DD. An experimental and clinical study of internal hydrocephalus. JAMA. 1913;61:2216-2217.
168 Dandy WE, Blackfan DD. Internal hydrocephalus: an experimental, clinical and pathologic study. Am J Dis Child. 1914;8:406-482.
169 Dandy WE. An operative procedure for hydrocephalus. Bull Johns Hopkins Hosp. 1922;33:189-190.
170 Dandy WE. Intracranial aneurysm of the internal carotid artery. Cured by operation. Ann Surg. 1938;107:654-659.
171 Dandy WE. Benign Tumors of the Third Ventricles. Springfield, IL: Charles C Thomas; 1933.
172 Corning JL. Spinal Anesthesia and Local Medication of the Cord. N Y Med J. 1885;42:483-485.
173 Quincke J. Die lumbalpunction des Hydrocephalus. Berl Klin Wochnschr. 1891;28:929-933. 965-968
174 Quincke J. Die Diagnostische und therapeutische Bedeutung der Lumbalpunktion. Klinischer Vortrag Deutsche Med Wochnschr. 1905;31:1825-1828. 1869-1872
175 Frazier C. Surgery of the Spine and Spinal Cord. New York: Appleton; 1918.
176 Elsberg CA. Surgery of intramedullary affections of the spinal cord anatomic basis and technic with report of cases. JAMA. 1912;59:1532-1536.
177 Elsberg CA. Diagnosis and Treatment of Surgical Diseases of the Spinal Cord and Its Membranes. Philadelphia: WB Saunders; 1916.
178 Pool L. The Neurological Institute of New York 1909-1974 with Personal Anecdotes. Lakeville: Pocket Knife Press; 1975.
179 Sicard JA, Forestier J. Méthode radiographique d’exploration de la cavité épidurale par le lipiodol. Rev Neurol. 1921;37:1264-1266.
180 Moniz CE. L’encéphalographie artérielle, son importance dans la localisation des tumeurs cérébrales. Rev Neurol. 1927;2:72-90.
181 Moniz CE. Diagnostic des tumeurs cérébrales et épreuve de l’encéphalographie artérielle. Paris: Masson & Cie; 1931.
182 Fleming A. On the antibacterial action of cultures of a Penicillium with special reference to their use in the isolation of B. influenza. Br J Exp Biol. 1929;10:226-236.


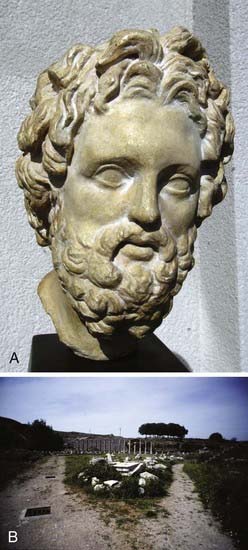
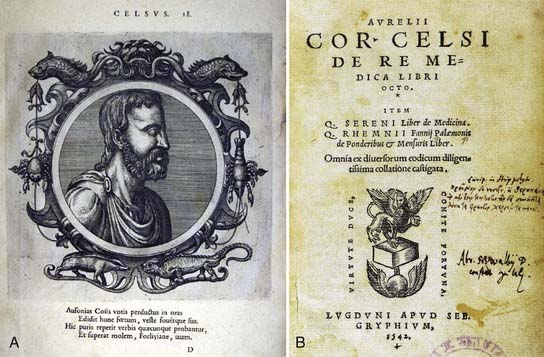
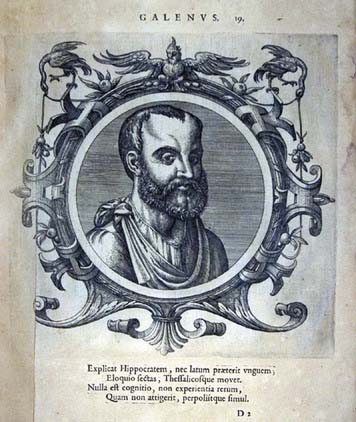
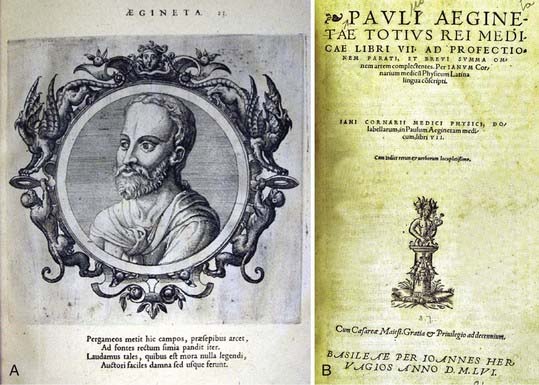
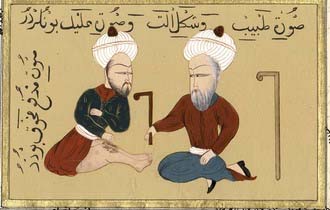
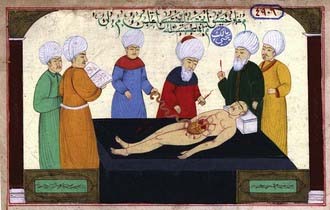
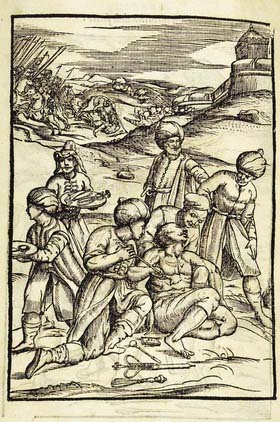
 . Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.)
. Armamentarium Chirurgicum XLIII. Ulm: Balthasar Kühnen; 1655.)