83 Hip and Femur Injuries
• Most hip fractures result from ground-level falls in patients with osteoporosis.
• Patients with intertrochanteric fractures can experience significant blood loss into the thigh and may require fluid or blood resuscitation.
• Hip dislocations and femoral fractures are often caused by high-energy trauma such as motor vehicle collisions and falls from heights; associated injuries are therefore common and should always be looked for.
• Computed tomography is more sensitive than radiography in detecting fractures and can be considered when radiographs appear to be negative and clinical suspicion for fracture is present.
• Emergency physicians may relocate hip dislocations in the emergency department; however, most hip and femoral fractures require orthopedic consultation and operative repair.
Epidemiology
Approximately 300,000 hip fractures occur each year in the United States,1 and this number is projected to increase significantly as the population ages. The major cause of hip fractures is ground-level falls in elderly patients with osteoporosis. Hip injuries are a major cause of morbidity and mortality, especially in the elderly, in whom 1-year mortality after a hip fracture is approximately 25%. Femoral shaft and distal femoral fractures are usually the result of high-energy trauma such as motor vehicle collisions and falls from heights, and thus open wounds and associated traumatic injuries are common.
Pathophysiology
The leading cause of hip fractures is falls in elderly people with underlying osteoporosis. Osteoporosis is a common condition in the elderly, and its incidence increases with advancing age. After about the age of 30, bone resorption slowly begins to exceed bone formation, and as a result bone mass and bone strength lessen. The lifetime risk of fracturing a hip is about 17% in white women and 5% in white men.2
The major cause of hip dislocations is motor vehicle collisions. A great deal of force is required to dislocate a hip, and thus associated injuries are common. Up to 88% of hip dislocations will be accompanied by an associated fracture.3 Patients with hip dislocations have about a 25% risk for osteoarthritis and a 20% risk for avascular necrosis. In addition, sciatic nerve injuries occur in approximately 10% to 14% of patients with posterior hip dislocations.4 These risks may be decreased by prompt diagnosis and treatment in the emergency department (ED).
Osteonecrosis (also known as aseptic necrosis, ischemic necrosis, or avascular necrosis) may be caused by acute disruption of the blood supply to the femoral head as a result of a hip fracture or dislocation. Fractures of the femoral neck can also disrupt the blood supply and result in osteonecrosis. Other causes are sickle cell disease, barotrauma, radiation therapy, chemotherapy, atherosclerosis, and Gaucher disease. Associated conditions include steroid use, excessive alcohol consumption, smoking, connective tissue diseases, pancreatitis, and chronic liver and renal diseases.5 The incidence of osteonecrosis after hip dislocation depends on the degree of trauma involved and the duration of the dislocation. Some data suggest that reduction of the hip within 6 hours after dislocation decreases the incidence of osteonecrosis.6 Therefore, every effort must be made to relocate dislocated hips as soon as possible. Femoral neck fractures are also associated with a high incidence of osteonecrosis. It is thought that the synovial fluid around the fracture site interferes with normal bone healing. Intertrochanteric fractures and other more distal fractures of the femur are rarely complicated by osteonecrosis.
Presenting Signs and Symptoms
Pain is the most common complaint in patients with hip problems.7 The location and character of the pain are very helpful in making a diagnosis. Increased pain during and after weight bearing and improvement with rest suggest a structural joint problem such as osteoarthritis. Constant pain, unrelated to use, suggests an infectious, inflammatory, or neoplastic process.
Diagnostic Testing
Frog-leg views of the pelvis should not be ordered if hip fracture or dislocation is a possibility.
Hip Fractures
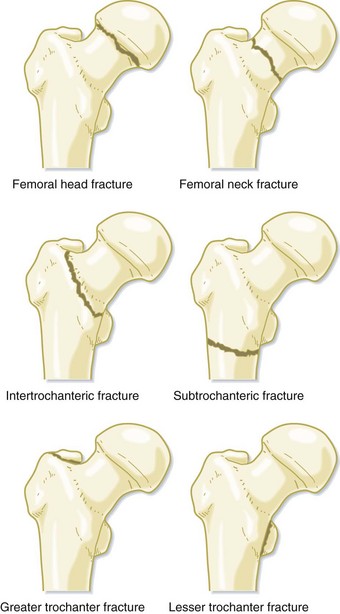
Hip fractures are classified as intracapsular or extracapsular. Intracapsular fractures include femoral head and femoral neck fractures (Fig. 83.1). These fractures are further categorized as either displaced or nondisplaced. Extracapsular fractures include intertrochanteric and subtrochanteric fractures, as well as the less common greater and lesser trochanteric fractures. These fractures can be further categorized by the degree of comminution.
Femoral Neck Fractures
This area of the femur has relatively little cancellous bone and very thin or absent periosteum; in addition, blood supply to the femoral head may be disrupted. As a result, degenerative changes involving the femoral head and frank avascular necrosis are common after these fractures.8
Hip Dislocations
Posterior Hip Dislocations
Several techniques for reducing posterior hip dislocations have been described in the literature. All these methods require adequate sedation and analgesia. The Stimson method requires the patient to lie with the legs hanging over the edge of the bed. This position is seldom practical in a trauma patient, however.4
The Whistler technique involves lying the patient supine on the bed with the knees flexed about 130 degrees.9 An assistant stabilizes the pelvis while the operator stands on the side of the bed near the affected hip. The operator places an arm under the knee on the leg with the dislocation and then grips the top of the other knee. The other hand stabilizes the patient’s ankle. The operator then raises up the arm by using the patient’s knee as a lever in an attempt to relocate the hip. After reduction, the legs are immobilized in slight abduction with a pillow between the knees, and the patient should be sent for radiographs and hospital admission.
Ultrasound-Guided Femoral Nerve Block
Pain relief for hip fractures and femoral shaft fractures can be achieved with ultrasound-guided femoral nerve blocks.10 Contraindications to this procedure include hypersensitivity to the local anesthetic and infections near the injection site. In addition, patients with neurologic deficits in the affected leg or those at risk for compartment syndrome should not have a femoral nerve block performed because it may make it difficult to detect new or worsening neurologic changes. A femoral nerve block is also relatively contraindicated in patients taking anticoagulants or with a bleeding diathesis.
Because high energy is generally required to dislocate a hip, associated injuries are common.11 Ligamentous knee injuries, acetabular and femoral fractures, and sciatic nerve palsies should be considered. If an associated fracture is not clearly seen on plain films, a computed tomography scan should be ordered.
Posterior dislocations are likely to cause a fracture of the inferior aspect of the femoral head and may cause injury to the sciatic nerve.12 Anterior dislocations are associated with fractures of the anterior femoral head and also with vascular injuries.
Hip relocations require procedural sedation in the ED or general anesthesia in the operating room.
![]() Priority Actions
Priority Actions
Hip dislocations are true orthopedic emergencies. Reduction should be done as soon as possible. Reduction within 6 hours reduces the incidence of avascular necrosis.
Significant blood loss is common with hip and femoral fractures, especially fractures in young people, which usually involve a high-energy force. Good intravenous access, fluid resuscitation, and monitoring for blood loss are mandatory.
![]() Red Flags
Red Flags
It is important to look for acetabular fractures before performing closed reduction of a hip dislocation.
On average, patients with femoral shaft fractures lose about 2 to 3 units of blood at the fracture site, and about half of these patients will require blood transfusions.
Hip dislocation or fracture in a young person is strong evidence of serious multisystem trauma.
Christos S, Chiampas G, Offman R, et al. Ultrasound-guided three-in-one nerve block for femur fractures. West J Emerg Med. 2010;11:310–313.
. Fracture dislocations of the hip. In: Wheeless’ textbook of orthopedics (online). Available at www.wheelessonline.com/ostho/fracture_dislocations_of_the_hip
LaVelle DG. Fractures of hip. In: Canale ST, ed. Campbell’s operative orthopaedics. 10th ed. St. Louis: Mosby; 2003:2874–2878.
1 Burge R, Dawson-Hughs B, Solomon D, et al. Incidence and economic burden of osteonecrosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–475.
2 Kannus P, Parkkari J, Sievanen H, et al. Epidemiology of hip fractures. Bone. 1996;18(1 Suppl):57S–63S.
3 Dreinhofer KE, Schwarzkopf SR, Haas NP, et al. Isolated traumatic dislocation of the hip: long-term results in 50 patients. J Bone Joint Surg Br. 1994;76:6–12.
4 Tornetta P, III. Hip dislocations and fractures of the femoral head. 6th ed. Bucholz RW, Heckman JD, Court-Brown CM, et al, eds. Rockwood and Green’s fractures in adults. Philadelphia: Lippincott Williams & Wilkins; 2006;vol. 2:1715.
5 National Osteonecrosis Foundation. Osteonecrosis. Available at www.nonf.org/nofbrochure/nonf-brochure.htm
6 Gurr DE, Gibbs MA. Femur and hip. In: Marks JA, Hockberger RS, Walls RM. Rosen’s textbook of emergency medicine: concepts and clinical practice. 5th ed. St. Louis: Mosby; 2002:643–672.
7 Anderson BC. Evaluation of the adult with hip pain. Available at www.uptodate.com
8 LaVelle DG. Fractures of hip. In: Canale ST, ed. Campbell’s operative orthopaedics. 10th ed. St. Louis: Mosby; 2003:2874–2878.
9 Herwig-Kempers AH, Veraart BE. Reduction of posterior dislocation of the hip in the prone position. J Bone Joint Surg Br. 1993;75:328.
10 Christos S, Chiampas G, Offman R, et al. Ultrasound-guided three-in-one nerve block for femur fractures. West J Emerg Med. 2010;11:310–313.
11 Mirza A, Ellis T. Initial management of pelvic and femoral fractures in the multiply injured patient. Crit Care Clin. 2004;20:159–170.
12 . Fracture dislocations of the hip. In: Wheeless’ textbook of orthopedics (online). Available at www.wheelessonline.com/ostho/fracture_dislocations_of_the_hip