CHAPTER 33 Hinged External Fixators of the Elbow
INTRODUCTION
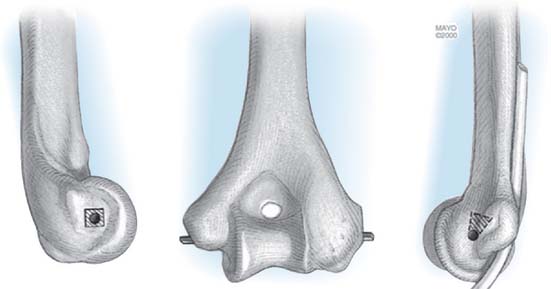
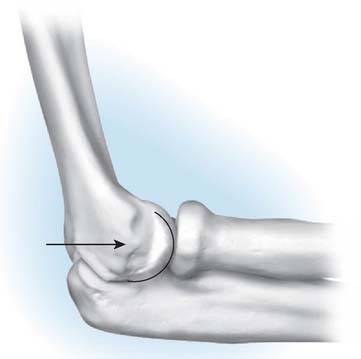
By definition, a dynamic hinged external fixation allows for an axis of rotation to provide elbow stability and motion following trauma or reconstruction.30 With a properly constructed device, the ulna may be separated or distracted from the humerus and still allow physiologic flexion and extension. The mechanics and anatomic landmarks for the application of several fixator devices have been well defined.6,20,28 The axis of rotation of the distal humerus passes through the tubercle of origin of the lateral collateral ligament and through the anteroinferior aspect of the medial epicondyle (Fig. 33-1). Replication of the axis of rotation is essential to avoid pin loosening, persistent stiffness, or instability. In cadaver models, 5 mm of translation or 5 degrees of angulation results in a fourfold increase in resistance to elbow flexion.15
INDICATIONS
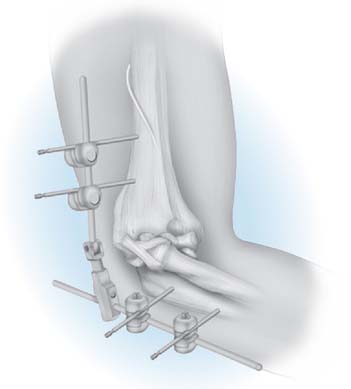
External fixation allows for flexion of the elbow to prevent contracture while still maintaining joint space and appropriate coronal alignment (Fig. 33-2).18 The hinged fixator, when properly applied, maintains a reduced and balanced ulnohumeral joint during motion, thereby protecting repaired or reconstructed collateral ligaments. In trauma, fixators may be used to protect operative fixation of unstable fractures and ligament repair in cases of persistent postoperative instability and for longstanding elbow dislocation or recurrent instability.9 In reconstruction of the elbow, hinged fixators can also be used in the treatment of instability, following ligamentous repair, or with interposition arthroplasty.3,19
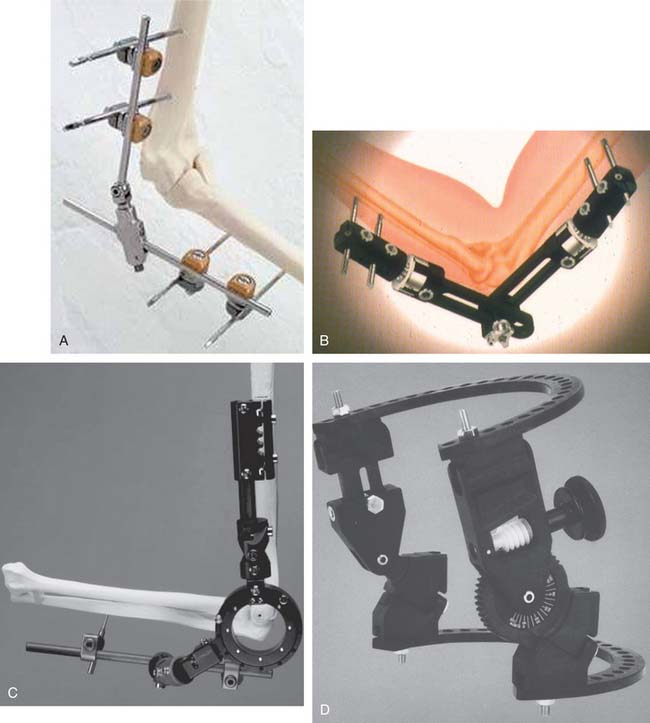
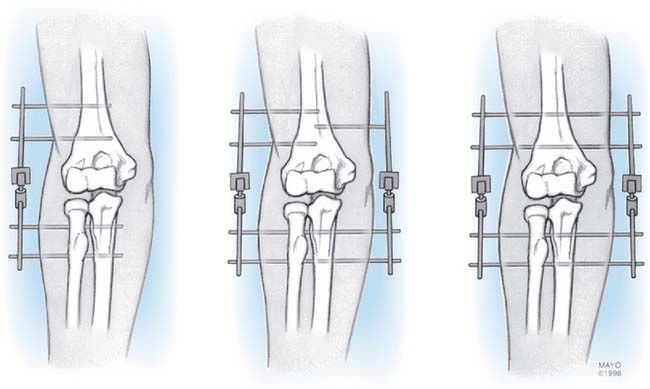
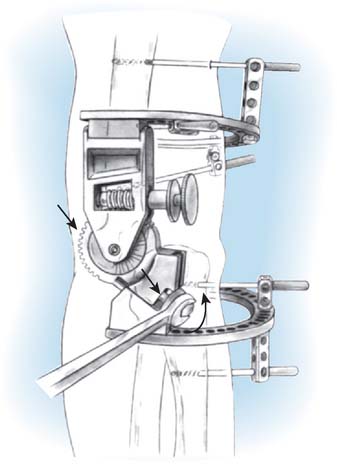
Although goals of treatment may be attained with relatively simple designs, greater flexibility and broader utility have been introduced by Hotchkiss with a more complex fixation. Although several designs are currently available (Fig. 33-3), only the Mayo dynamic joint distractor (DJD)19 and the Hotchkiss Compass Hinge12 are discussed in this chapter because they represent the spectrum from simple to complex.
TRAUMA
Instability
Elbow dislocation with extensive soft tissue injury results in gross instability, even after reduction or repair of involved structures.5 Adjunctive management of late untreated elbow dislocations involve the use of an external fixator.9
Articular Injury (Fracture-Dislocation)
This category includes instability with fractures of the radial head,17,21 some olecranon fractures (Mayo type III)16 as well as Regan-Morrey type II and III coronoid fractures.13,23 Use of a hinged fixator for complex, unstable distal humerus fractures has also been described.7 Open fixation is the primary treatment modality. When gross instability persists or when fixation is deemed vulnerable, an external fixator can be added to allow for immediate postoperative motion and neutralization or unloading of the stresses placed on the fracture fixation (Fig. 33-4).
Residual or Recurrent Subluxation
Residual or recurrent subluxation after simple or complex fracture-dislocation is the third indication for use of a fixator.24 In this setting, percutaneous fixator application can assist in reducing a subluxated joint without having to revert to an open procedure. Maintenance of the device allows for early motion with minimal risk of frank redislocation or continued subluxation. The added stability facilitates proper healing of the capsule and soft tissue restraints.
RECONSTRUCTION
The same basic goals obtain for the use of the fixator after reconstructive interventions.
Ankylosis
When arthrolysis for the post-traumatic joint stiffness is carried out, release of the collateral ligament is sometimes necessary, as well as excision of capsular and bone restraints.8,19 These releases can result in instability. Application of the device protects the repaired collateral ligaments after the arthrolysis while allowing immediate motion of the stabilized concentric joint.
CONTRAINDICATIONS
RELATIVE CONTRAINDICATIONS
SELECTION OF FIXATOR CONFIGURATION
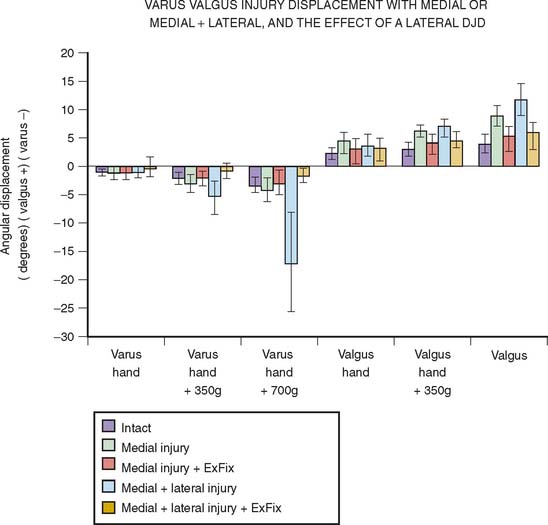
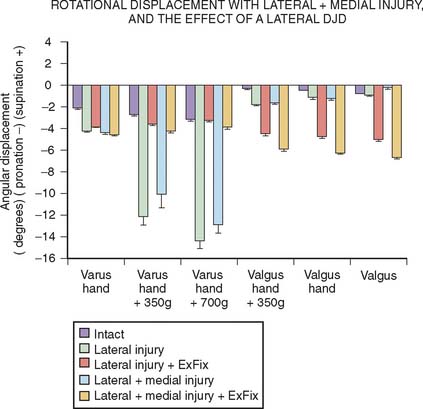
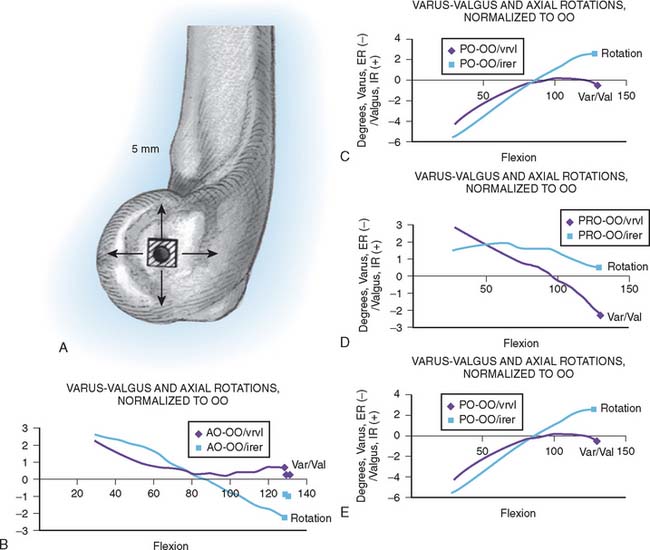
Over the last several years, a number of experiments have been conducted in our laboratory to better understand the function and indications for external fixator configuration. One such assessment demonstrated that compression across the joint with the half-pin lateral application of an external fixator doubles the stiffness of the system in varus load when in extension but had much less effect otherwise. Thus, distraction, one of the recommended applications of the articulated external fixator, does render this system less stable than when the articulation is compressed.27 Of particular importance is the study of Kamineni et al.10 which released the medial and lateral collateral ligaments and assessed the kinematic pattern with a half-pin laterally applied external fixator. In this experiment, it was demonstrated that both varus and valgus stability was restored even with the half-pin lateral configuration and even with up to 7 N out of plane load applied to the forearm (Fig. 33-6). Rotational stability, however, was not as reliably restored (Fig. 33-7). An additional clinical relevant experiment sought to assess the sensitivity of pin placement approximating the axis of rotation. It has been shown that increased energy is needed to move the elbow if a nonoptimum application of the articulated external fixator occurs.15 A subsequent assessment in our laboratory demonstrated that the nonoptimum placement of an external fixator, however, did not alter the kinematics as much as had been anticipated (Fig. 33-8). Based on these data, it was concluded that a slight proximal placement of the axis of the external fixator actually enhances the rigidity of the elbow in a manner that would favor reconstruction of the lateral ulnar collateral ligament. Thus, there may be instances in which slight nonanatomic axis placement is clinically acceptable.2
TECHNIQUE
MAYO DYNAMIC JOINT DISTRACTOR
Author’s Surgical Technique
The patient is supine with a sandbag under the scapula, and a nonsterile tourniquet is applied. The arm is draped free and brought across the chest. In most cases of trauma or reconstruction, a posterior skin incision is used and the elbow joint is exposed either medially or laterally according to the pathologic condition being addressed.
Applying the DJD II External Fixator
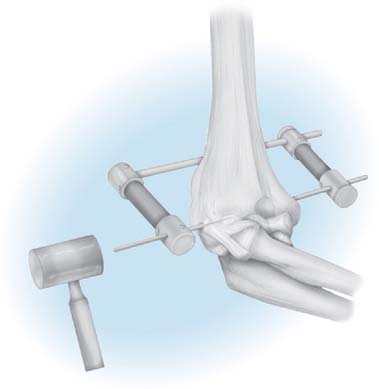
Once the elbow has been exposed and the pathologic condition addressed including collateral ligament repair/reconstruction, the external fixator is applied. Several possible configurations are available and are used depending on the lesion and surgeon preference (Fig. 33-9). As noted earlier, we employ the lateral half-pin configuration almost exclusively today.
AXIS IDENTIFICATION
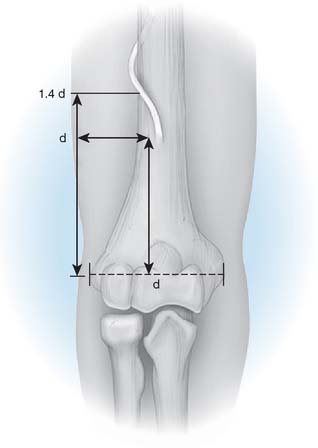
The essential landmarks of the flexion axis are identified. On the lateral aspect of the capitellum, a tubercle is present at the site of origin of the lateral collateral ligament, which represents the geometric center of curvature of the capitellum (Fig. 33-10).
On the medial aspect of the distal humerus, the axis of rotation lies just anterior and inferior to the medial epicondyle. This corresponds to the center of curvature of the medial contour of the trochlea and is the locus of the humeral origin of the medial ulnar collateral ligament (Fig. 33-11).
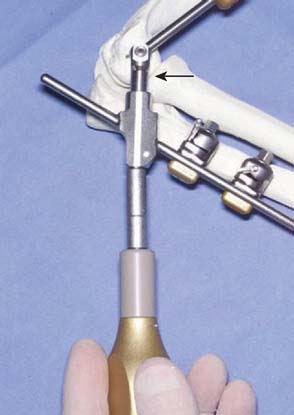
AXIS STYLUS
HUMERAL PIN INSERTION
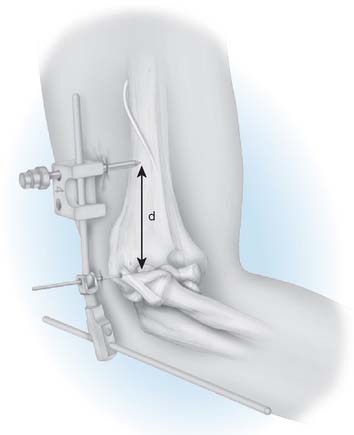
FIGURE 33-15 A cannula is inserted through the pin guide and protects the soft tissue with the placement of the threaded pin.
Ulnar Pin Insertion
DISTRACTION
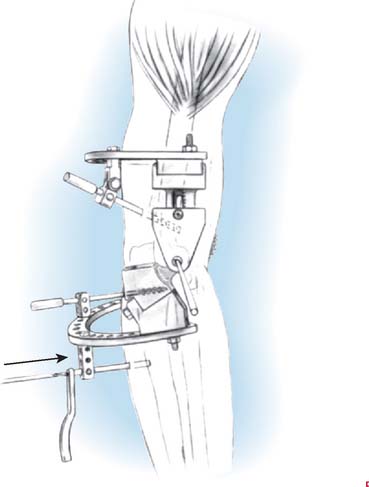
Percutaneous Application
For some acute or subacute fractures in which the elbow is unstable due to coronoid deficiency, there is a tendency for the ulna to sublux posteriorly. In these cases, the dynamic joint distractor may sometimes be applied percutaneously under fluoroscopy to neutralize fracture displacement forces (Figs. 33-19 and 33-20). Full motion may be achieved by this slight asymmetric distraction, but a flexion arc of 60 to 90 degrees of motion is usually attainable and this is considered adequate given the specific goals of this application.

FIGURE 33-20 In a manner similar to the open condition (see Fig. 33-14), the key is to place the proximal pin at a distance “D” from the axis pin, which is a safe distance from the radial nerve. The use of the trochar further minimizes the likelihood of injury to the radial nerve. The pins are placed distally in the ulna to avoid the plate.
THE COMPASS HINGE
Frame Assembly
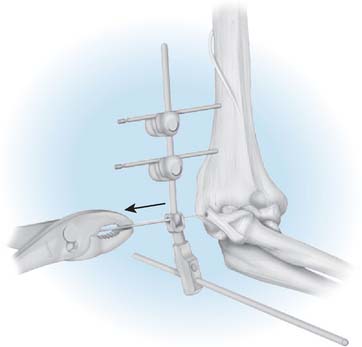
When the frame has been assembled and appropriately adjusted, it should slide along the axis pin without significant impingement or resistance (Fig. 33-21). If there is resistance, the components are probably out of alignment. The clinician should make sure to allow for swelling in the postoperative period, allowing at least 2 cm of clearance from the skin to the hinge block at the time of surgery.
Patient Positioning
For release of contracture and removal of heterotopic bone, the patient should be placed in the supine position, with the arm on a radiolucent hand table. If the patient first requires a more extensive exposure of the distal humerus for fracture or reconstructive work, it may be useful to begin the operation with the arm over the chest when using one of the more standard posterior approaches to the elbow, either olecranon ostectomy or a triceps sparing exposure (Bryan-Morrey). In cases of gross instability, the prone position can be used, with the added benefit that gravity in this position tends to reduce the joint during hinge placement and operative ligament repair or reconstruction. However, exposure of the coronoid is difficult in the prone position.
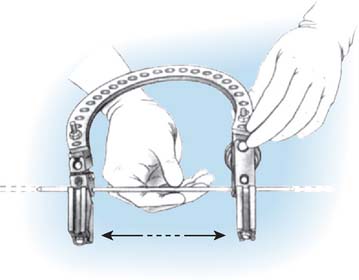
Axis Pin Placement
As with the dynamic joint distractor, a single temporary axis pin is placed across the joint, or two half-pins can be inserted, one from the medial and the other from the lateral aspect. The alignment of the axis is crucial. It is important to take the time necessary to achieve perfect placement of this pin for alignment of the Compass Hinge at the elbow. Both an anteroposterior and lateral radiograph should be viewed to ensure adequate placement. Once the two pins are coincident, entering at their respective centers of rotation, the frame should still be easy to slide from medial to lateral, back and forth, before securing the axis pin from the medial side (Fig. 33-22).
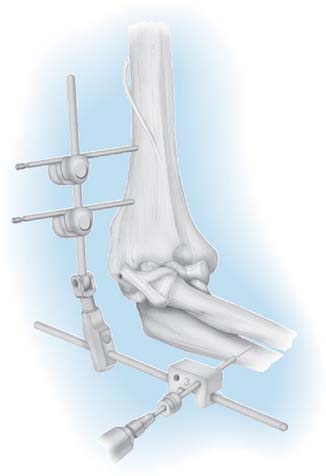
Humeral Pin Placement
The lateral pin is usually placed using a two-hole post and a single-hole Rancho cube. The lateral flare of the humerus is used for placement. The drill guide rests on the lateral supracondylar ridge, directed anterior and distally. The radial nerve, at this level, is anterior to the pin (Fig. 33-23). Humeral fixation and alignment of the axis of the hinge must be achieved before fixation of the ulna.
Placement of Ulnar Fixation
One 5-mm and one or two 4-mm pins are used in the ulna. The more proximal pin (5-mm) provides optimal control of the joint and is placed from the dorsal surface through the coronoid. The smaller (4-mm) pins are used more distally in the ulna, again from the dorsal surface. If the elbow is grossly unstable, it is quite important to reduce the elbow by placing it in approximately 90 degrees of flexion when applying the ulnar fixation. Once the joint is reduced and held in position, the first two proximal ulnar pins can be placed. After this, ranging through flexion and extension and ensuring reduction of the joint is important. If there is a tendency for the elbow to subluxate, then alignment has not been achieved and the bolts must be loosened and reduction achieved (see Fig. 33-23).
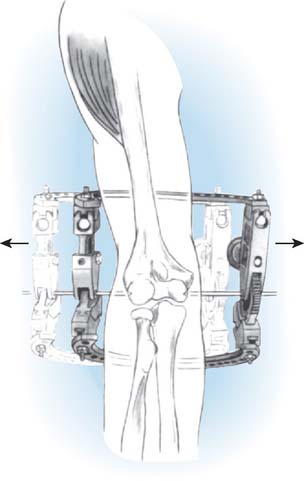
Application of Distraction
After the joint has been reduced and all pins applied, distraction can then be applied to the system through the distraction mechanism. Distraction is achieved by turning the bolts located on the ulnar ring fixation blocks (Fig. 33-24). Both sides of the hinge should be distracted an equal amount. Use and extent of distraction should be done at the discretion of the surgeon.
Aftercare
For the DJD II, the patient is placed in a continuous motion machine for 21/24 hours a day (see Chapter 10).
After reconstructive procedures, the patient returns approximately 3 weeks after dismissal from the hospital, the distraction device is removed, and the elbow is examined under general anesthesia. The arc of motion obtained at surgery is re-established under anesthesia. Care is taken not to forcefully manipulate the elbow, but some sense of the firmness of the end points of motion is determined, because this is believed to have prognostic value. Joint crepitus and stability are also assessed. We have encountered virtually no problems with this assessment.1
Splints
For patients treated for arthrolysis, static adjustable splints are employed when the device is removed, usually at about 3 weeks for stiffness and 4 to 6 weeks after fracture (see Chapter 11). The goal is to attain a degree of soft tissue stretch with a constant force allowing the soft tissue to “relax” under the constant pressure. For the first 3 weeks of application, the patient wears one or the other for approximately 20 to 21 hours a day. After 3 weeks, the program is individualized, with the time in the splint decreasing to 10 to 16 hours, but the basic principles continue to be followed. For release of the stiff elbow, splint usage may be required at night and to maintain motion for up to 3 months or occasionally even up to 6 months.
Fixator Removal and Examination Under Anesthesia
If progress is not being achieved with the splints and there is no concern about fracture displacement, additional examination under anesthesia may be performed. If this is to be done, this is accomplished before 3 months. The most recent radiograph should be available to appreciate the specific pathologic lesion being addressed. We have evaluated the effectiveness of 56 “evaluations,” 30 of which occurred at the time of external fixator removal. A mean of 37 degrees improvement in the flexion arc was documented. There were no fractures or any other notable complications.1
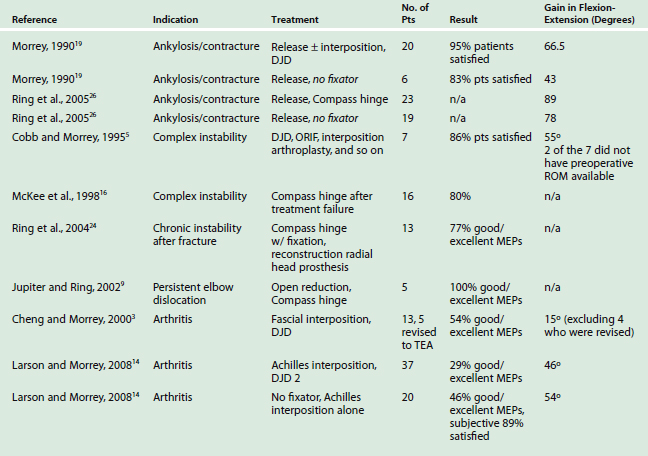
RESULTS
A summary of the literature organized by documented indications is shown in Table 33-1. For most surgeons, the value of these devices is in the management of trauma and its sequelae (Fig. 33-25) (also see Figs. 33-4, 33-19, and 33-20).16,17 Surgical indications for hinged fixator use include ankylosis or elbow contracture, acute or chronic elbow instability, or arthritis.
Elbows treated for ankylosis or contracture respond well to release, with mean flexion arc gains of 40 to 80 degrees.19,25 In a series of 26 patients, Morrey initially reported greater patient satisfaction and elbow range of motion following arthrolysis with the use of a hinged external fixator compared with no fixator.18 A retrospective series of 42 patients reported by Ring et al.,25 however, showed no significant advantage in postoperative range of motion with the use of external fixator and capsular release when compared with capsular release alone for the treatment of elbow contractures. Demographics and injury characteristics were similar between the two groups, but in the latter group, the plan was to specifically use the fixator (Compass) as an adjunct to improving motion.
External fixators have also been described in the treatment of complex instability with approximately 80% patient satisfaction or satisfactory Mayo Elbow Performance scores.5,16,24,26 Jupiter and Ring report successful results in five out of five patients treated for long-standing unreduced elbow dislocations.9 In a complex patient population with joint subluxation and coronoid deficiency, Papandrea et al.22 were not able to demonstrate the value of the external fixator as an adjunct to the complex management in these complex injuries treated at the Mayo Clinic.
For post-traumatic or inflammatory elbow arthritis, the literature contains several reports of external fixators used in conjunction with débridement, capsular release, or interposition arthroplasty.3,14 A series of 13 patients undergoing fascial interposition arthroplasty in conjunction with distraction by the Dynamic Joint Distractor documented in 54% good or excellent Mayo Elbow Performance (MEP) scores.3 Recently, we reported a series of 57 patients undergoing Achilles tendon interposition arthroplasty, 37 with placement of the Dynamic Joint Distractor II and 20 with no use of a fixator. Only 29% of patients in the external fixator group had good or excellent MEP score.14 From the 20 patients without the use of an external fixator, 46% had good/excellent results.14 However, there were strong selection bias to use the fixator in the more difficult cases. Of note, the more unstable elbows were more likely to be placed in an external fixator after operative reconstruction, and instability has independently been shown to be a predictor of poor outcomes following interposition arthroplasty.3,14 Nonetheless, there was no statistical association between clinical outcomes and use of an external fixator.
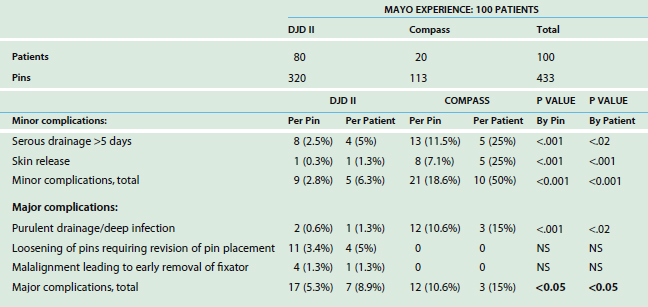
COMPLICATIONS
This topic has recently been studied by Cheung et al.,4 who reviewed the Mayo experience with 100 consecutive applications of 80 DJD II and 20 Compass fixators. The complications documented to be associated with these respective devices are listed in Table 33-2. These include superficial or deep infection, skin irritation, nerve injury, pin loosening, fracture, and pin breakage. There are statistically significant differences in the complication rate, which is greater with the use of the more complicated Compass device.4 Difference in the frequency of these complications relate to a number of factors, including the indications for application and possibly from technical difficulties encountered. No reoperations were required in any patient for pain-related problems.
INFECTION
Soft tissue pin site infection or irritation is a minor problem and is readily treated by pin removal. In the Mayo retrospective assessment of 433 pins in 100 patients, 11 pins loosened (2.5%), 13 pin sites resulted in deep (not osseous) infection (3%), and 21 pin sites (5%) had redness and nonpurulent drainage managed with oral antibiotics.3 Transarticular pins used in the early external fixator designs were a concern, because infection at that site can cause a deep infection of the joint, resulting in treatment failure. Although deep infection may occur, it should be noted that these largely occur in the post-traumatic patient population, who is generally at a higher risk of infection due to previous instrumentation or open contamination of the fracture or elbow than the general adult population. Nonetheless, the current designs of external fixators eliminate a permanent articular pin, which should certainly reduce the frequency of intra-articular infection.
NEURAL INJURIES
The incidence of neural injury relates to the underlying pathologic condition, to the surgical approach, and to the surgeon’s skill and care in the use of the device. A posterior interosseus nerve palsy that subsequently recovered has been attributed to placement of the proximal ulnar half-pin with the forearm pronated.29 In our experience with 100 applications using 433 pins, there have been no cases of direct nerve injury applicable to the device.4 The ulnar nerve may certainly be irritated from increased motion after arthrolysis. If it is tethered or compressed, the additional motion, especially in flexion, causes nerve entrapment and compression that occasionally requires a decompressive procedure.
SUMMARY
The external fixator is an important tool in the elbow surgeon’s armamentarium, although its precise role in a variety of pathologic conditions is still being defined. The protective effect and ability to replicate elbow kinematics has been experimentally verified.2,11 Clinically, the fixator is a useful augment to reconstruction in cases of complex instability and interposition arthroplasty. Several designs of hinged external fixators are currently available, each with strengths and deficits. Although a low rate of significant pin site complications have been reported, meticulous technique and appropriate monitoring of pin sites is essential to achieving safe, successful results from an external fixator.
1 Araghi, A., Celli, A., Adams, R., and Morrey, B. F.: The effect of examination under anesthesia on the stiff elbow following surgical release. (Submitted for publication).
2 Baumfeld, J. A., Morrey, B. F., van Riet, R. P., Neale, P. G., O’Driscoll, S. W., and An, K. N.: The effect of malpositioning of a hinged elbow external fixation device (In preparation).
3 Cheng S.L., Morrey B.F. Treatment of the mobile, painful arthritic elbow by distraction interposition arthroplasty. J. Bone Joint Surg.. 2000;82B:233.
4 Cheung, E. V., O’Driscoll, S. W., and Morrey, B. F.: Complications of hinged external fixators of the elbow. J. Shoulder Elbow Surg. 2008 Epub Feb 27.
5 Cobb T.K., Morrey B.F. Use of distraction arthroplasty in unstable fracture dislocations of the elbow. Clin. Orthop. Rel. Res.. 1995;312:201.
6 Deland J.T., Gerd A., Walker S.P. Biomechanical basis for elbow hinge-distractor design. Clin. Orthop. Rel. Res.. 1987;215:303.
7 Hall J., Schemitsch E.H., McKee M.D. Use of a hinged external fixator for elbow instability after severe distal humeral fracture. J. Orthop. Trauma. 2000;14:442.
8 Hertel R., Pisan M., Lambert S., Ballmer F. Operative management of the stiff elbow: Sequential arthrolysis based on a transhumeral approach. J. Shoulder Elbow Surg.. 1997;6:82.
9 Jupiter J.B., Ring D. Treatment of unreduced elbow dislocations with hinged external fixation. J. Bone Joint Surg.. 2002;84A(9):1630.
10 Kamieni, S., Ankem, H., and Amis, A.: A safe normalized parameter for lateral distal humeral pin insertion. (Accepted for publication, Clin Anat, 2007).
11 Kamineni S., Hirahara H., Neale P., O’Driscoll S.W., An K-N., Morrey B.F. Effectiveness of the lateral unilateral dynamic external fixator after elbow ligament injury. J. Bone Joint Surg. Am.. 2007;89:1802.
12 Kasparayan N.G., Hotchkiss R.N. Dynamic skeletal fixation in the upper extremity. Hand Clin.. 1997;13:643.
13 Koslowsky T.C., Mader K., Siedek M., Pennig D. Treatment of bilateral elbow dislocation using external fixation with motion capacity: A report of two cases. J. Orthop Trauma. 2006;20:499.
14 Larson, A. N., and Morrey, B. F.: Interposition arthroplasty with an Achilles tendon allograft. AAOS, San Diego, CA, 2007 (accepted for publication).
15 Madey S.M., Bottlang M., Steyers C.M., Marsh J.L., Brown T.D. Hinged external fixation of the elbow: optimal axis alignment to minimize motion resistance. J. Orthop Trauma. 2000;14:41.
16 McKee M.D., Bowden S.H., King G.J., Patterson S.D., Jupiter J.B., Bamberger H.B., Paksima N. Management of recurrent, complex instability of the elbow with a hinged external fixator. J. Bone Joint Surg.. 1998;80B:1031.
17 Morrey B.F. Complex instability of the elbow. J. Bone Joint Surg.. 1997;79A:460.
18 Morrey B.F. Distraction arthroplasty: Clinical applications. Clin. Orthrop. Rel. Res.. 1993;293:46.
19 Morrey B.F. Post-traumatic contracture of the elbow: Operative treatment including distraction arthroplasty. J. Bone Joint Surg.. 1990;72A:601.
20 Morrey B.F., Chao E.Y. Passive motion of the elbow joint. J. Bone Joint Surg.. 1976;58A:501.
21 Morrey B.F., Chao E.Y., Hui F.C. Biomechanical study of the elbow following excision of the radial head. J. Bone Joint Surg.. 1979;61A:63.
22 Papandrea R.F., Morrey B.F., O’Driscoll S.W. Reconstruction for persistent instability of the elbow after coronoid fracture-dislocation. J. Shoulder Elbow Surg.. 2007;16:68.
23 Regan W., Morrey B.F. Fractures of the coro-noid process of the ulna. J. Bone Joint Surg.. 1989;71A:1348.
24 Ring D., Hannouche D., Jupiter J.B. Surgical treatment of persistent dislocation or subluxation of the ulnohumeral joint after fracture-dislocation of the elbow. J. Hand Surg.. 2004;29:470.
25 Ring D., Hotchkiss R., Guss D., Jupiter J. Hinged elbow external fixation for severe elbow contracture. J. Bone Joint Surg.. 2005;87A:1293.
26 Ring D., Jupiter J., Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J. Bone Joint Surg.. 2002;84A:547.
27 Sekiya H., Neale P.G., O’Driscoll S.W., An K.N., Morrey B.F. An in vitro biomechanical study of a hinged external fixator applied to an unstable elbow. J. Shoulder Elbow Surg.. 2005;14:429.
28 Tomaino M.M., Sotereanos D.G., Plakseychuk A. Technique for ensuring ulnohumeral reduction during application of the Richards compass elbow hinge. Am. J. Orthop. 1997;26:646.
29 Tomaino M.M., Sotereanos D.G., Westkaemper J., Plakseychuk A. Posterior interosseous nerve palsy following placement of the compass elbow hinge for acute instability: a case report. J. Hand Surg. 1999;24A:554.
30 Volkov M.V., Oganesian O.V. Restoration of function in the knee and elbow with a hinge-distractor apparatus. J. Bone Joint Surg. 1975;57A:591.