CHAPTER 69 High lateral tension abdominoplasty
History
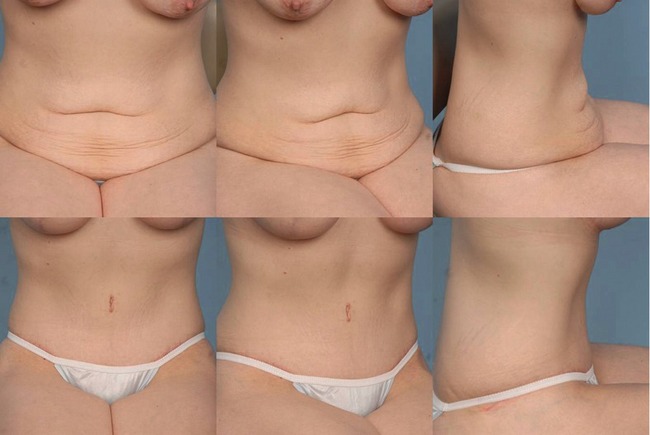
The HLT is not just an abdominoplasty; it is a powerful lower body lifting procedure, creating improvement not just of the abdomen, but to the mons, inguinal region, proximal thighs, and even the buttocks. Even posture can be improved (Figs 69.1, 69.2).
Physical evaluation
• Vertical skin laxity: The signatures of the high lateral tension abdominoplasty is to place the highest tension on the lateral portion of the incision, such that the central third of the incision is nearly in apposition after closure of each lateral third. This often means that the old umbilical site does not get excised, leaving a vertical scar from its closure. While this usually heals well, and accepting the presence of this scar may be considered part and parcel with being a true HLT “purist”, this scar does not always heal perfectly, and many patients and surgeons indeed do want to avoid it. There are occasions preoperatively when the surgeon cannot be certain as to whether the old site will be able to be excised, without tension but if there is any question, the patient should be warned that there are three choices: proceeding with a classically marked HLT and accepting that vertical scar if it is necessitated for proper skin tension of excision intraoperatively, perhaps locating the entire incision more superiorly in order to increase the likelihood of getting out the old umbilical site, or simply not doing an HLT, but resecting as much tissue as necessary centrally in order to remove the site, even if this means distorting or raising the height of the mons.
• Extent of skin laxity: Many patients today ask for a “mini” tummy tuck, wanting the horizontal extent of the incision to be as short as possible, perhaps even as narrow as their C-section scar. It is rare to find women whose laxity is so centrally located that such a short scar removes all of the laxity that is troubling to the patient while creating a smooth contour to the abdomen, and the patient should always be evaluated sitting upright, as this demonstrates the extent to which the laxity extends laterally. Patients can understand that if the laxity extends to the mid-axillary line that an incision the width of her previous C-section will fail to correct the lateral laxity. Even compared to the standard abdominoplasty, the HLT does require a wider incision. That is because the standard tummy tuck is essentially an exercise in “excising the umbilicus”; the width of the incision is determined according to one parameter: how much is necessary to remove that vertical excess without creating a dog-ear. But the HLT considers that lateral excess the most important area for excision. By pulling down and out laterally, a greater degree of flattening of the epigastrium occurs than pulling simply straight inferiorly. This can easily be demonstrated to a patient by creation of downward tension on the epigastrium by pinching between the umbilicus and just above the mons, and contrasting that with the greater improvement that occurs to the epigastrium by simultaneously pinching lateral, angled down and out, so that the epigastrium is being pulled in two directions. The greatest laxity on the trunk of the post-partum or weight loss patient is also laterally, so this area needs the greatest amount of excision.
• Skin quality and texture: Just like with a mastopexy, after skin is removed, the same skin that stretched once and was damaged remains behind. The ultimate quality of the result and appearance will be based upon the patient’s own skin, for which we have little if any control. It is important to asses the skin in order to give the patient expectations as to what their particular outcome is likely to be. Do stretch marks still exist superior to the likely line of resection so that many will remain, or are they likely to all be excised? Is the skin thin and/or sun-damaged, likely to reloosen to a significant degree or have notable lines or wrinkles? These issues must all be addressed with the patient preoperatively in order to set their expectations, and patients should further realize that there is no preoperative test that can predict how their particular skin will hold up after surgery; the best a surgeon can do is offer them an educated guess. The presence of pre-existing abdominal scars must be assessed as they may have affected blood supply in such a way so as to necessitate modification of the HLT design, or to limit undermining even more than usual. Occasionally the scar is adherent to the underlying abdominal wall and consideration needs to be given to whether the scar needs to be freed to allow transfer of tightening forces beyond it, or whether such a maneuver would compromise blood supply. There are also sometimes transverse lines of adhesion, usually between umbilicus and xyphoid between the midline and the anterior axillary line that prevent transference of pull from the abdominoplasty to the tissues cephalad to it. It can take substantial undermining to free these up, and in doing so the blood supply to the flap can be compromised. These issues need to be discussed with the patient preoperatively.
• Excess fat within flap: The HLT allows for safe suctioning of the abdominoplasty flap. The flap should be evaluated not just for the presence of significant subcutaneous fat, but for the extent to which this fat is proportional to the patient’s overall body habitus. Most important is noting the thickness at the expected level of flap transection relative to where that tissue will be sewn inferiorly. It is frequently much thicker superiorly, and liposuction of the flap should be considered to create a smooth transition. I tend to suction abdominaplasty flaps only occasionally. The patient population I predominantly see is thin. Moreover, though liposuction of the flap can be done safely, it does seem to increase the likelihood of seroma formation and prolong recovery.
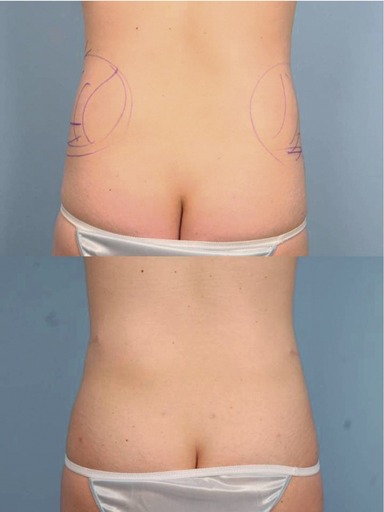
• Excess fat in contiguous areas: When a patient seems to have a large amount of fat in their abdominal flap, there is usually an even greater amount of fat in the pubic area or the posterior iliac crest area. Too much is made of liposuctioning of abdominal fat within the flap. Oftentimes, there is not enough to remove to make a significant difference in the appearance. Usually, the hips contain substantially more fat in proportion to the abdomen. If there is a lot to remove in the abdomen, there is usually more in the hips or the thighs, and it is important to look at those areas and consider treating them, lest the surgeon create a disharmonious proportion. With the abdomen flattened from an abdominoplasty, the width that results from excess hip fat can be very apparent. In fact, by tightening the abdomen, the width of the hip area can appear to increase following an abdominoplasty (Fig. 69.3). Narrowing the waist through suction of the posterior hip roll can dramatically improve the appearance of the abdomen. Similarly, excess fat in the mons area is often not noted preoperatively. Either the abdomen may be protuberant or there may be tissue overhanging the waist. After a smooth and flatter abdomen, the mons can protrude in clothing and be disconcerting. This can be treated with liposuction at the time of abdominoplasty and this area should be assessed for this preoperatively.
• Rectus diastasis/hernia: The patient should be examined standing, sitting, and laying back flat while raising her shoulders up, as in doing a partial sit-up. This is a good way to test for a rectus diastasis. From this position, one can take the patient’s hands and show them the gap that exists between their muscles. Some patients will comment that they need “to work out more.” But they need to be reassured that exercise will only increase the strength of the muscles; only surgery can bring them back together. I always discuss with patients that they have an option of whether or not to plicate any diastasis. While the plication can substantially improve the outcome, so too does it lengthen the recovery and make it more uncomfortable. The umbilicus is always assessed for the presence of a fascial defect that may need to be repaired either separately or at the time of abdominoplasty. The patient should also be examined in profile with her arms at her sides and above her head, asking her to allow her abdominal musculature to relax. During plication, it is all too tempting to tighten her as much as possible from pubis to xyphoid; more important is to assess the patient’s laxity and preplan where the abdomen needs to be tightened to create the most attractive contour.
• Intra-abdominal fat: Pressure from the internal organs including intra-abdominal fat puts pressure on any repair that is done of the rectus diastasis. While it is possible for there to be relapse in any situation, this is certainly exacerbated in cases in which there is the greatest degree of intra-abdominal fat. This is important because it might weigh on your choice as to whether or not there is enough of a benefit from plication to make it worth the additional recovery. Also, it helps to warn patients about an increased possibility of the repair loosening and restretching with time.
Anatomy
The skin/adipose layer
It also must be appreciated that there is both horizontal and vertical excess of the skin/subcutaneous fat layer. The horizontal scar of an abdominoplasty obviously reduces the vertical excess, but what about the horizontal excess? Usually the body is wider at the height of the lower abdominoplasty incision than it is at the upper abdominoplasty incision, so that when the edges are closed, the horizontal excess is apparently eliminated. But there is not a significant change in width of the abdomen from the level of the xyphoid down to about the level of the umbilicus; in fact, the body often narrows. What this means is that the tissue that is transferred down from the upper to the mid-abdomen during a tummy tuck develops even greater horizontal laxity when a traditional abdominoplasty is done, as the incision is relatively parallel to the ground and the greatest pull is straight inferiorly. But with the HLT, the lateral limbs of the final closure diverge superiorly in an oblique direction, and they hold the greatest amount of tension. This serves to excise that horizontal redundancy in the epigastrium, thereby flattening it and significantly improving the abdominal contour.
Technical steps
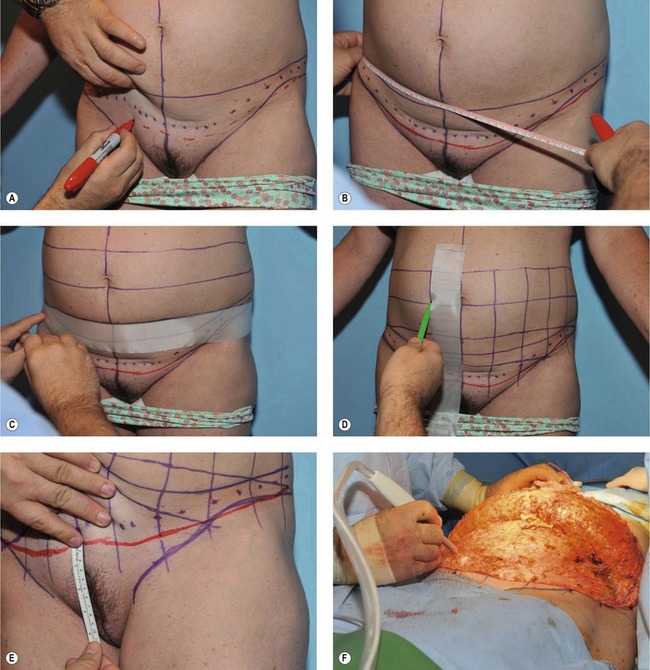
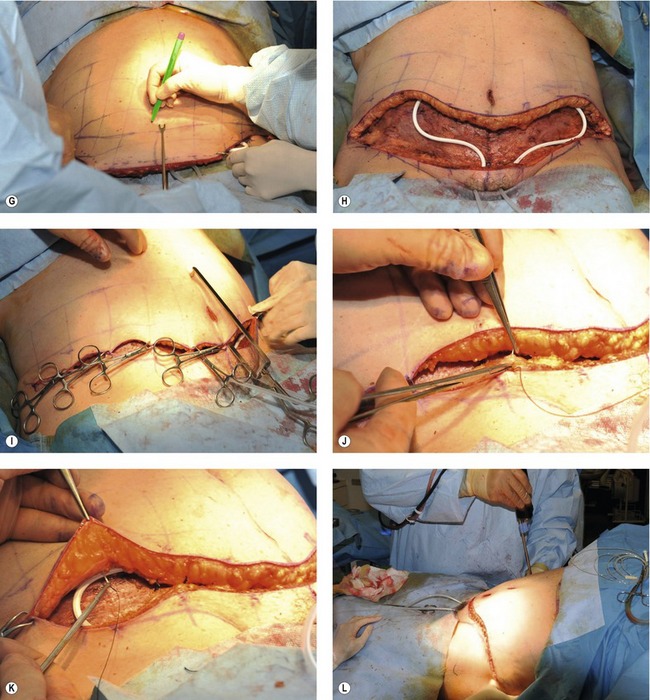
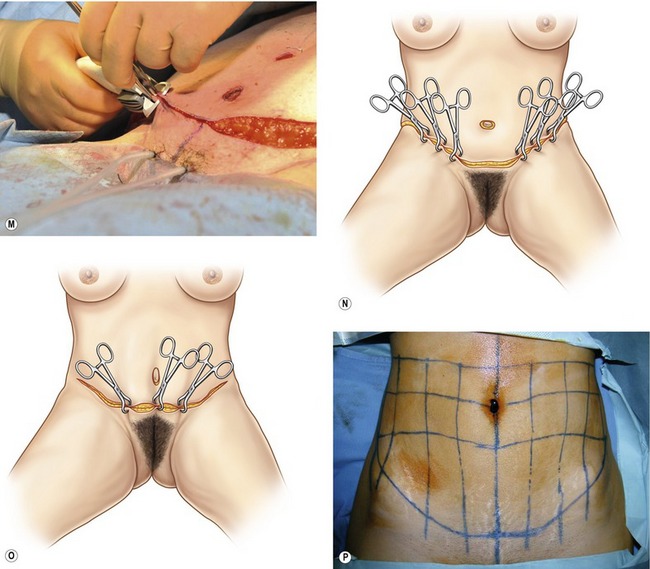
Fig. 69.4 A, The outline of a typical pair of the patient’s panties is drawn. Then the proposed final scar location is drawn (as shown here by the dotted blue line). With the pen held at the level of that line, the skin is pushed cephalad with the expected amount of tension on the closure at that area to determine where the initial incision must be made for the final scar to end up at that dotted line. B, The patient is marked, measured, and checked multiple times for symmetry. C, I have found it difficult to draw straight lines while holding a tape measure flat against the body; use of 2-inch tape has facilitated the ability to draw straight lines. D, Using the tape to checkerboard the stomach greatly facilitates drawing even lines of resection intraoperatively and makes final closure more precise. E, There should be about 7 cm of hairbairing skin on stretch above the anterior vulvar commissure. F, The PlasmaJet used to paint the entire raw surface, reducing bleeding and sealing lymphatics, thereby reducing the time a drain is necessary and reducing the likelihood of seromas. G, The Lockwood D’assumpco clamp is used to mark the extent of resection. It is critical to pull on the flap in the direction that it will be closed and with the amount of tension that you wish to put on that part of the flap. There is less tension placed centrally, as high tension would distort the mons. More tension is used laterally. After hash marks are made with the table flexed at about 30 degrees, the patient is laid flat, and the final resection line is made, using the checkerboard to assess symmetry. H, Final resection. Note not just the obviously greater resection laterally than centrally, but that in fact the lateral resection is just a bit more than the central resection (see resection relative to original preoperative horizontal line from the preoperative markings). Also note that even the upper line seems to drop inferiorly centrally, while the more lateral part of what was once a horizontal line rises up laterally. This is part of the confusion of the HLT. While in fact there is more taken laterally than centrally, it is only a bit more, not a lot more. Most of what appears to be a greater amount taken laterally is really due to the way the tissue is adherent to the deeper structures. I, The vertical lines are extremely helpful in arranging a speedy and well-aligned closure. Note the umbilicus marking clamp; the deep side of the clamp is around the umbilical stalk, and the other side can be used to mark exactly where that is transferred to the front. J, It is important for the closure to incorporate a sturdy bite of the cut edge of the SFS. The layer is always more stout in the inferior cut edge than the superior edge. It tends to retract a significant degree in the central third of the abdomen, and one needs to really. K, Though usually less obvious than in the inferior edge, there is a prominent SFS in the superior flap. #1 Nurolon soaked in Betadine is used to make a tight deep closure, taking all the tension off of the skin. L, Liposuction is performed at the end of the incision to reduce dog-ear and bulk in all but the thinnest of patients. The extreme lateral tension requires that the incision be lengthened, but even with that, there still tends to be a thickening at the waist if the extra fat is not removed. M, The Insorb subcuticular stapler has reduced closing times and made the wound edges more evenly approximated. Because of the double Adson forceps, it can help to smoothly redistribute mismatches in lengths of the two flaps. Reducing operative time is an important part of reducing DVT and PE risk, and the fact that scars are at least as good with this as with sutures argue strongly for its adoption. N, With the HLT, the greatest tension is lateral. When it is closed, the incision above the pubic area almost comes together without a clamp in the area. This maximally rejuvenates the thighs as well as the epigastrium, applying an oblique angle of tension to the epigastrium from each limb. The incision angles up more than a standard abdominoplasty in the lateral area, and it also extends wider into the flank in order to not have a dog ear from the large lateral resection and tension that is thereby created. O, Closure with a traditional abdominoplasty pulls most of the tension centrally. The only improvement to the epigastrium is that which occurs from the straight downward tension, and there is no oblique lines of tension pulling on the thighs and epigastrium as there is with the HLT. P, This patient is lying supine. The horizontal lines were drawn straight with a laser level, yet they are pulling up somewhat from the midline. Once the flap is released along the lower incision, this happens to an even greater extent, thereby accentuating the perception of the extent of lateral tension. In reality, the resection is often only a little bit more laterally than centrally with an HLT (blue line). But with a standard, the surgeon is usually focused on just “getting out” the old umbilical site, and the length of the incision is that which is dictated to close it without skin redundancy (green line). Therefore, the standard usually does not have as wide of an incision as does the HLT. Though the HLT resection drawn in blue here was able to be done on this patient, the HLT frequently results in non-excision of the umbilicus. So long as there is sufficient lateral tension, there will not be laxity and redundancy in the epigastrium. One must be diligent about creating adequate lateral tension, and be willing to extend the incision as far laterally as necessary to accomplish this.
Photography should be done in a complete and consistent manner. All patients should have photos of the entire aesthetic area from the shoulder to knee. Sometimes when the view is too cropped, the effect of the result on the patient’s overall physique is not as noticeable as when there is a wider view. Images should be taken both AP and PA, both laterals, and all four obliques. Photos should always be taken with the patient sitting, particularly if the patient is thin and there is not significant skin redundancy appreciated when standing (Figs 69.5–69.7). Frankly, the abdomen always looks much worse in a seated photo, but this is a position in which we spend much of our lives, and the exaggeration of abdominal redundancy noted in this position must be reckoned with. The photos do not just force the surgeon to notice everything relevant to the surgery and act as a basis for discussion with the patient, but they serve a critical role of demonstrating for the patient the rationale for the surgery down the road should they question the width of the scar or the extent of improvement. Standardized photos can do much to allay patient concern and anxiety. The recovery from the procedure is long and there are often times in which a patient asks themselves whether it was worth it; seeing the original picture can be very helpful for them. If the scar ends up wide or thick, the photos can remind the patient that the scar is less problematic than their laxity.
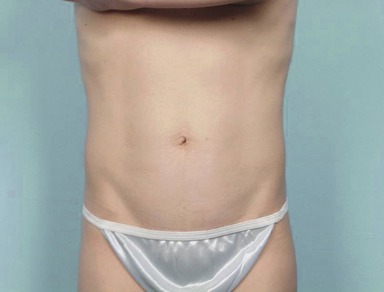
Fig. 69.5 Muscle wall laxity, skin redundancy, and fat excess should all be assessed and documented.
The patient wears a bikini bottom or underwear that is typical of the style she likes to wear. Frequently, patients are now wearing underwear that is relatively horizontal, preventing the scar from rising laterally as much as necessary to create high tension that pulls obliquely from each lateral limb against the epigastrium, thereby forcing the scar to be lower and more horizontal than optimal for giving the patient the best possible contour. There are two ways to deal with this. First, one can advise the patient that a higher scar laterally will give a better appearance to the abdomen, which is usually the biggest concern to the patient. But it is also true that styles change, and sooner or later swimsuits and underwear will ride up higher again on the hips, meaning that a low scar would be visible in even one-piece suits. However, a high scar that is optimal for an HLT will always be covered by a one-piece and will be above it and visible only with a low one-piece. Ultimately, the patient must know what to expect with the scar. The other option when the patient wants the scars low is to make the scar lower above the mons, which allows one more room to let the scar course more superiorly up to the lateral ends of the incision. But one must be careful not to remove too much hair-bearing skin in the pubic region; generally it should be about 6.5–7 cm from the anterior labial commissure to the top of the pubic hair on maximum stretch. And the other problem with lowering the scar centrally is that it makes it that much more likely that the old umbilical site will not be able to be excised, and that a short vertical scar to close it will remain in the infraumbilical/suprapubic region. While most all facelifts can begin with a similar initial incision around the ear, varying only in final skin excision, the initial abdominoplasty incision lacks the concrete anatomical landmarks of the ear, and given various abdominal configurations and patient wishes, the initial incision must be customized to each patient.
The midline is marked from xyphoid to umbilicus to the labial commissure. While it is embarrassing to mark this, many women today have pubic hair that is trimmed unevenly, so that drawing a line to the center of the pubic hair can result in a crooked inset of the flap. I then draw a number of vertical lines parallel to the first line from the midline going out laterally to where the incision is expected to end (Fig. 69.8). Additional horizontal lines are drawn to create a checkerboard on the abdomen. This helps not just at this point while marking the patient, but it makes for a much more rapid determination of final resection, reduces the likelihood of unevenness of resection, and facilitates insetting the flap by lining up the closure.
A line is then drawn where you would like the final scar to be. The patient must inspect this and any compromises discussed and made. This line is not where an incision will be made! Because tension will vary along the length of the incision, there are points at which this will be pulled up by the final closure greater than at other areas. So with a pen held horizontally at the level of the desired final scar, the abdomen is pushed up superiorly with the expected tension of the final closure at that point. This will yield a series of dots below the incision. They are checked side by side for evenness. I use a laser level to assure that both ends of the incision are parallel to the floor (Fig. 69.9). Check to assure that the incisions are also located at the same point relative to the hipbone. If there are discrepancies between what is even with the floor and what is even with the body, it needs to be pointed out to the patient, discussed, and documented. The final scar will never be symmetrical. Consents for abdominoplasty should require patients to initial the statement “the scar will not be symmetrical.” Extend the lines for the incision beyond what you think you will need, as this provides for removal of any dog-ear with placement of the incision in the proper location. Keep in mind that some of these patients will at some stage decide to get the posterior part of a lower body lift added, so end the incision at a point that would be within a lower body lift scar. Mark the umbilicus at 12, 3, 6, and 9 so that it is easy to identify those areas and to inset the umbilicus later without concern for there being a twist. Areas for liposuction are marked in the usual manner. Photographs are taken of the marked patient and are printed and posted in the operative room for intraoperative reference.
The patient is sat up only about 25 or 30 degrees; sitting up more than that makes it too easy to over-resect centrally, and it does not allow for significantly more lateral resection which is where resection is emphasized. Start by determining the amount of resection that can be done centrally. In the traditional abdominoplasty, the surgeon’s mind is focused on removing the old umbilical site. In the HLT, the surgeon is at peace with leaving that site behind, but if it can be removed, so much the better. Do not have the mons completely draped off, as the amount of resection is determined by mons distortion. No more than a small of distortion should be accepted and the extent to which the pubic hair is pulled cephalad is also noted, as there must be an adequate distance left between the umbilicus and the top of the pubic hair. Once this is determined, the flap is split up to this point and tacked into place. The Lockwood flap marker is then used to mark the remaining flap, taking note that there should be greater tension laterally than centrally. After it is marked, the central clamp is released and the patient is laid flat again. The proposed excision is then carefully drawn assuring symmetry (Figs 69.10–69.12).
Drains are placed as well as a pain pump, if desired. The patient is sat back up, tacked shut, the umbilicus is matured, and closure is done. Lockwood advocated a vertical slit with no excision. If indeed the lateral arms of the abdominoplasty are oblique, then their closure under tension will help to open up the slit. One should be cautious about umbilicoplasty designs that might be prone to enlarge from the high lateral tension.
Complications
Pearls & pitfalls
Pearls
• Accept that removing the umbilical site is not a goal of the procedure.
• Realize that pulling inferolaterally from the epigastrium to each groin most optimally rejuvenates the epigastrium and avoids the distortion of the mons seen with a standard abdominoplasty.
• The HLT requires a longer scar than a traditional procedure because of the amount of skin taken laterally, and it requires that the lateral limbs be angled upwards so that they are pulling at oblique angles towards the epigastrium. The patient must be made aware of this and accept this.
• Recognize that the final scar is not where the initial incision was made; it will float superiorly based upon the tension following final resection.
Pitfalls
• The patient needs to know ahead of time how long the scar will be; they also need to know that even with optimal SFS repair that it may still widen. Many patients have a C-section scar that they wish to compare it to; while occasionally it can look that good, since the C-section scar heals in a condition of skin laxity and the HLT in a condition of tension, the HLT usually spreads more.
• It sometimes seems very easy to pull just a bit more to remove the umbilical site, but avoid the temptation to do so if it distorts the mons or raises the pubic hair so high that the umbilicus seems to close to the top of the pubic hair.
• Sometimes the transition from the very high lateral tension at the end of the incision to the unpulled skin behind it results in a large dog-ear of sorts. With a traditional abdominoplasty, the greatest tension is in the center, so there is a relatively long distance at which the tension gradually diminishes. To reduce this, it is often necessary to lengthen the incision and/or to perform aggressive liposuction to defat this area.
• PE, PE, PE. This cannot be overstated. Every patient should be considered to be at risk. Keep abreast of the most current recommendations. This is a very real and even inevitable complication, but being diligent about avoiding it and recognizing early signs and symptoms can reduce the incidence and consequence.
Summary of steps
2. The patient wears a bikini bottom or underwear that is typical of the style she likes to wear.
3. The midline is marked from xyphoid to umbilicus to the labial commissure. A number of vertical lines may be drawn parallel to the first line from the midline going out laterally to where the incision is expected to end. Additional horizontal lines are drawn to create a checkerboard on the abdomen.
4. A line is then drawn where you would like the final scar to be.
5. The patient is given a general anesthetic.
6. Incision is made and dissection continued with an electrocautery.
7. If it is obvious that the umbilical site will be removed, the flap should be split to allow for easier dissection up towards the xyphoid.
8. Marcaine with epinephrine is injected along the rectus sheath. Suturing is then done.
9. The flap is irrigated, debris is washed away, and hemostasis is achieved.
10. The patient is sat up about 25 or 30 degrees. The amount of resection that can be done centrally is determined. The proposed excision is then carefully drawn assuring symmetry.
11. The excision is done with a knife in the skin and then a cautery, pulling on the discarded part of the flap to assure that the cut is done perpendicular to the cut edge.
12. Drains are placed as well as a pain pump, if desired. The SFS is closed with simple buried 0 Nurolons dipped in betadine. The final skin closure is done with 4-0 Monocryl followed by Steri-Strips.
Lockwood TE. High-lateral-tension abdominoplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96(3):603–615.
Lockwood TE. Is the standard abdominoplasty obsolete? In: Jurkiewicz MJ, Culbertson JH. Operative techniques in plastic and reconstructive surgery: Abdominoplasty. Philadelphia, PA: WB Saunders; 1996:77–81.
Lockwood TE. Lower body lift with superficial fascial system suspension. Plast Reconstr Surg. 1993;92(6):1112–1122.
Lockwood TE. Lower-body lift. Aesthet Surg J. 2001;21(4):355–370.
Lockwood TE. Maximizing aesthetics in lateral-tension abdominoplasty and body lifts. Clin Plast Surg. 2004;31(4):523–537.
Lockwood TE. Superficial fascial system (SFS) of the trunk and extremities: a new concept. Plast Reconstr Surg. 1991;87(6):1009–1018.
Lockwood TE. The role of excisional lifting in body contour surgery. Clin Plast Surg. 1996;23(4):695–712.
Matarasso A. Abdominolipoplasty: A system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy. Aesthet Plast Surg. 1991;15(2):111–121.
Matarasso A. Liposuction as an adjunct to a full abdominoplasty revisited. Plast Reconstr Surg. 2000;106(5):1197–1202.
Matarasso A. Liposuction as an adjunct to a full abdominoplasty. Plast Reconstr Surg. 1995;95(5):829–836.
Shestak KC. Marriage abdominoplasty expands the mini-abdominoplasty concept. Plast Reconstr Surg. 1999;103(3):1020–1031.
Teitelbaum S. Demystifying high-lateral-tension abdominoplasty. Aesthet Surg J. 2006;26(3):325–329.








 inches. But this varies with the tension on the skin flaps, and there are times that it is almost horizontal, yet the tension is greater laterally than centrally.
inches. But this varies with the tension on the skin flaps, and there are times that it is almost horizontal, yet the tension is greater laterally than centrally.





