80
Heritable Connective Tissue Disorders
Heritable connective tissue disorders present with a broad range of cutaneous and extracutaneous manifestations. Recognition of characteristic skin findings is often critical to establishing the diagnosis and identifying associated internal involvement, which may include life-threatening cardiovascular disease (e.g. in the vascular type of Ehlers–Danlos syndrome [EDS] and pseudoxanthoma elasticum [PXE]).
Ehlers–Danlos Syndrome
• The cardinal physical findings of hyperextensible, fragile skin, and hypermobile joints (Fig. 80.1) are present to varying degrees in different subtypes of EDS (Table 80.1).




Fig. 80.1 Clinical features of Ehlers–Danlos syndrome (EDS). Patients with classic EDS demonstrating joint hypermobility (A), hyperextensible skin (B), and a widened atrophic scar (C). Extensive bruising on the shins in a patient with dermatosparaxis (D); similar changes can be seen in vascular EDS. D, Courtesy, Julie V. Schaffer, MD.
Table 80.1
Major types of Ehlers–Danlos syndrome.
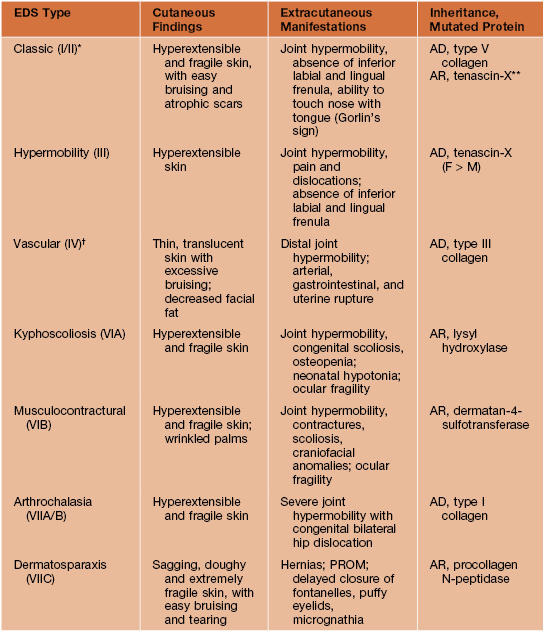
* Most common form of Ehlers–Danlos syndrome.
** May be associated with congenital adrenal hyperplasia due to a contiguous gene syndrome.
† Loeys–Dietz syndrome type II (see Table 80.5) can have a similar clinical presentation.
AD, autosomal dominant; AR, autosomal recessive; PROM, premature rupture of fetal membranes.
• Manifestations of cutaneous fragility include easy bruising (sometimes leading to suspicion of a bleeding disorder; see Fig. 80.1D) and gaping, ‘fish-mouth’ wounds from minor trauma that heal with widened, atrophic scars (see Fig. 80.1C); additional findings may include smooth velvety skin, molluscoid pseudotumors (fleshy nodules in sites of repetitive trauma), subcutaneous spheroids over bony prominences (small, hard nodules that represent calcified fat lobules), piezogenic papules (see Chapter 82), and elastosis perforans serpiginosa (see Chapter 79).
Pseudoxanthoma Elasticum
• Thin yellowish papules coalesce to form cobblestoned plaques (resembling ‘plucked chicken skin’) on the lateral neck and in other flexural sites (e.g. antecubital and popliteal fossae, axillae, groin) (Fig. 80.2); decreased elasticity leads to sagging skin in affected areas (see Fig. 80.2D), and yellow papules on the oral mucosa may be evident (see Fig. 80.2E).





Fig. 80.2 Mucocutaneous findings in pseudoxanthoma elasticum. Yellowish papules and ‘cobblestoned’ plaques on the neck (A, B) and in the antecubital fossa (C). Thickened, yellowish, sagging skin in the axilla (D). Yellow papules on the inner aspect of the lower lip (E). C, D, Courtesy, Julie V. Schaffer, MD.
• DDx: PXE-like cutaneous and extracutaneous findings can be seen in generalized arterial calcification of infancy (ENPP1 mutations), PXE-like disorder with coagulation factor deficiency (GGCX mutations), β-thalassemia, and sickle cell anemia; other conditions featuring PXE-like skin lesions are outlined in Table 80.2.
Table 80.2
Differential diagnosis of pseudoxanthoma elasticum (PXE)-like skin findings.
Additional considerations may include PXE-like skin lesions in patients receiving D-penicillamine, exposed to saltpeter, or with chronic kidney disease, β-thalassemia, or sickle cell anemia.
| Disorder | Patient Characteristics | Clinical Features |
| Actinic elastosis | Middle-aged and older adults with lightly pigmented skin and a history of chronic sun exposure | Yellow to gray, thickened, lax, finely to coarsely wrinkled skin; photodistribution on the lateral forehead, neck, dorsal aspect of the forearms |
| Perforating calcific elastosis* | 5th–8th decades; primarily multiparous black women** | Plaque composed of coalescing keratotic papules (most apparent at the periphery); periumbilical area >> breasts |
| PXE-like papillary dermal elastolysis (PPDE)† and white fibrous papulosis of the neck (WFPN)† | 5th–9th decades; primarily Caucasian women and (for WFPN) Japanese men | Multiple 2- to 3-mm yellow, skin-colored, or (in WFPN) whitish papules; in PPDE, coalesce to form plaques with a cobblestone appearance; neck > upper trunk, axillae, flexor forearms, lower abdomen |
* Also referred to as periumbilical perforating PXE.
** Occasionally associated with an increased calcium-phosphate product in chronic kidney disease.
† Related conditions within the spectrum of fibroelastolytic papulosis; late-onset focal dermal elastosis has a similar clinical presentation.
• Rx: an approach to management of PXE is presented in Table 80.3.
Table 80.3
A multidisciplinary approach to the management of pseudoxanthoma elasticum.
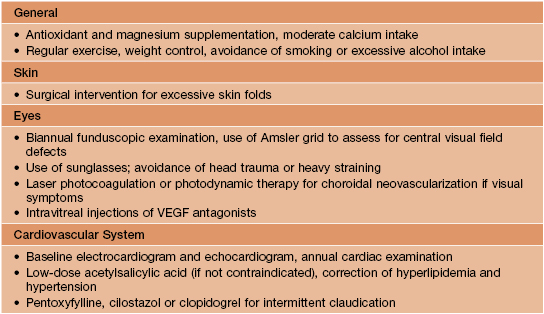
VEGF, vascular endothelial growth factor.
Cutis Laxa
• Heterogeneous group of heritable and acquired disorders (Table 80.4) characterized by loose, sagging skin due to sparse and fragmented elastic fibers.
Table 80.4
Etiologies of cutis laxa.
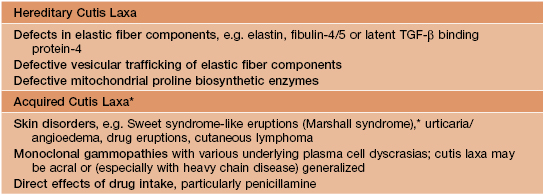
* Sometimes in the setting of α1-antitrypsin deficiency.
TGF-β, transforming growth factor-β.
• Skin involvement is often generalized, giving patients a prematurely aged appearance (Fig. 80.3), but it may be localized to acral or periorbital sites; cutaneous findings are present at birth in most heritable forms of cutis laxa, developing later in acquired cutis laxa and some autosomal dominant variants.

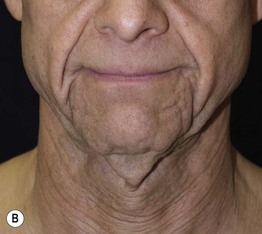
Fig. 80.3 Clinical features in cutis laxa. A Loose skin and drooping jowls in an infant with heritable cutis laxa. B Sagging folds of skin giving a prematurely aged appearance to a man with acquired cutis laxa associated with multiple myeloma. A, Courtesy, Thomas Schwarz, MD. B, Courtesy, Jeffrey P Callen, MD.
• Extracutaneous manifestations can include emphysema, hernias (e.g. umbilical, inguinal), diverticula (e.g. GI, genitourinary), cardiovascular defects, musculoskeletal or craniofacial anomalies, and developmental delay; these findings are most common in autosomal recessive variants and occasionally occur in acquired forms.
• DDx: PXE and related conditions, mid-dermal elastolysis (see Chapter 82), anetoderma (see Chapter 82; smaller, circumscribed lesions), hereditary gelsolin amyloidosis.
Other Disorders
• Additional heritable connective tissue disorders with cutaneous manifestations are summarized in Table 80.5.
Table 80.5
Additional heritable connective tissue disorders with cutaneous findings.
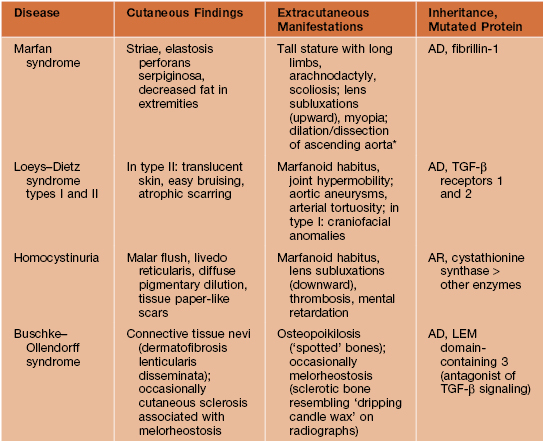
* Rx: β-blockers and angiotensin II receptor blockers, which antagonize pathogenic TGF-β signaling.
AD, autosomal dominant; AR, autosomal recessive; TGF-β, transforming growth factor-β.
For further information see Chs. 95 and 97. From Dermatology, Third Edition.







