Chapter 59 Herbs, Complementary Therapies, and Integrative Medicine
Dietary Supplements
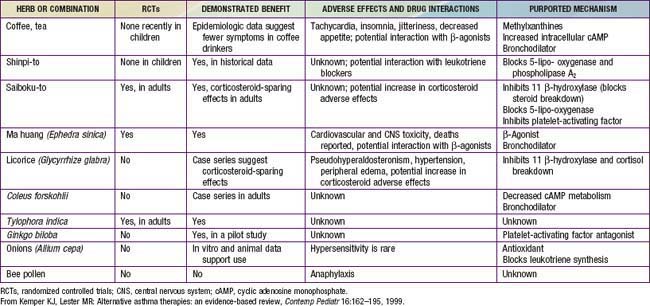
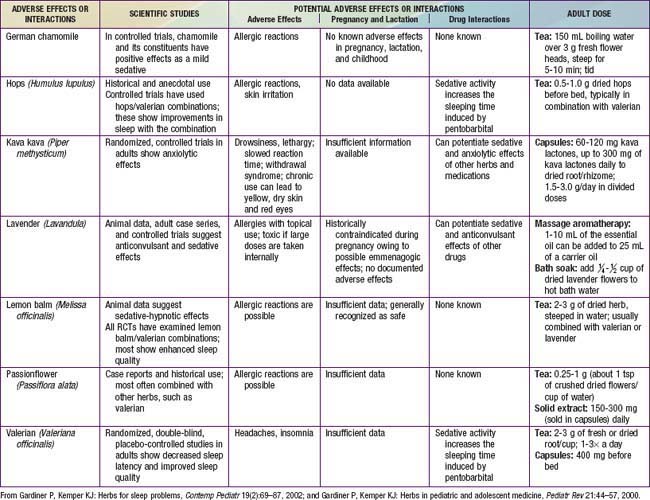
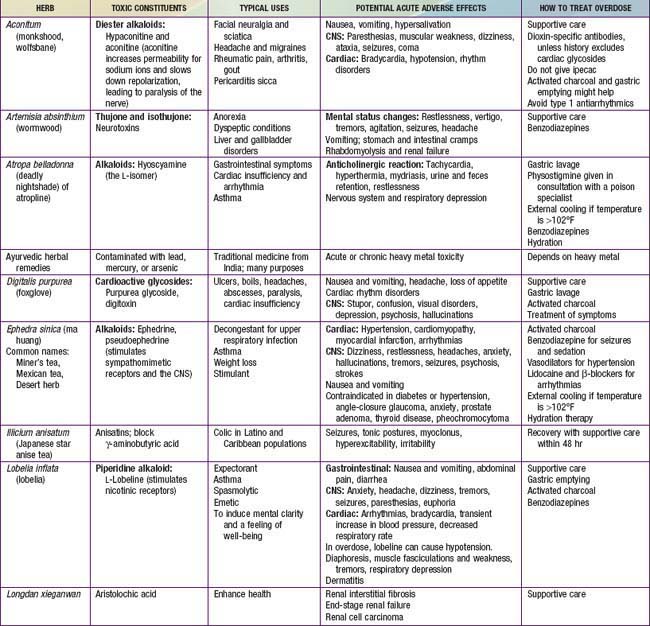
Although they are generally safe, natural products can cause serious toxicity (Tables 59-1 to 59-5). For example, acute hepatic toxicity and death can result from ingestion of even small amounts of Amanita mushrooms. Ephedra, also known as ma huang, is banned as a weight loss or sports supplement in the United States because of its toxicity. Even when a product is safe when used correctly, it can cause mild or severe toxicity when used incorrectly. For example, although peppermint is a commonly used and usually benign gastrointestinal spasmolytic included in after-dinner mints, it can exacerbate gastroesophageal reflux. Probiotics are generally safe when taken orally, but in an immune-compromised patient in an ICU setting, they can cause sepsis. Excessive vitamin C or magnesium can cause diarrhea.
| ACTION | HERB OR SUPPLEMENT FOR TOPICAL USE |
|---|---|
| Soothing, emollient | Aloe, calendula |
| Anti-inflammatory | Aloe, chamomile, evening primrose oil, lemon balm |
| Antiviral | Aloe vera, calendula, chamomile, lemon balm |
| Antibacterial | Aloe vera, calendula, chamomile, lavender, lemon balm, tea tree oil |
| Antifungal | Lavender, tea tree oil |
From Gardiner P, Coles D, Kemper KJ: The skinny on herbal remedies for dermatologic disorders, Contemp Pediatr 18:103–104, 107–110, 112–114, 2001.
Table 59-5 SPANISH-ENGLISH BOTANICAL NAME TRANSLATION CHART*
| SPANISH NAME | ENGLISH NAME | BOTANICAL NAME |
|---|---|---|
| Ajo | Garlic | Allium sativum |
| Azarcon | Lead tetraoxide | Not a plant |
| Azogue | Mercury | Not a plant |
| Cebolla | Onion | Allium cepa |
| Cenela | Cinnamon | Cinnamomum aromaticum |
| Clavo | Cloves | Eugenia aromatica |
| Comino | Cumin | Cuminum cyminum |
| Epasote or herba Sancti Mariae | Wormseed | Chenopodium anthelminticum |
| Estafiate | Wormwood | Artemisia absinthium |
| Eucalipto | Eucalyptus | Eucalyptus globulus |
| Granada | Pomegranate | Punica granatum |
| Jengibre | Ginger | Zingiber officinale |
| Limon | Lemon | Citrus limon |
| Manzanilla | Chamomile | Anthemis nobilis or Chamomilla recutita or Matricaria chamomilla |
| Oregano | Oregano | Origanum vulgare |
| Pelos de elote | Corn silk | Zea mays |
| Savila | Aloe vera | Aloe vera |
| Siete jarabes | Mixture of syrup of sweet almond, castor oil, balsam resin, wild cherry, licorice, cocillana bark, honey | |
| Tomillo | Thyme | Thymus vulgaris |
| Una de gato | Cat’s claw | Uncaria tomentosa |
| Valeriana | Valerian | Valeriana officinalis |
| Yerba buena | Spearmint | Mentha spicata |
* Prepared with assistance of Laura Howell, MD.
Evidence about the effectiveness of dietary supplements to prevent or treat pediatric problems is mixed, depending on the product used and condition treated; research in this area is growing rapidly. Some herbal products may be helpful adjunctive treatments for common childhood problems. For example, some herbs have proved helpful for colic (fennel and the combination of chamomile, fennel, vervain, licorice, balm mint), nausea (ginger), irritable bowel syndrome (peppermint), and diarrhea (probiotics) (Chapter 332).
Ball SD, Kertesz D, Moyer-Mileur LJ. Dietary supplement use is prevalent among children with a chronic illness. J Am Diet Assoc. 2005;105:78-84.
Beider S, Mahrer NE, Gold JI. Pediatric massage therapy: an overview for clinicians. Pediatr Clin North Am. 2007;54:1025-1041.
Gardiner P, Phillips RS, Kemper KJ, et al. Dietary supplements: inpatient policies in US children’s hospitals. Pediatrics. 2008;121:e775-e781.
Goldman RD, Rogovik AL, Lai D, et al. Potential interactions of drug–natural health products and natural health products–natural health products among children. J Pediatr. 2008;152:521-526.
Kemper KJ, Vohra S, Walls R. The use of complementary and alternative medicine in pediatrics. Task Force on Complementary and Alternative Medicine, Provisional Section on Complementary, Holistic, and Integrative Medicine, American Academy of Pediatrics. Pediatrics. 2008;122:1374-1386.
Lin YC, Lee AC, Kemper KJ, et al. Use of complementary and alternative medicine in pediatric pain management service: a survey. Pain Med. 2005;6:452-458.
Sadler C, Vanderjagt L, Vohra S. Complementary, holistic, and integrative medicine: butterbur. Pediatr Rev. 2007;28:235-238.
Shamseer L, Vohra S. Complementary, holistic, and integrative medicine: cranberry. Pediatr Rev. 2007;28:e43-e45.
Vohra S, Johnston BC, Cramer K, et al. Adverse events associated with pediatric spinal manipulation: a systematic review. Pediatrics. 2007;119:e275-e283.

 of North American academic pediatric pain treatment programs. Although additional studies are needed in children, research in adults suggests that acupuncture can offer significant benefits in the treatment of recurrent headache, depression, and nausea. As with any therapy involving needles, infections and bleeding are expected, but uncommon complications and more serious complications, such as pneumothorax, occur in <1 in 30,000 treatments.
of North American academic pediatric pain treatment programs. Although additional studies are needed in children, research in adults suggests that acupuncture can offer significant benefits in the treatment of recurrent headache, depression, and nausea. As with any therapy involving needles, infections and bleeding are expected, but uncommon complications and more serious complications, such as pneumothorax, occur in <1 in 30,000 treatments.




