Hepatitis Viruses
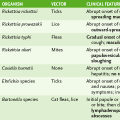
I General Properties (Table 27-1)
TABLE 27-1
Comparison of Hepatitis Viral Infections
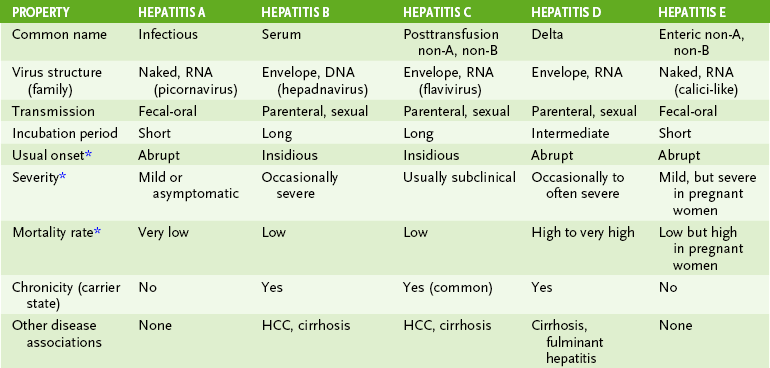
*Refers to acute infection. HDV replicates only in HBV-infected cells. Onset of hepatitis D is most rapid, and the prognosis is worst when HDV infects cells already infected with HBV (superinfection).
• The hepatitis viruses (types A to E) are a diverse group of viruses that infect the liver, resulting in mild to severe acute disease (all types) and chronic disease (types B, C, and D).
A Transmission and onset of hepatitis
1. Hepatitis virions are shed and transmissible before the onset and during symptomatic and asymptomatic phases of infections.
1. Host immune response is the primary cause of liver damage resulting from infection by any of the hepatitis viruses.
2. Direct cytopathic effects contribute to pathogenesis in hepatitis A, E, and D infection.
1. HAV is a small, naked (+) RNA virus belonging to the family Picornaviridae (see Chapter 23).
2. Like other enteroviruses, HAV is acid resistant and can survive in the gastrointestinal tract and sewage systems.
1. After ingestion, HAV probably replicates in the oropharynx and the intestinal epithelium.
2. Viremia spreads the virus to the liver, where it replicates within hepatocytes with minimal damage.
3. Virions are released into the bile and shed into the stool 10 days before symptoms appear.
4. Disease manifestations result from host immune and inflammatory response.
C Hepatitis A disease (infectious hepatitis)
1. Acute disease is usually mild, or asymptomatic, and occurs most often in school-aged children and young adults.
2. Complete recovery occurs in 99% of the cases and confers lifelong immunity.
• Serologic detection of anti-HAV immunoglobulin M (IgM) antibody provides confirmation of hepatitis A diagnosis.
1. Chlorine treatment of water and sewage, good hygienic practices, and avoidance of contaminated food and water (especially uncooked shellfish) reduce HAV transmission.
2. Inactivated HAV vaccine is recommended for travelers to endemic regions.
3. Passive immunization with immune globulin before exposure or soon after can protect contacts.
1. HBV is a small, enveloped virus with a circular, partially double-stranded DNA genome.
2. HBV encodes a reverse transcriptase, which is carried in the virion particle.
3. Only human virus belonging to the family Hepadnaviridae.
4. Unlike most enveloped viruses, HBV virion (Dane particle) is resistant to low pH, moderate heating, and detergents.
1. HBcAg (major core antigen) surrounds genome and core enzymes.
2. HBsAg (surface antigen) is present in the envelope.
3. HBeAg is shed into blood and indicative of active disease (related to HBc).
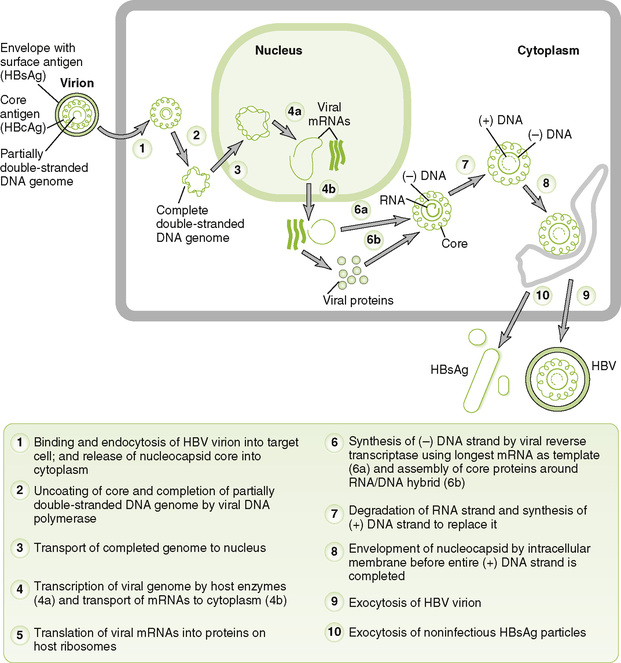
C Replication of HBV (Fig. 27-1)
1. Virions carry a reverse transcriptase similar to the retrovirus enzyme, which is essential to the unique HBV replication mechanism.
2. Viral genome is transcribed into a longer than genomic length RNA.
3. Virions and noninfectious particles composed of HBsAg without genomes are released from infected cells.
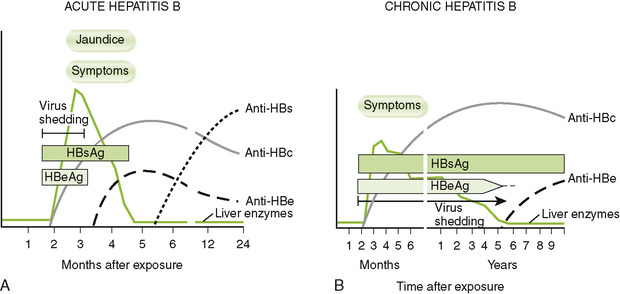
D Markers of the course and nature of hepatitis B disease (Fig. 27-2; Table 27-2)
TABLE 27-2
Serology of Hepatitis A and B Viruses
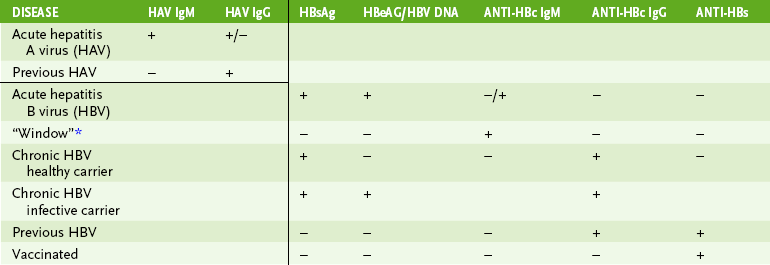
*The window period of HBV disease occurs after infection has been resolved but before anti-HBs can be detected.
1. Serum HBeAg and HBV DNA are the best indicators of the presence of infectious virions (transmissibility).
2. Anti-HBc, IgM antibody to HBcAg, is an indicator of recent acute infection
3. Anti-HBs, antibody to HBsAg, indicates resolution of infection or prior vaccination and confers lifelong immunity.
4. The continued presence of HBsAg, presence of IgG anti-HBcAg, and lack of anti-HBsAg are the best indicators of chronic infection.
1. Viremia spreads HBV virions from the site of entry to the liver.
• Anti-HBsAg produced by prior infection, vaccination, or gammaglobulin prevents infection by blocking spread to the liver.
2. Viral replication in hepatocytes continues for a long period without damage to the liver.
3. Cell-mediated immune response, responsible for both the symptoms and the resolution of HBV infection, develops during the incubation period.
• Strong response → acute disease with complete resolution
• Mild response → mild symptoms (or asymptomatic) with incomplete resolution, leading to chronic infection
4. HBsAg secreted by infected liver cells forms immune complexes with serum antibody that can trigger type III hypersensitivity reactions (e.g., glomerulonephritis, polyarthritis, rash, and itching).
5. Permanent liver damage and cirrhosis can result from fulminant infection, activation of a chronic infection, or coinfection with hepatitis D virus.
6. Long-term chronic infection predisposes patient to primary hepatocellular carcinoma.
F Hepatitis B disease (serum hepatitis)
• About 5% to 10% of HBV infections become chronic, usually after a mild or asymptomatic initial infection.
• Prolonged elevation of serum liver enzymes and the continued presence of HBsAg in the blood mark the chronic state (see Fig. 27-2B).
• Up to 10% of patients with chronic hepatitis B develop cirrhosis and permanent liver damage.
• After about a 30-year period, chronic infection can lead to primary hepatocellular carcinoma (PHC).
1. Asymptomatic and chronic carriers shed HBV and are major sources for spread of the virus.
2. Virion-containing body fluids (blood, semen, vaginal secretions, saliva, and mother’s milk) can be acquired through transfusions, needle stick, sexual contact, and breastfeeding.
1. Screening of blood supply with enzyme-linked immunosorbent assay (ELISA) for HBsAg and antibody to HBcAg
2. HBsAg subunit vaccine is recommended for newborns, health care workers, and other at-risk groups (e.g., individuals with multiple sex partners and patients requiring numerous blood and blood product treatments).
V Hepatitis D Virus (HDV, Delta Agent)
1. HDV replicates only in HBV-infected cells.
2. Virion comprises circular, single-stranded (–) RNA genome and delta antigen surrounded by an HBsAg-containing envelope.
1. HDV is acquired by the same routes as HBV.
2. Coinfection occurs when hepatocytes are infected simultaneously (or nearly so) with HBV and HDV.
3. Superinfection occurs when HDV infects cells that are already infected with HBV → most rapid and severe disease progression.
4. Cytotoxicity and liver damage result from replication of HDV.