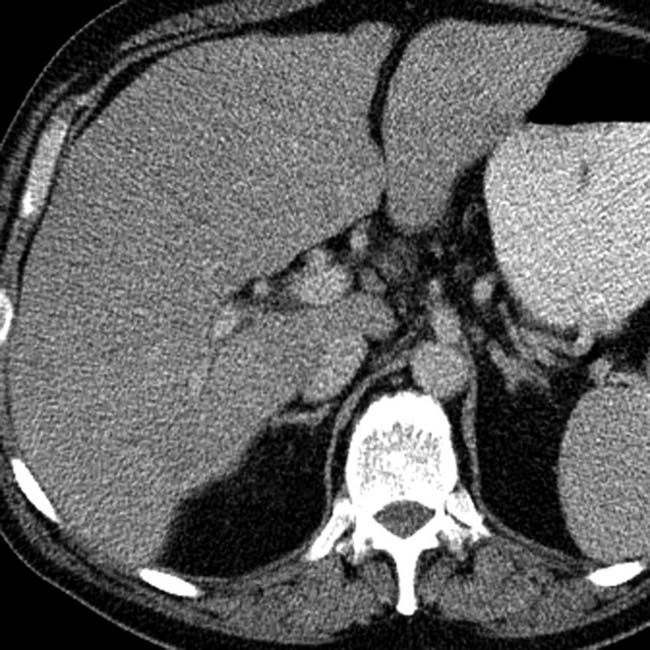
Diffuse infiltration and low density on NECT
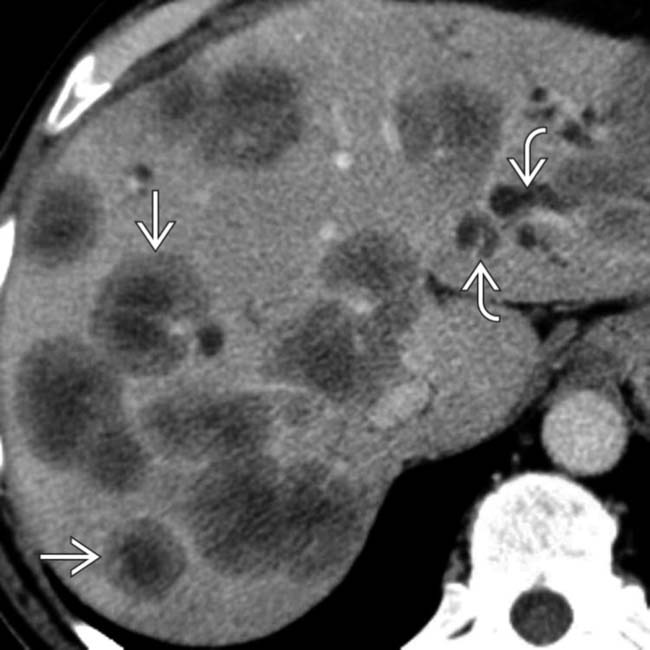
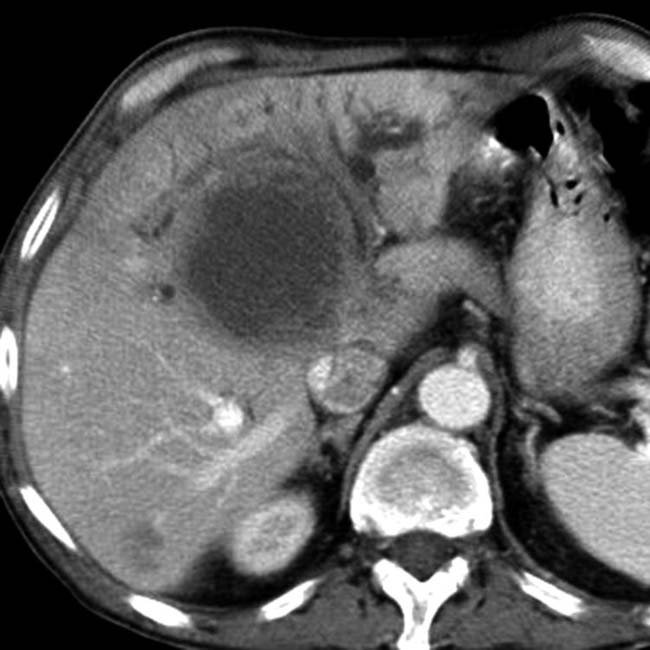
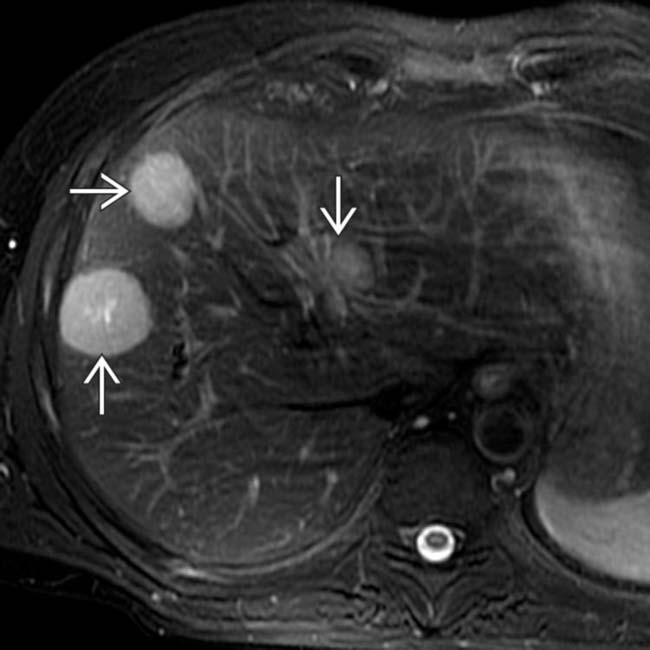
 with a “target” appearance. This is the most typical appearance for liver metastases, especially from colon cancer. Also note the focally dilated bile ducts
with a “target” appearance. This is the most typical appearance for liver metastases, especially from colon cancer. Also note the focally dilated bile ducts  due to compression by the metastases.
due to compression by the metastases.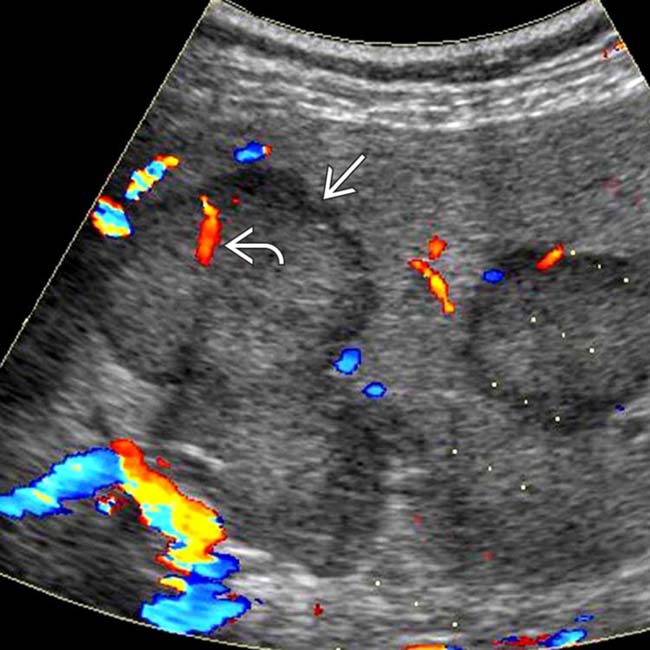
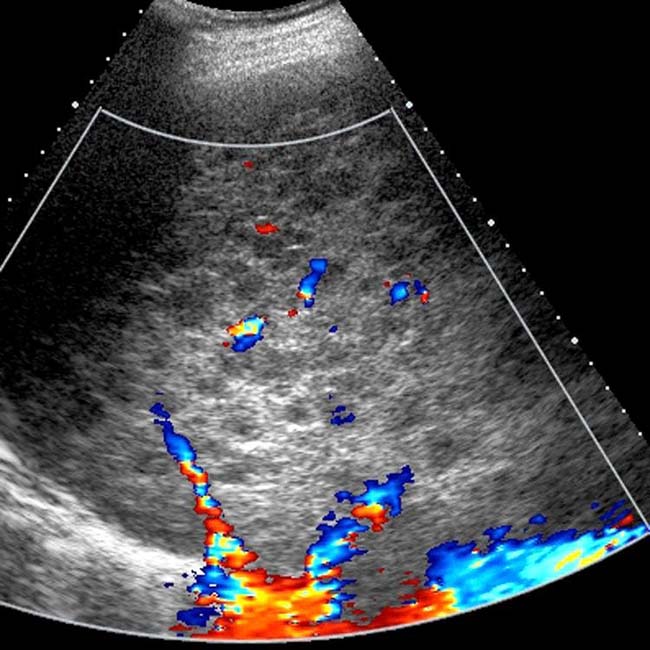
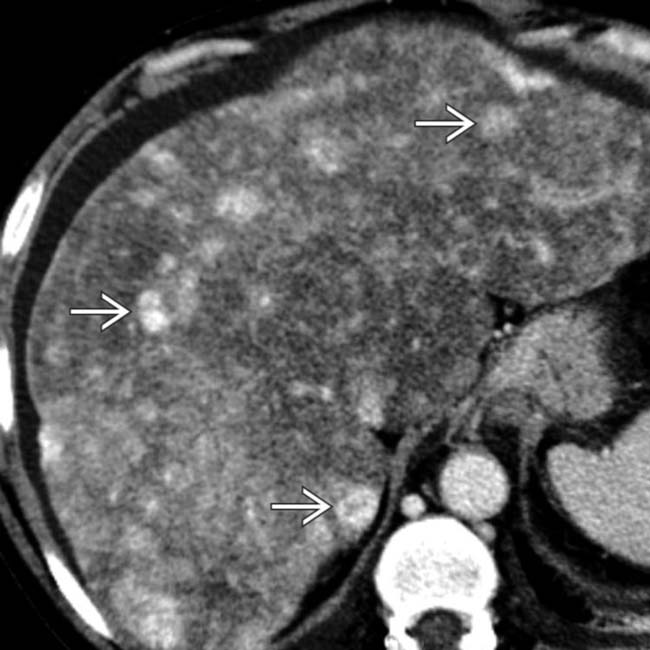
 , some containing visible blood vessels
, some containing visible blood vessels  . This is the typical appearance of metastatic colorectal carcinoma.
. This is the typical appearance of metastatic colorectal carcinoma.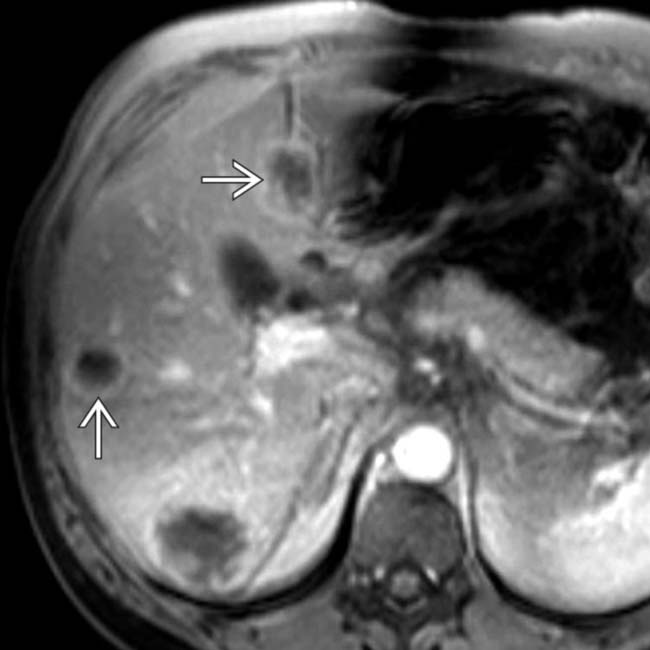
 .
.
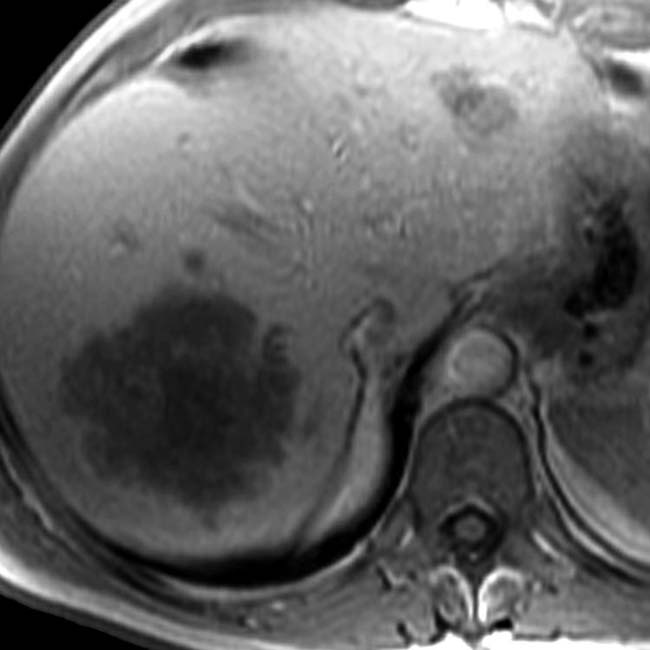
 . Most metastases are heterogeneously hyperintense on T2WI and hypovascular and hypointense on T1WI.
. Most metastases are heterogeneously hyperintense on T2WI and hypovascular and hypointense on T1WI.IMAGING
General Features

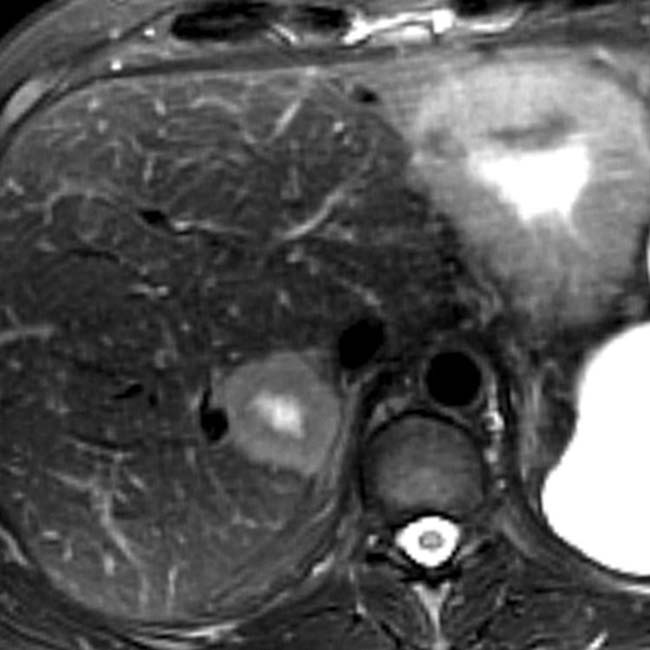
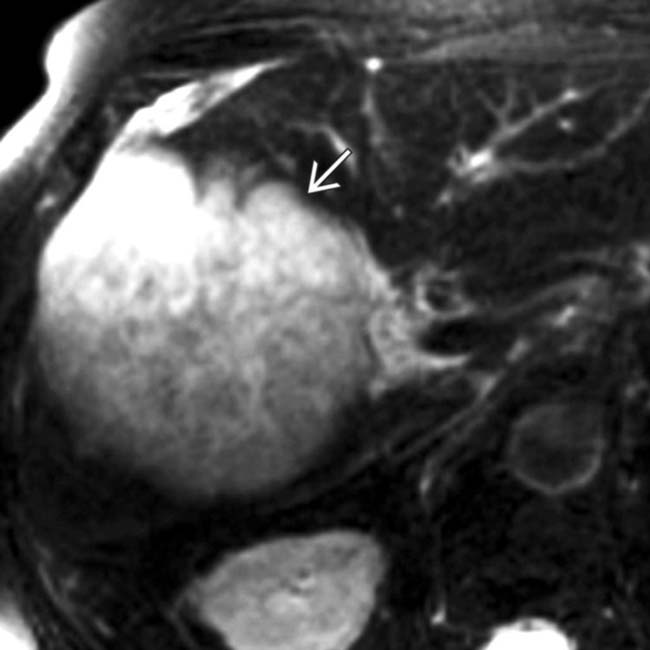
 near the confluence of hepatic veins that mimics the appearance of a hemangioma.
near the confluence of hepatic veins that mimics the appearance of a hemangioma.
 having the typical appearance of a metastasis, rather than a hemangioma. In an oncology patient, sonography is generally less reliable than CT or MR in detection and characterization of solid masses, though exceptions do occur.
having the typical appearance of a metastasis, rather than a hemangioma. In an oncology patient, sonography is generally less reliable than CT or MR in detection and characterization of solid masses, though exceptions do occur.
 adjacent to the IVC.
adjacent to the IVC.
 as nearly isodense to the liver and difficult to recognize. For hypervascular tumors, it is critical to obtain both arterial and venous phase images through the liver. Hypervascular tumors include primary HCC and adenomas; metastatic endocrine, renal, thyroid; and some melanoma sarcoma, and breast cancers.
as nearly isodense to the liver and difficult to recognize. For hypervascular tumors, it is critical to obtain both arterial and venous phase images through the liver. Hypervascular tumors include primary HCC and adenomas; metastatic endocrine, renal, thyroid; and some melanoma sarcoma, and breast cancers.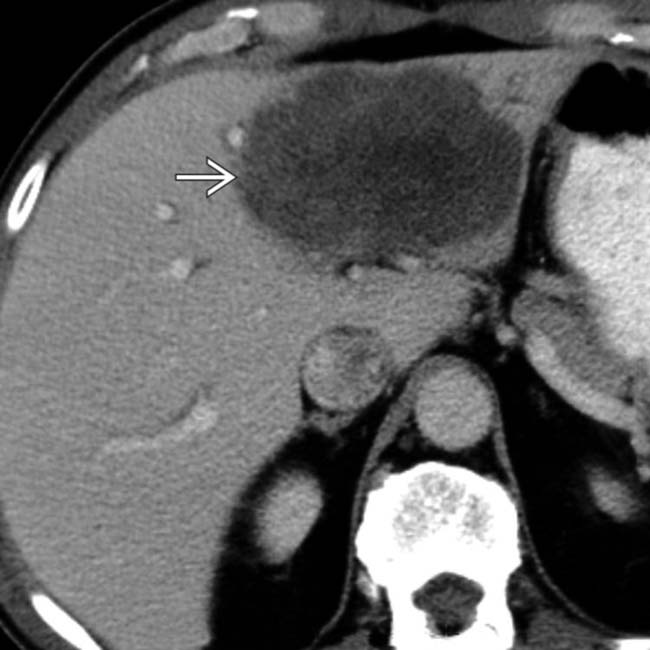
 .
.
 , which could be mistaken for a simple cyst. Cystic metastases can result from a variety of primary tumors, especially sarcomas and cystadenocarcinomas of the ovary. Attention to details such as mural nodularity and comparison with prior imaging studies are key.
, which could be mistaken for a simple cyst. Cystic metastases can result from a variety of primary tumors, especially sarcomas and cystadenocarcinomas of the ovary. Attention to details such as mural nodularity and comparison with prior imaging studies are key.
 that have the peculiar feature of being hyperintense on T1WI, which is attributed to the melanin in these lesions. Most metastases are hypo- or isointense to the liver on T1WI.
that have the peculiar feature of being hyperintense on T1WI, which is attributed to the melanin in these lesions. Most metastases are hypo- or isointense to the liver on T1WI.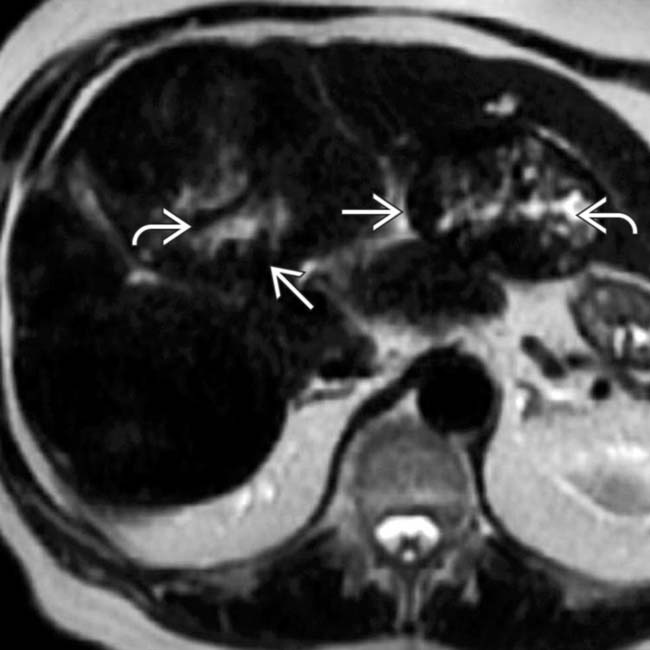
 , but they are nearly isointense to the liver except for foci of necrosis that are hyperintense
, but they are nearly isointense to the liver except for foci of necrosis that are hyperintense  .
.
 .
.
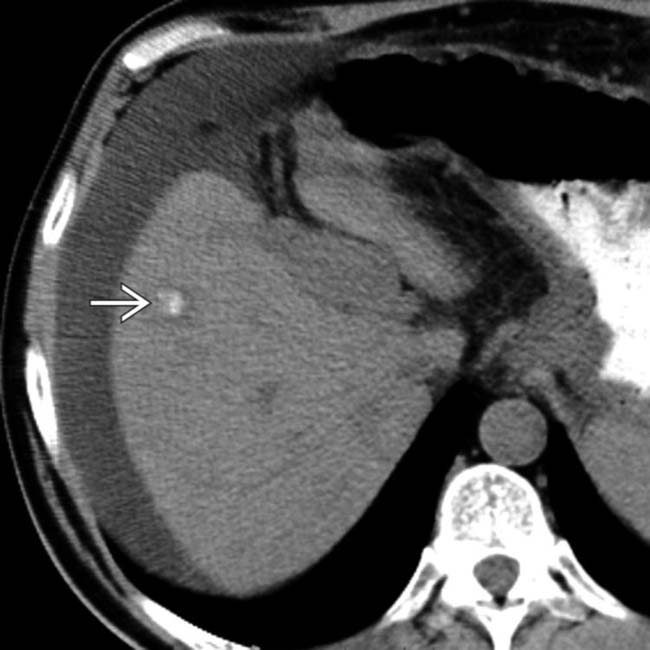
 . The calcification is more difficult to recognize on this phase of CECT. Calcified metastases can result from several primary tumors, especially mucinous adenocarcinomas of the colon and ovary.
. The calcification is more difficult to recognize on this phase of CECT. Calcified metastases can result from several primary tumors, especially mucinous adenocarcinomas of the colon and ovary.
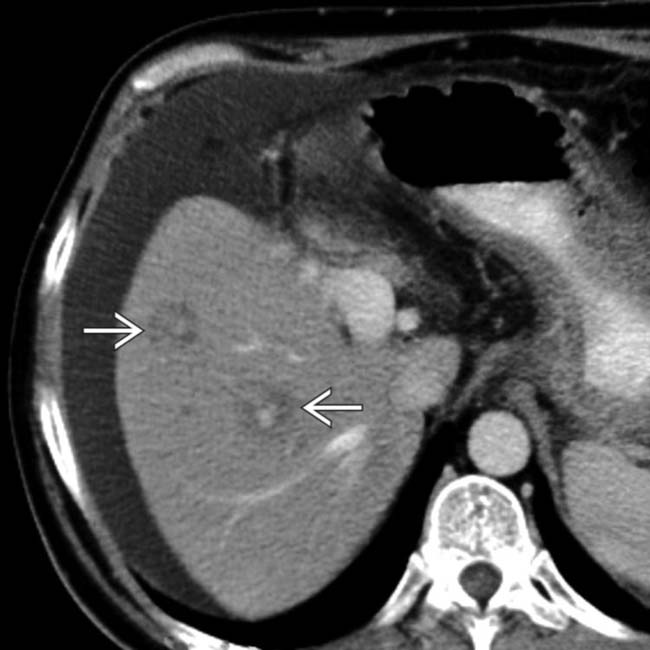
 . The presence of subtle hypodense lesions
. The presence of subtle hypodense lesions  within the liver indicates widespread metastases. In response to chemotherapy, some have shrunk in size and become fibrotic, resulting in the appearance of pseudocirrhosis.
within the liver indicates widespread metastases. In response to chemotherapy, some have shrunk in size and become fibrotic, resulting in the appearance of pseudocirrhosis.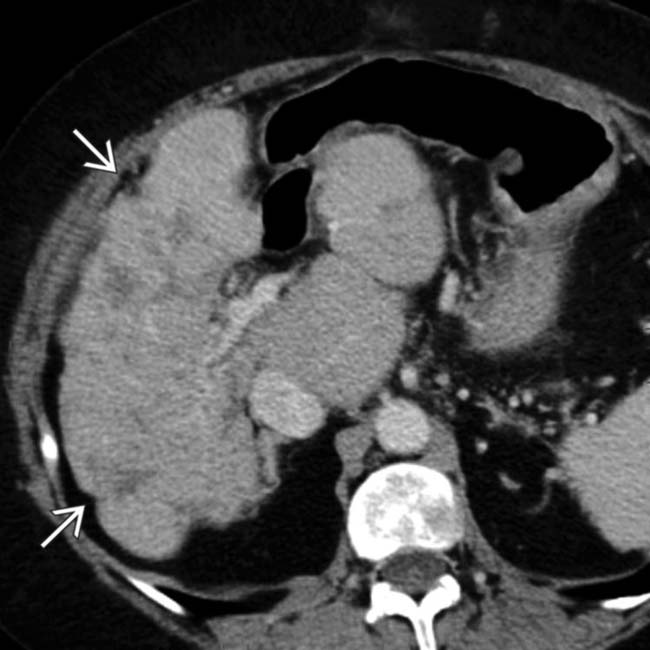
 .
.
 , 3 of which are seen on this section.
, 3 of which are seen on this section.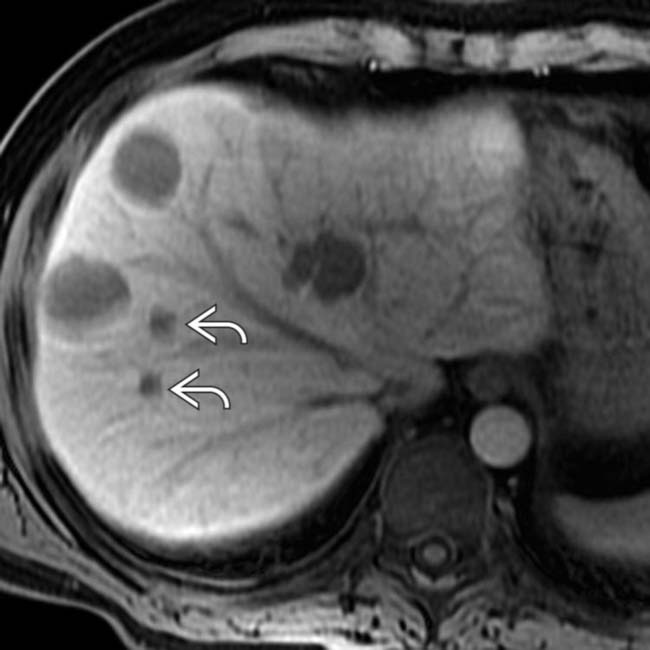
 . Gadoxetate can make small metastases much more evident than on routine MR or CT evaluation. In this patient, the presence of 6 metastases precluded surgical or ablative therapy.
. Gadoxetate can make small metastases much more evident than on routine MR or CT evaluation. In this patient, the presence of 6 metastases precluded surgical or ablative therapy.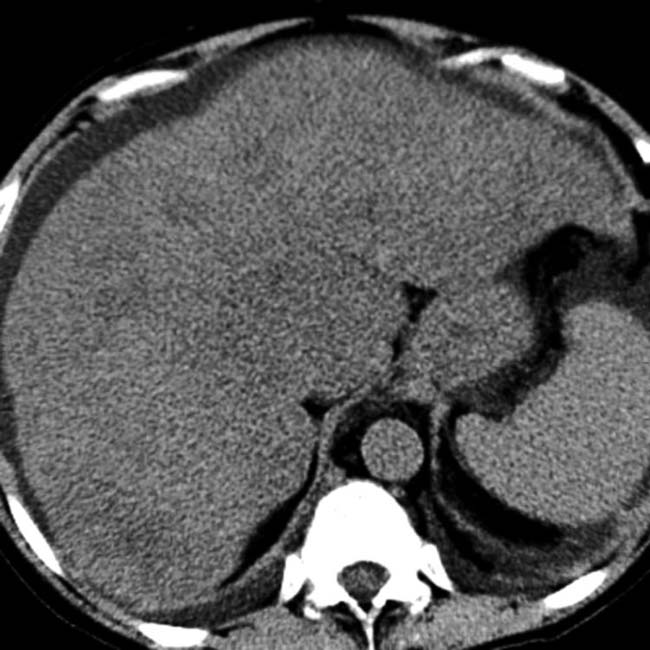
 . Ascites is also present. Diffuse metastases that simulate hepatic steatosis can be seen with a variety of primary tumors, including breast, melanoma, and especially lymphoma.
. Ascites is also present. Diffuse metastases that simulate hepatic steatosis can be seen with a variety of primary tumors, including breast, melanoma, and especially lymphoma.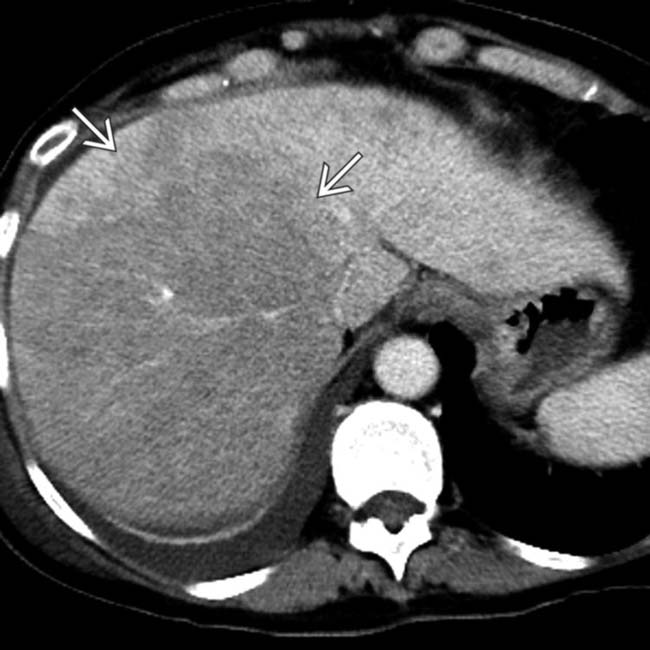
 replacing most of the right lobe of the liver, in a pattern suggesting steatosis or widespread metastases.
replacing most of the right lobe of the liver, in a pattern suggesting steatosis or widespread metastases.
 are FDG avid, indicating malignant disease (metastases). PET/CT can be valuable in detection of subtle or diffuse liver metastases or lymphoma.
are FDG avid, indicating malignant disease (metastases). PET/CT can be valuable in detection of subtle or diffuse liver metastases or lymphoma.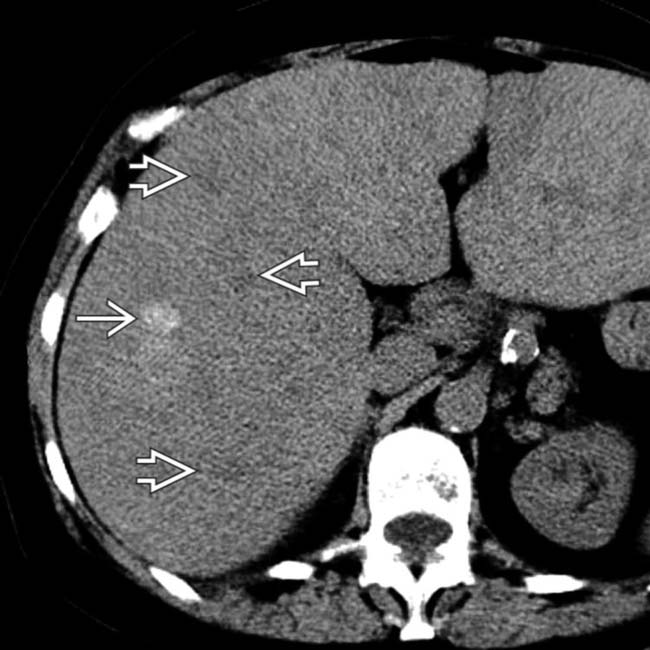
 and others that are hyperdense
and others that are hyperdense  . Melanoma is one of the few metastases that may be hyperdense to normal-attenuation liver; almost any metastases can be hyperdense to fatty liver.
. Melanoma is one of the few metastases that may be hyperdense to normal-attenuation liver; almost any metastases can be hyperdense to fatty liver.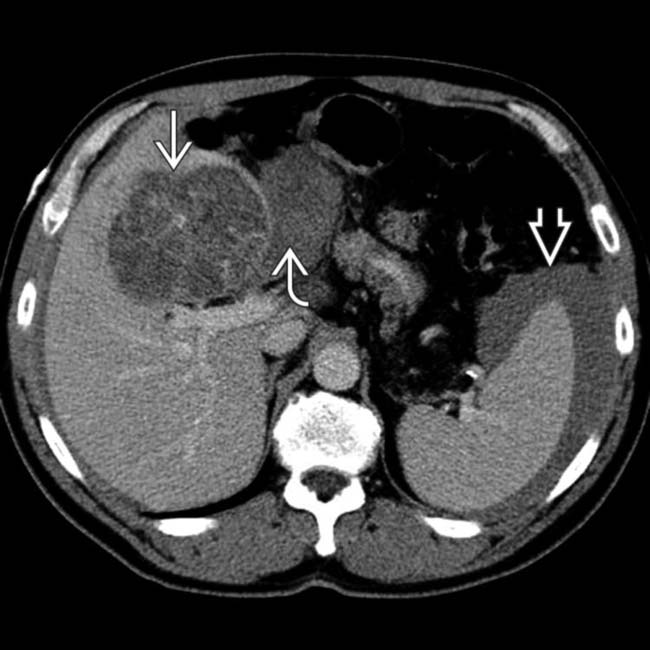
 adjacent to a liver mass
adjacent to a liver mass  , indicating this as the source of bleeding. Also note hemoperitoneum
, indicating this as the source of bleeding. Also note hemoperitoneum  , a relatively rare complication of liver metastases.
, a relatively rare complication of liver metastases.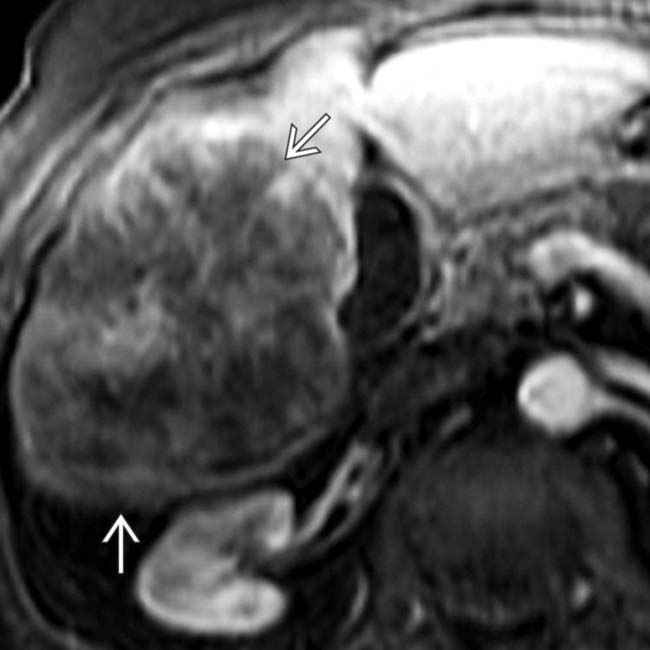
 .
.
 .
.

 in the liver and spleen. Similar masses were present in the kidneys and in multiple nodal groups. AIDS patients and transplant recipients are at high risk for developing non-Hodgkin lymphoma.
in the liver and spleen. Similar masses were present in the kidneys and in multiple nodal groups. AIDS patients and transplant recipients are at high risk for developing non-Hodgkin lymphoma.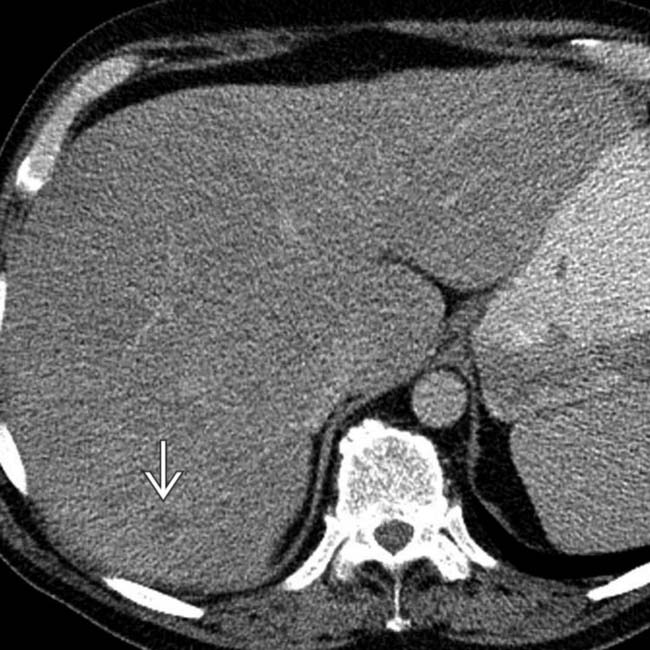
 are also seen.
are also seen.
 , but these are still consistent with focal steatosis or metastases.
, but these are still consistent with focal steatosis or metastases.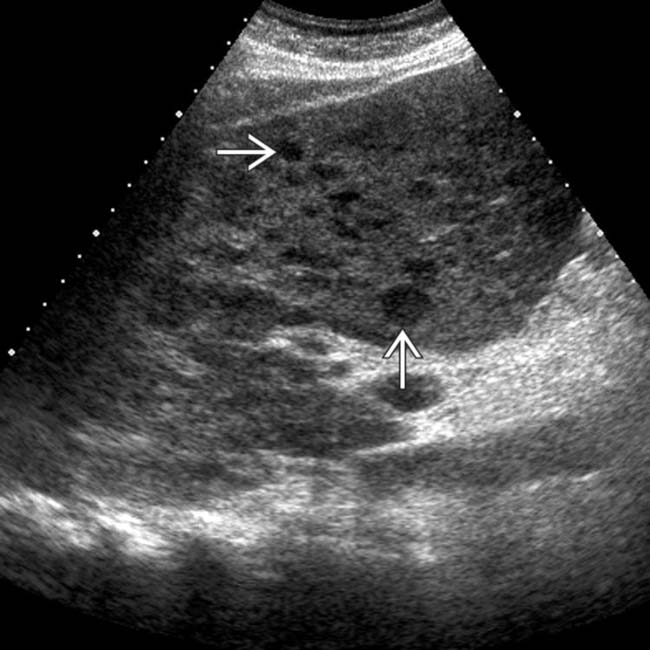
 , many of them are < 1 cm in diameter. Focal steatosis would be echogenic; therefore, these lesions are likely to represent metastases (proven on biopsy).
, many of them are < 1 cm in diameter. Focal steatosis would be echogenic; therefore, these lesions are likely to represent metastases (proven on biopsy).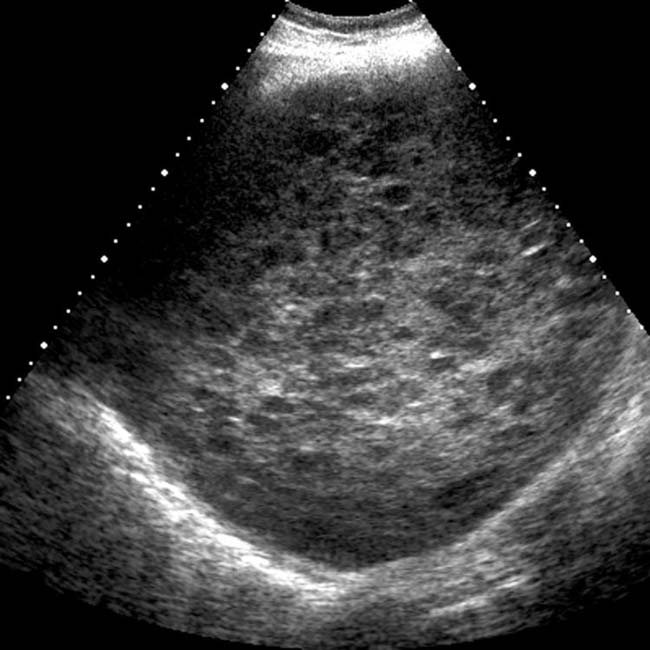

 . Note the obstruction of intrahepatic bile ducts
. Note the obstruction of intrahepatic bile ducts  .
.