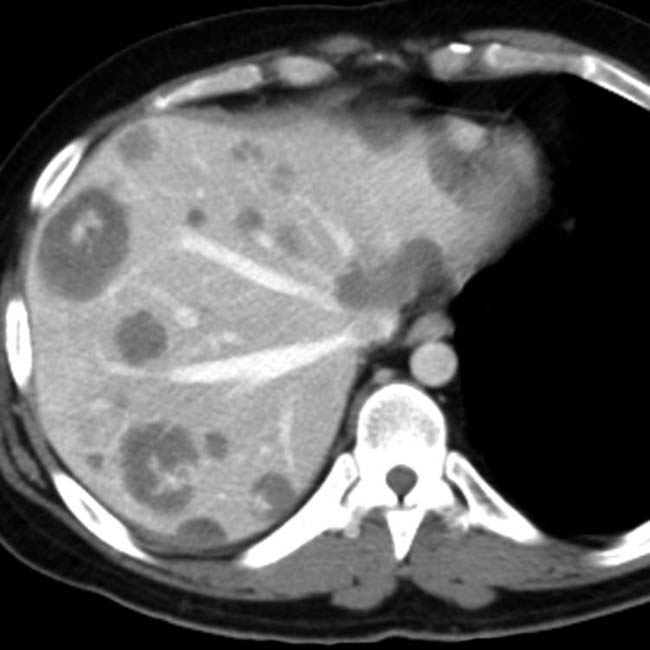
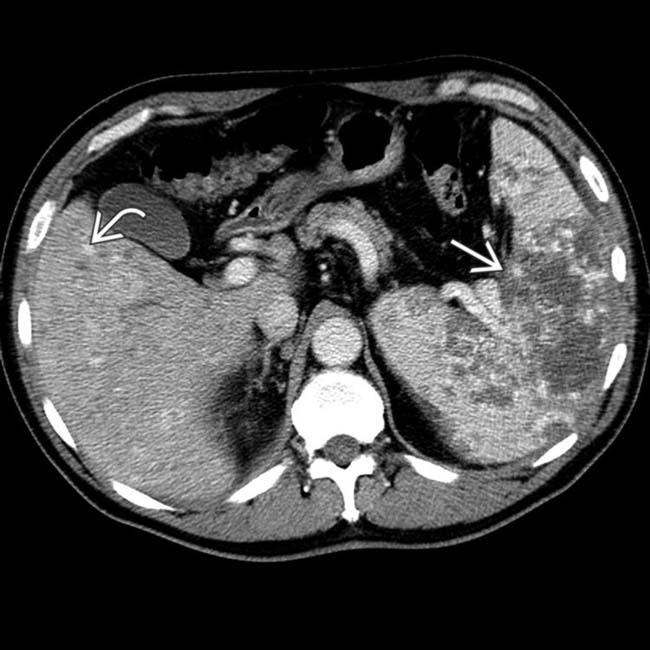
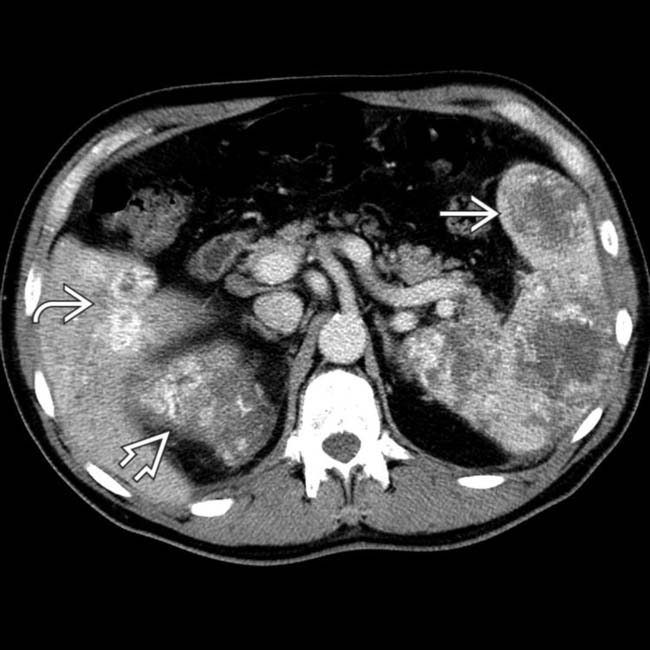
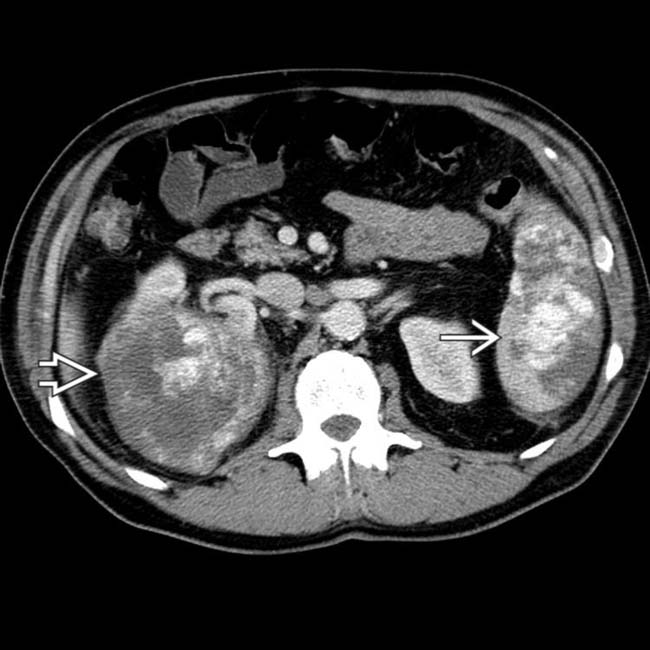
Multifocal hypervascular masses in liver ± spleen

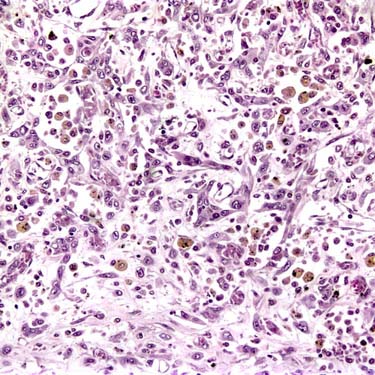
 . Biopsy specimen of a liver lesion confirmed the diagnosis of angiosarcoma.
. Biopsy specimen of a liver lesion confirmed the diagnosis of angiosarcoma.
 involving both the left and right lobes. The focal areas of high signal
involving both the left and right lobes. The focal areas of high signal  represent vascular spaces with slow flow.
represent vascular spaces with slow flow.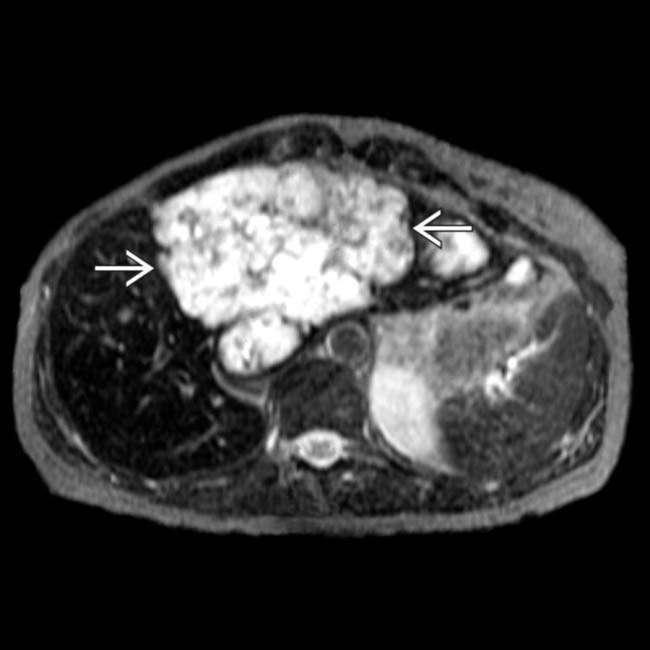
 is of heterogeneous high signal intensity.
is of heterogeneous high signal intensity.
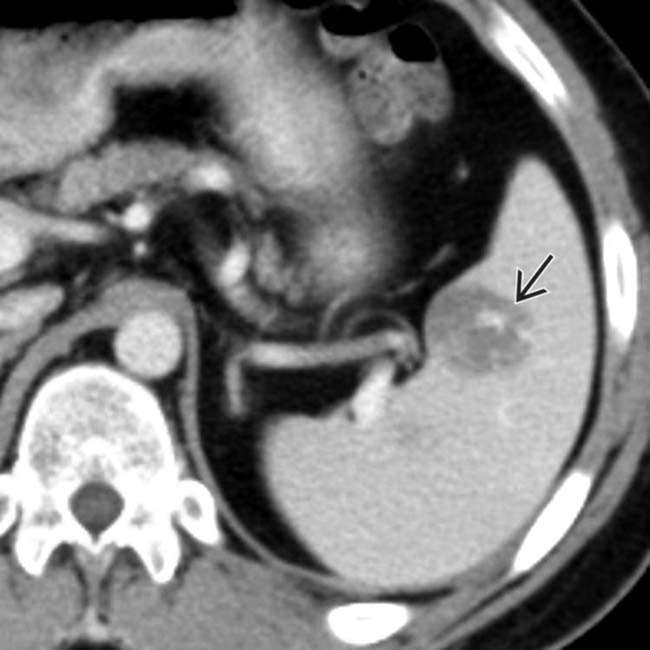
 with heterogeneous enhancement.
with heterogeneous enhancement.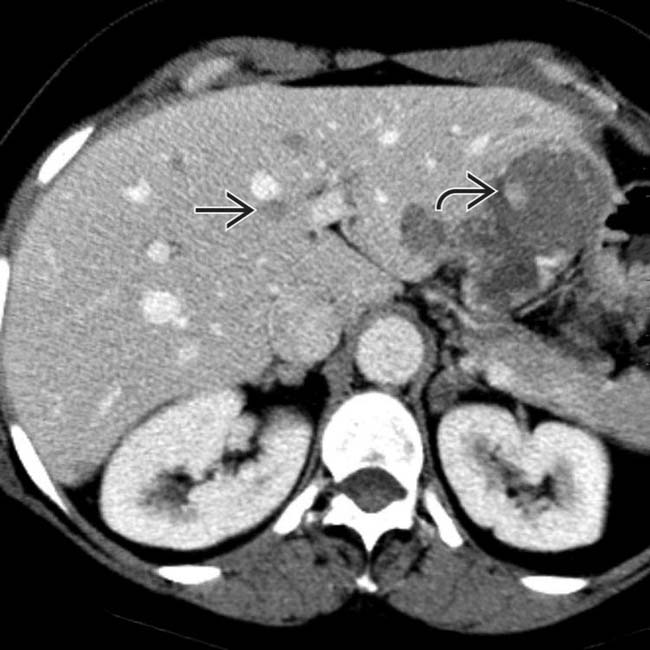
 , whereas other lesions appear as nonspecific, heterogeneous, hypodense masses
, whereas other lesions appear as nonspecific, heterogeneous, hypodense masses  typically seen with metastases.
typically seen with metastases.
 .
.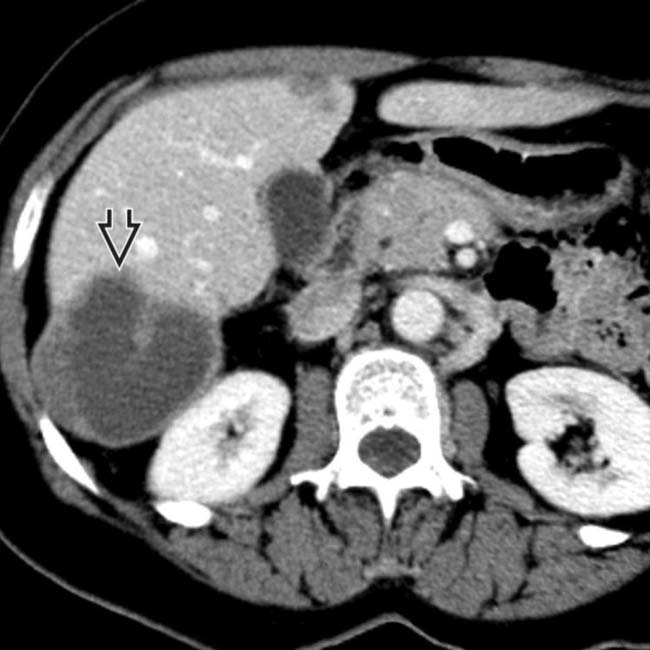
 , illustrating the spectrum of morphologic patterns seen with angiosarcoma.
, illustrating the spectrum of morphologic patterns seen with angiosarcoma.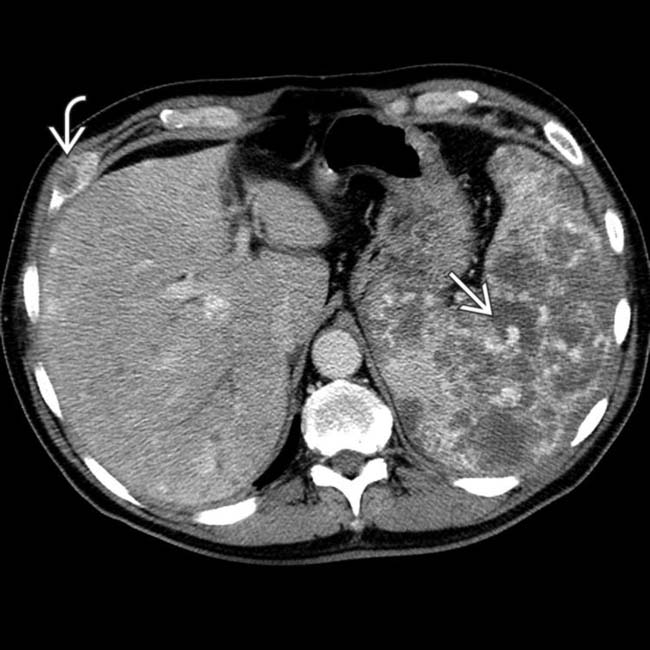
 and an anterior rib
and an anterior rib  .
.
 and subtle, small masses in the liver
and subtle, small masses in the liver  .
.
 , liver
, liver  , and right kidney
, and right kidney  .
.
 and kidney
and kidney  .
.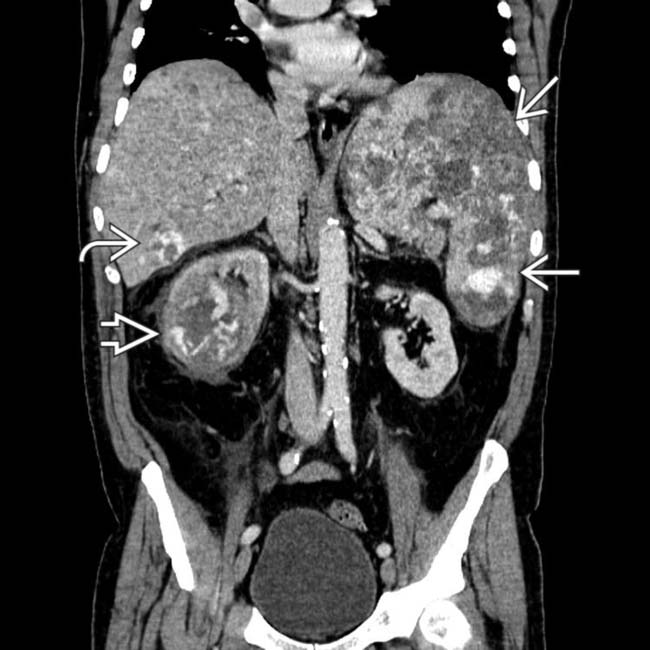
 , spleen
, spleen  , and kidney
, and kidney  .
.
 , spleen
, spleen  , and kidney
, and kidney  . The tumors do not fulfill the strict imaging criteria for hemangioma, including nodular peripheral enhancement that is isodense to blood vessels. Angiosarcoma is a very rare and aggressive tumor that is usually fatal within 1 year of diagnosis.
. The tumors do not fulfill the strict imaging criteria for hemangioma, including nodular peripheral enhancement that is isodense to blood vessels. Angiosarcoma is a very rare and aggressive tumor that is usually fatal within 1 year of diagnosis.



































