Chapter 19 Hemostasis
Coagulation
1. What is the mechanism of coagulation?
2. What activates platelets to form the initial platelet plug at the site of vascular injury?
3. What is the role of activated platelets in the formation of a blood clot?
4. Where is tissue factor located? What is its role in coagulation at the site of vascular injury?
5. What physiologic event leads to the secretion of tissue plasminogen activator and eventually fibrinolysis?
6. How is fibrinolysis affected normally by surgery or massive trauma?
7. What is the potential clinical effect of systemic fibrinolysis? What can be used for the treatment of systemic fibrinolysis?
Common laboratory tests of hemostasis
8. Name some laboratory tests of platelet function.
9. How can a difficult blood draw result in an artificially low platelet count number?
10. Which test of platelet function is the single best predictor of functional platelet disorders?
11. How is a bleeding time test of platelet function performed?
12. What is a normal bleeding time?
13. What are some limitations of the bleeding time test of platelet function?
14. What function of platelets is evaluated by the platelet function analysis test?
15. What are some common causes of platelet dysfunction that can be detected by the platelet function analysis test?
16. What are platelet aggregation studies of platelet function?
17. What are a benefit and a drawback of platelet aggregation studies over other platelet function tests?
18. Name some laboratory tests of coagulation.
19. Low levels of which factors will result in a prolonged prothrombin time?
20. What is the international normalized ratio (INR)? What is it useful for?
21. Low levels of which factors will result in a prolonged partial thromboplastin time?
22. What drug therapy can be monitored by the partial thromboplastin time?
23. A low level of which factor will result in a prolonged prothrombin time and a normal partial thromboplastin time?
24. What is evaluated by the thrombin time test?
25. What is the relationship between the results of the thrombin time test and the results of the prothrombin time and partial thromboplastin time tests?
26. What is tested by the activated clotting time (ACT)? What is its clinical use?
27. What elements of blood clot formation, consolidation, and lysis are measured by thromboelastography?
28. Name some laboratory tests of fibrinolysis.
29. What is suggested by elevated levels of fibrinopeptide or fibrin monomer?
30. What is suggested by elevated levels of fibrin degradation products?
Disorders associated with altered hemostasis during surgery
32. In general, what laboratory values of platelet counts are associated with uncontrolled intraoperative bleeding?
33. In general, what percent of coagulation factors must be present to prevent uncontrolled intraoperative bleeding?
34. Name some diseases associated with an increased incidence of bleeding during surgery.
35. Name some diseases or conditions associated with an increased incidence of thrombosis during surgery.
36. Name some diseases that are associated with initiating disseminated intravascular coagulation during surgery.
37. What are some hereditary coagulation and platelet disorders? Which of these is the most common?
38. How are hereditary coagulation disorders treated?
39. Where is von Willebrand factor stored?
40. Name three important hemostatic functions of von Willebrand factor.
41. How does von Willebrand disease inhibit the formation of fibrin?
42. What are the clinical effects of von Willebrand disease?
43. How can von Willebrand disease be distinguished from factor VIII deficiency?
44. How many types of von Willebrand disease are there? What are they and how are they inherited?
45. What is the anesthetic management of a patient with von Willebrand disease when undergoing a surgical procedure?
46. What disease or condition is a contraindication to the administration of desmopressin acetate tablets (DDAVP)?
47. What are alternative perioperative treatment options of patients with von Willebrand disease if DDAVP is not available?
48. How does vitamin K support coagulation?
49. Which coagulation factors are vitamin K dependent?
50. How could a patient become vitamin K deficient without fasting?
51. Which coagulation factor is not synthesized in the liver? Where, instead, is this factor made?
52. Name three reasons for the increased risk of bleeding caused by severe liver disease.
53. What diseases or conditions are associated with acquired antibodies to coagulation factor VIII? What is the clinical relevance of this?
54. What are some causes of peripheral platelet destruction?
55. What are some causes of thrombocytopenia that can occur during pregnancy?
56. What percent of platelets are normally sequestered in the spleen? What happens during pathologic splenic sequestration of platelets?
57. Name some causes of an impaired quality of platelet function despite the adequate number of circulating platelets.
58. What are some intraoperative conditions that may facilitate bleeding?
59. At what body temperature can hypothermia begin to contribute to intraoperative bleeding?
Disorders favoring thrombosis
61. What are some inherited factor deficiencies that can lead to a hypercoagulable state?
63. What is antiphospholipid syndrome?
64. What percent of patients with systemic lupus erythematosus have circulating lupus anticoagulant? What is the clinical implication of this?
65. What laboratory analysis values for partial thromboplastin time and prothrombin time are associated with lupus anticoagulant?
66. What is the classic set of circumstances, sometimes referred to as Virchow triad, that predisposes patients to perioperative thrombosis?
67. What is disseminated intravascular coagulation (DIC)?
68. What coagulation test results would you expect in a patient with DIC?
69. Which conditions have similar laboratory findings as those of DIC? Which lab finding might help distinguish between DIC and these conditions?
Anticoagulants, thrombolytics, and antiplatelet drugs
71. What are some common clinical complications associated with perioperative thrombosis?
72. What categories of drugs are available to prevent and treat perioperative thrombotic complications?
73. What are some clinically used anticoagulants?
74. What is the mechanism of action of warfarin (Coumadin)?
75. Which of the coagulation factors has the shortest half-life? Why is knowledge of this factor’s plasma half-life important for warfarin therapy?
76. Why is it necessary to coadminister heparin in the early phases of warfarin treatment?
77. What laboratory test monitors warfarin therapy? Why is it necessary to monitor warfarin therapy and not therapy with oral direct thrombin inhibitors?
78. What are some advantages of unfractionated heparin therapy over low-molecular-weight heparin (LMWH) or pentasaccharide (fondaparinux) drugs?
79. Why does unfractionated heparin therapy need to be closely monitored?
80. Why is it necessary to monitor unfractionated heparin therapy and not therapy with LMWH or pentasaccharide drugs?
81. What laboratory test is used to monitor unfractionated heparin therapy?
82. What are some procedures in which heparin is administered to prevent blood clotting? What laboratory test value is the usual end point for heparin therapy in these procedures?
83. How is heparin anticoagulation during surgery reversed? What is the dose? What is its mechanism of action?
84. What are some potential negative effects of the administration of protamine to reverse the anticoagulation effects of heparin?
85. What are some potential disadvantages and/or side effects of the administration of heparin?
86. What is heparin-induced thrombocytopenia? How many types are there?
87. How is the diagnosis of heparin-induced thrombocytopenia (HIT) type 2 made? What is its incidence among patients who receive heparin therapy? What is the mortality rate of patients with HIT type 2?
88. What is the incidence of HIT type 2 among patients who receive heparin therapy? What is the mortality rate of patients with HIT type 2?
89. What is the management of heparin-induced thrombocytopenia once the diagnosis is made?
90. What is heparin resistance and what causes it?
91. How is heparin resistance treated?
92. How does heparin differ from both LMWH and pentasaccharide drugs regarding its effect on thrombin?
93. What is the mechanism of action of LMWH and pentasaccharide drugs for anticoagulation?
94. What are some advantages and disadvantages of LMWH and pentasaccharide drugs over heparin for anticoagulation therapy?
95. What are some direct thrombin inhibitor drugs that are in current clinical use?
96. What are the drawbacks of direct thrombin inhibitor drugs for intraoperative anticoagulation?
97. A patient with a recent history of HIT type 2 is scheduled for a semielective coronary artery bypass graft surgery. If the risk of bleeding associated with intraoperative direct thrombin inhibitor therapy is considered excessive, what other management options exist to meet the need for systemic anticoagulation for cardiopulmonary bypass?
98. What are some thrombolytic drugs currently used in clinical practice?
99. What is the mechanism of action of thrombolytic drugs?
100. How long is surgery contraindicated after thrombolytic therapy?
101. What are some classes of antiplatelet drugs currently used in clinical practice? What are some examples of drugs in each of these classes?
102. How is platelet function affected by aspirin, nonsteroidal antiinflammatory drugs, and COX-2 inhibitors?
103. How is platelet function affected by thienopyridine derivatives?
104. What is the duration of the effects of the thienopyridine derivatives clopidogrel and ticlopidine on platelets after their discontinuation?
105. How is platelet function affected by GPIIb/IIIa antagonists?
106. What is the duration of the effects of GPIIb/IIIa drugs after their discontinuation?
An approach to patients who are anticoagulated
107. When a patient on warfarin presents for surgery, what are the conflicting risks?
108. Which surgeries are generally associated with high risks of perioperative thrombosis?
109. Which baseline medical conditions place patients on chronic warfarin therapy at a high risk of perioperative thrombosis regardless of the type of surgery?
110. Which baseline medical conditions place patients on chronic warfarin therapy at an intermediate risk of perioperative thrombosis regardless of the type of surgery?
111. Which baseline medical conditions place patients on chronic warfarin therapy at a low risk of perioperative thrombosis regardless of the type of surgery?
112. Why is it important to stratify the risk of perioperative thrombosis for patients on chronic warfarin therapy?
113. In what way does the management of patients on chronic warfarin therapy at high risk for perioperative thrombosis differ from those at intermediate or low risk?
114. In a patient receiving perioperative heparin bridging therapy for warfarin treatment, when should the intravenous heparin infusion be stopped prior to surgery and when is it restarted?
115. In a patient receiving perioperative LMWH bridging therapy for warfarin treatment, when is the last dose of LMWH administered and when is it restarted?
116. In which patients should the administration of perioperative heparin likely be avoided?
117. How should a patient on chronic warfarin therapy who needs emergency surgery be managed?
118. Why should the administration of oral vitamin K be considered for the emergency patient on chronic warfarin therapy who is receiving fresh frozen plasma or prothrombin complex to reverse the effects of warfarin?
119. How should vitamin K be administered for emergency surgery in patients on chronic warfarin therapy? Why is this route preferred over the others?
An approach to patients receiving antiplatelet therapy
120. How long do patients with bare metal coronary stents require antiplatelet therapy?
121. How long do patients with drug-eluting coronary stents require antiplatelet therapy?
122. Why do patients with drug-eluting coronary stents require antiplatelet therapy much longer than patients with bare metal coronary stents?
123. How should patients with coronary stents that require antiplatelet therapy be managed in the perioperative period?
An intraoperative approach to uncontrolled bleeding
125. In the event of the massive transfusion of blood, and when laboratory testing is not available, at what volume of blood loss does the dilution of coagulation factors and platelets warrant the transfusion of fresh frozen plasma or platelets, respectively?
126. During ongoing blood loss, what laboratory value would indicate the need for the replacement of coagulation factors with fresh frozen plasma?
127. During ongoing blood loss, what laboratory value would indicate the need for the replacement of platelets with a transfusion of concentrated platelets?
128. During ongoing blood loss, what laboratory value of fibrinogen would indicate the need for a transfusion of cryoprecipitate?
129. What are some indications for the transfusion of cryoprecipitate?
130. What is the role of recombinant factor VIIa in perioperative hemorrhage?
131. List some adjuvant hemostatic agents and their mechanism of action.
132. What are some of the indications for DDAVP as an adjuvant hemostatic agent?
Answers*
Coagulation
1. The traditional thinking regarding the mechanism of coagulation was that there were two independent pathways, which could independently activate a common pathway leading to the generation of thrombin, which converts fibrinogen to fibrin. These two pathways were termed intravascular (intrinsic) and extravascular (extrinsic). It is now believed that this thinking is flawed; it appears the intrinsic pathway is not important in physiologic coagulation per se. Instead, the current understanding is that coagulation is a cell-based process that occurs on the surface of subendothelial cells and platelets, and that it involves elements of both the intrinsic and extrinsic systems. Specifically the extrinsic system generates a small amount of thrombin, which then activates parts of the intrinsic system. The extrinsic system also activates the intrinsic system directly via a recently discovered link between the two systems. This then leads to the overwhelming generation of thrombin (thrombin burst), which causes blood to clot. (349, Figure 22-1)
2. Platelets are activated at the site of vascular injury to form the initial platelet plug by adhering to collagen or von Willebrand factor. (349)
3. Platelets, once activated, degranulate and release large amounts of calcium and factors V and VIII. This activates a series of events that eventually leads to a cross-linked fibrin meshwork that traps activated platelets and red blood cells to form a blood clot. (349)
4. Tissue factor is located on subendothelial cells. Tissue factor located on the surface of perivascular subendothelial cells at the site of vascular injury binds with circulating factor VII to form a complex that leads to coagulation. (349)
5. The secretion of tissue plasminogen activator occurs when the endothelium is activated by injury. This results in the activation of plasminogen to plasmin, which degrades fibrin to soluble products such as D-dimers. This normally remains localized to areas of thrombus. (350)
6. In general, surgery and/or massive trauma results in an elevation of acute phase reactants that induces both a hypercoagulable state and inhibits the normal process of fibrinolysis. (350)
7. The potential clinical effect of systemic fibrinolysis is the inability to dissolve thrombus, or clots, and for continued bleeding. This can occur by unknown mechanisms in the setting of surgery, cardiopulmonary bypass, or massive trauma. Systemic antifibrinolytics such as ε-aminocaproic acid and tranexamic acid have been used to treat systemic fibrinolysis in this setting. (350-351)
Common laboratory tests of hemostasis
8. Laboratory tests of platelet function include the platelet count, bleeding time, platelet function analysis, and platelet aggregation studies. (351)
9. Platelet counts are quantified by automated instruments. Minimal platelet clumping, as can occur with a difficult blood draw, can result in an artificially low platelet count number. To confirm that an automated instrument-measured low platelet count is valid, the platelet count can be examined visually for clumping. Most clinical laboratories visually inspect platelet samples when the results of a platelet count are less than 100,000 cells/μL. (351)
10. The bleeding time is the test of platelet function that is the single best predictor of functional platelet disorders. (351)
11. The bleeding time test is a standardized test that involves making an incision 9 mm long and 1 mm deep on the volar surface of the forearm. A blood pressure cuff is placed on the upper arm insufflated to a pressure of 40 mm Hg. Excess blood is blotted away every 30 seconds with filter paper while not touching the edge of the incision. The time is calculated from incision to the end of bleeding, and this time is the result of the test. (351)
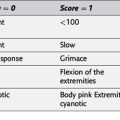
12. A normal bleeding time is less than 11 minutes. (351, Table 22-1)
13. Some limitations of the bleeding time test of platelet function are its required specific standard for performance, the difficulty with controlling the environment in which it is performed, the potential for scar formation at the test site, and that it is not readily available. (351)
14. The platelet function analysis test evaluates for the presence of dysfunctional platelet adhesion. Platelet adhesion is the sticking of platelets to other surfaces. Platelet aggregation, or the sticking of platelets to each other, is not evaluated by this test. (351)
15. Some common causes of platelet dysfunction that can be detected by the platelet function analysis test include uremia, hereditary platelet disorders such as von Willebrand disease, postcardiopulmonary bypass platelet dysfunction, and the presence of antiplatelet medications. (351)
16. Platelet aggregation studies of platelet function test the response of platelets to aggregating agents such as collagen, adenosine diphosphate (ADP), epinephrine, and ristocetin. (351)
17. A benefit of platelet aggregation studies over other platelet function tests is the ability of the test to differentiate between different causes of platelet aggregation dysfunction. A drawback of platelet aggregation studies over other platelet function tests is that it cannot be performed intraoperatively and is rarely performed perioperatively. (351)
18. Laboratory tests of coagulation include the prothrombin time, partial thromboplastin time, thrombin time, fibrinogen levels, ACT, and thromboelastography. (352)
19. Low levels of factors VII, X, V; prothrombin; and fibrinogen prolong the prothrombin time. (352)
20. The international normalized ratio (INR) is a number that standardizes reagent differences between prothrombin time results across different laboratories. The INR is useful for monitoring oral anticoagulant drug therapy with warfarin. (352)
21. Low levels of factors VIII, IX, XI, and XII will result in a prolonged partial thromboplastin time. Adequate levels of factors X and V; prothrombin; and fibrinogen must also be present. (352)
22. Heparin therapy can be monitored by the partial thromboplastin time. (352)
23. A low level of factor VII is the only cause of a prolonged prothrombin time and a normal partial thromboplastin time. (352)
24. The thrombin time test evaluates the thrombin-fibrinogen interaction and is prolonged with low levels of fibrinogen, abnormal fibrinogen, and in the presence of circulating anticoagulants such as heparin. (352)
25. The prothrombin time test and the partial thromboplastin time tests will both be prolonged if the thrombin time test is prolonged. Adequate fibrinogen levels are necessary for all three of these tests of coagulation. (352)
26. The ACT measures the amount of time required for whole blood to clot in a test tube. The ACT test is used clinically to monitor heparin therapy intraoperatively. (352)
27. Thromboelastography measures the time until initial clot formation (clotting factor concentrations and possible anticoagulant medicine), the time until clot formation (fibrinogen and platelets), the absolute clot strength (platelet quantity and aggregation), and the degree of clot lysis (excessive fibrinolysis or antifibrinolytic therapy). Note that thromboelastography does not measure platelet adhesion, only platelet aggregation. (352)
28. Laboratory tests of fibrinolysis include fibrinopeptide and fibrin monomer levels, fibrin degradation products, and D-dimer levels. (352)
29. Elevated levels of fibrinopeptide or fibrin monomer are suggestive of intravascular coagulation. (352)
30. Elevated levels of fibrin degradation products are suggestive of conditions of intravascular fibrin deposition with resultant secondary fibrinolysis, such as disseminated intravascular coagulation. (352)
31. D-dimers are essentially a specific fibrin degradation product and are generated by the fibrinolytic activity of plasmin. Plasmin cleaves cross-linked fibrin. Fibrin monomers are cross-linked by factor XIII to form D-dimers. Elevated D-dimer levels are suggestive of some prior formation of cross-linked fibrin (i.e., clot) such as that caused by thrombotic or thromboembolic disorders. (352)
Disorders associated with altered hemostasis during surgery
32. Platelet counts of 50,000 cells/μL can be associated with uncontrolled intraoperative bleeding. (353)
33. In general, 20% to 30% of coagulation factors must be present to prevent uncontrolled intraoperative bleeding. (353)
34. Some diseases associated with an increased incidence of bleeding during surgery include hereditary and spontaneous coagulation factor deficiencies, hereditary and spontaneous platelet disorders, liver disease, renal disease, HELLP syndrome, acute immune thrombocytopenia, elevated plasma proteins, multiple myeloma, dysproteinurias, myeloproliferative disorders, coagulation factor inhibitors, and drugs. Examples of drugs include warfarin, heparin, aspirin, nonsteroidal antiinflammatory drugs, digitalis, thiazide diuretics, and ethyl alcohol. (353, Table 22-2)
35. Some diseases or conditions associated with an increased incidence of thrombosis during surgery include hereditary or spontaneous hypercoagulable states, anticoagulant or factor mutations, factor V Leiden, homocystinemia, dysfibrinogenemia, increased platelet turnover, prosthetic heart valves, antiphospholipid antibody, lupus anticoagulant, anticardiolipin antibody, and blood stasis and vascular damage. (353, Table 22-2)
36. Some diseases that are associated with initiating disseminated intravascular coagulation during surgery include crush injury, acute hemolytic transfusion reaction, abruption placentae, cardiopulmonary bypass, intravascular emboli, sepsis, liver disease, arterial hypoxemia acidosis, pancreatitis, immune complex disease, allergic reactions, transplant rejection, and cancer. (353, Table 22-2)
37. Some hereditary coagulation and platelet disorders include von Willebrand disease and deficiencies in factor VIII (hemophilia A), factor IX (hemophilia B or Christmas disease), factor XII, and factor XI. Of these, von Willebrand disease is the most common with a prevalence of 1% to 2% in some populations. (353, Table 22-3)
38. Hereditary coagulation disorders are treated with a specific factor concentrate or cryoprecipitate, as needed. Replacement therapy should aim to achieve 50% to 100% of normal factor levels perioperatively until wound healing is complete. (353-354)
39. Von Willebrand factor is stored in platelets. (354)
40. Von Willebrand factor has three important hemostatic functions. First, it mediates adhesion of platelets to the damaged vessel wall, or the subendothelium. Second, it is important in the adhesion of platelets to each other (platelet aggregation). Finally, it protects factor VIII from inactivation and clearance. (354)
41. Fibrin formation requires sufficient levels of factor VIII. If factor VIII levels are low (e.g., hemophilia A), fibrin formation is impaired. Von Willebrand factor protects factor VIII levels from clearance and thus factor VIII levels are low in certain forms of von Willebrand disease. (354)
42. Quantitative or qualitative deficits in von Willebrand factor results in dysfunctional platelet adhesion, dysfunctional platelet aggregation, and insufficient levels of factor VIII. The clinical effects of von Willebrand disease therefore are defective platelet plug formation and defective fibrin formation. (354)
43. Von Willebrand disease can be distinguished from factor VIII deficiency through the evaluation of the results of a bleeding time electrophoresis of von Willebrand antigens, ristocetin cofactor, or platelet function analysis tests. (355)
44. There are three types of von Willebrand disease. Type 1 is an insufficient quantity of von Willebrand factor. This type of von Willebrand disease is the most common, accounting for 70% to 80% of von Willebrands disease. Type 1 von Willebrand disease is associated with a decrease in factor VIII levels by 5% to 30%. Type 2 applies when there is a defect in the quality of von Willebrand factor. Type 3, which is rare, is when von Willebrand factor is absent entirely. Types 1 and 2 are autosomal dominant, while type 3 is autosomal recessive. (354, Table 22-4)
45. To most appropriately manage a surgical patient with von Willebrand disease, the type of disease must be determined. If necessary, a hematology consult should be obtained. Bleeding in the presence of von Willebrand disease can be treated with DDAVP, with the exception of type 3 and type 2B. Type 3 von Willebrand disease requires von Willebrand factor and factor VIII concentrates, as well as a platelet transfusion. In type 2B von Willebrand disease, DDAVP is actually contraindicated because of transient thrombocytopenia after its administration. If the patient has a type of von Willebrand disease that should respond to DDAVP, the dose that should be administered is 0.3 μg/kg 1 hour before incision. (355)
46. DDAVP should be administered very cautiously or not at all to patients with unstable coronary artery disease. When DDAVP is administered, there can be an increase in platelet aggregation at sites of high shear stress, such as at coronary narrowing. This can precipitate platelet plug formation and thus increase the risk for myocardial infarction in these patients. (355)
47. There are alternative treatment options of patients with von Willebrand disease if DDAVP is not available. These include cryoprecipitate and intermediate purity concentrates of factor VIII. Cryoprecipitate contains large amounts of von Willebrand factor and factor VIII, both of which are low in patients with von Willebrand disease. Intermediate purity concentrates of factor VIII used for the treatment of hemophilia A should also work, since these contain large amounts of von Willebrand factor. High purity (recombinant) factor VIII preparations that do not contain von Willebrand factor are not useful. (355)
48. Vitamin K is a cofactor in an enzymatic reaction necessary for the production of certain coagulation factors. (355)
49. Factors II, VII, IX, and X, as well as protein C and protein S are vitamin K dependent coagulation factors. (355)
50. If intestinal absorption is impaired (ileitis, celiac disease, etc.) or bacterial production of vitamin K is decreased (antibiotic therapy), or both of these circumstances are present, vitamin K deficiency could develop. (355)
51. Factor VIII is made in lung endothelial cells. All other coagulation factors are synthesized in the liver. (355)
52. Decreased coagulation factor levels, increased fibrinolysis (liver degrades plasmin), and splenic platelet sequestration in patients with portal hypertension can all contribute to the increased risk of bleeding in patients with severe liver disease. (355)
53. There are several diseases or conditions that are associated with acquired antibodies to coagulation factor VIII. Patients with hemophilia A (factor VIII deficiency), who have undergone longstanding factor VIII replacement, occasionally develop antibodies against that factor. Also, rheumatoid arthritis, ulcerative colitis, and old age have all been associated with antibodies against factor VIII. Clinically, these patients may have severe bleeding after minor injury. (355)
54. Some causes of peripheral platelet destruction include viral infections, chronic lymphocytic leukemia, lymphoma, colon cancer, collagen vascular disease, multiple blood transfusions, and drugs such as heparin, quinine, quinidine, digitoxin, and thiazides. (355, Table 22-5)
55. Some causes of thrombocytopenia that can occur during pregnancy include gestational thrombocytopenia, preeclampsia, and HELLP syndrome. (355)
56. Normally about one third of platelets are sequestered in the spleen, where they remain until times of vascular stress when they are released into the circulation. During pathologic splenic sequestration states, the spleen does not release platelets into the circulation, and splenomegaly and thrombocytopenia result. (355-356)
57. There are a number of situations in which the number of platelets may be adequate, but they are defective such that there is an increased risk of bleeding. Impaired platelet function can be seen in uremia, and in the presence of some drugs such as aspirin, nonsteroidal antiinflammatory agents, and alcohol. Platelet function is also impaired when there are high levels of circulating fibrin-fibrinogen split products, as can occur with severe liver disease, in disseminated intravascular coagulation, and with therapeutically induced fibrinolysis such as with the treatment with urokinase. Platelet dysfunction also occurs in conditions in which there are high levels of abnormal serum proteins, such as multiple myeloma, dysproteinemias, or transfused dextran infusions. (356)
58. Some intraoperative conditions that may facilitate bleeding include hypothermia, acidosis, anemia, and hemodilution. (356)
59. Hypothermia with temperatures of 34° C or less is associated with poor platelet function and decreased procoagulant activity. (356)
60. Anemia and hemodilution can both cause a coagulopathy. Increasing anemia results in decreasing plasma viscosity. The formation and strength of hemostatic plugs are impaired in the presence of low plasma viscosity. Aggressive intravenous fluid resuscitation can dilute plasma coagulation factors and platelet numbers below amounts needed for effective hemostasis. (355)
Disorders favoring thrombosis
61. Some factor deficiencies that are inherited can lead to a hypercoagulable state. These may include antithrombin, protein C, protein S, or factor V. Inheritance of these deficiencies may lead to deep vein thrombosis and pulmonary embolism. (356)
62. Factor V Leiden is a disease in which factor V has qualitative abnormalities. The patients are resistant to activated protein C. Normally protein C activated by thrombin, in the presence of thrombomodulin, inactivates factor V, limiting thrombin production. Therefore patients with factor V Leiden are somewhat hypercoagulable and are prone to thrombosis. (356)
63. Antiphospholipid syndrome is a heterogeneous group of syndromes that manifests as venous and arterial microvascular thromboses. Antiphospholipid syndrome describes an autoimmune production of antibodies against phospholipids in cell membranes. When antiphospholipid syndrome occurs in isolation, it is called primary antiphospholipid syndrome. Antiphospholipid syndrome most commonly occurs in conjunction with another autoimmune disease. (356)
64. Lupus anticoagulant is a type of phospholipids antibody. About 5% to 10% of patients with systemic lupus erythematosus have lupus anticoagulant. These patients are at an increased risk for perioperative thromboses. (356)
65. In patients with lupus anticoagulant the partial thromboplastin time is prolonged and the prothrombin time is normal to slightly prolonged. This would suggest that a bleeding disorder is present (lupus anticoagulant) when, in fact, the patient is prone to thrombosis. (356)
66. Virchow triad is the combination of venous stasis, hypercoagulability, and vascular damage. All of these conditions are typically present in the perioperative period. (356)
67. Disseminated intravascular coagulation (DIC) is an acquired disorder characterized by uncontrolled intravascular coagulation and fibrinolysis with bleeding and thrombosis. Generalized intravascular thrombin generation and fibrin deposition in small blood vessels lead to the formation of microvascular thrombi. Tissue hypoxia and multiorgan failure follow. Normal regulatory control of thrombin and plasmin is impaired, thereby allowing these proteolytic enzymes to activate and consume circulating coagulation factors, fibrinogen, and platelets. (356)
68. The laboratory findings in DIC reflect the pathophysiology of the condition, which is the concurrence of thrombus formation and fibrinolysis with consumption of coagulation factors. The combination of a decreased platelet count, decreased fibrinogen, prolonged PT and PTT, and elevated fibrin degradation products or D-dimers is present in DIC. Once elevated, D-dimers remain increased for days, thus making serial test measurements more sensitive and specific than single measurements. (356)
69. Both fibrin degradation products and D-dimers are elevated with trauma or recent surgery, and with liver and kidney disease. Coagulation test results in patients with severe liver disease may be similar to those in patients with DIC, although D-dimer levels may not be as high and platelet counts not as low. Factor VIII activity is helpful in discriminating between these conditions because factor VIII is consumed in DIC and factor VIII levels are normal or elevated in liver disease. (356-357)
70. The most definitive treatment of DIC is removal of the stimulus causing DIC. Other treatment of DIC is a matter of controversy. Generally, treatment is supportive with replacement of factors and platelets as needed. This has previously been contested as “fueling the fire” but there is no evidence that factor replacement worsens DIC and common sense dictates that replacement of consumed products is necessary to minimize bleeding complications. Heparin has been suggested as a treatment option with the rationale that DIC, when primarily caused by uncontrolled coagulation, may be halted when coagulation is inhibited. This approach is also currently not supported by clinical evidence. (357)
Anticoagulants, thrombolytics, and antiplatelet drugs
71. Perioperative thrombotic events include deep vein thrombosis, pulmonary embolism, stroke, and myocardial infarction. (357)
72. Generally, drugs against perioperative thrombotic complications either prevent (anticoagulants, antiplatelet drugs) or treat (thrombolytics) thrombus formation. Since venous thrombosis starts with activation of the coagulation cascade, it seems logical to aim to prevent thrombus formation by inhibiting some aspect of the coagulation system with anticoagulants. Since arterial thrombus formation starts with platelet adhesion, it seems logical to primarily target that process with antiplatelet drugs. (357)
73. Anticoagulants in clinical use include heparin, LMWH parin, fondaparinux, warfarin, direct thrombin inhibitors, and a recently FDA-approved oral direct thrombin inhibitor. These drugs could potentially replace warfarin as oral anticoagulants. (357)
74. Warfarin is a vitamin K antagonist. Warfarin exerts its effect through the inhibition of an enzyme that recycles vitamin K (vitamin K epoxide reductase). Warfarin thus causes a state similar to vitamin K deficiency. (357)
75. Initiation of the anticoagulant and antithrombotic effects of warfarin depends on the plasma factor VII concentration because factor VII has the shortest half-life (3 to 6 hours). Several factor half-lives are required to deplete factor VII to the 20% to 30% level needed for effective anticoagulation. Therefore, despite oral warfarin reaching effective plasma concentrations in 90 minutes, full anticoagulant efficacy does not develop until several days later. (357)
76. Heparin coadministration during the first 5 days of warfarin therapy is necessary for two reasons. First, the anticoagulant activity of warfarin does not develop for several days. Second, since the plasma half-life of protein C is only 6 to 10 hours, a hypercoagulable state due to uninhibited thrombin formation can initially develop when warfarin therapy is commenced. This is prevented by heparin coadministration. (357)
77. Warfarin therapy is monitored with the measurement of the prothrombin time (INR). Warfarin has a very narrow therapeutic window between bleeding and the prevention or treatment of thrombosis. In addition, drugs, foods, and alcohol can profoundly alter the pharmacokinetic profile of warfarin. Therefore, it is necessary to monitor warfarin therapy. This is in contrast to the more modern anticoagulants such as oral direct thrombin inhibitors, which require no monitoring. (357)
78. Some advantages of unfractionated heparin therapy over low LMWH or pentasaccharide (fondaparinux) drugs include its immediate onset, efficacy against thrombin, short half-time of 30 to 60 minutes, and reversibility with protamine. These characteristics of heparin therapy make it more useful for administration intraoperatively than LMWH or fondaparinux. (357)
79. Unfractionated heparin therapy needs to be closely monitored because of its unpredictable pharmacokinetics. Heparin binds to plasma proteins, macrophages, endothelial cells, and proteins released from activated platelets and endothelial cells. This variation in the available free heparin in plasma makes its necessary to monitor heparin therapy with laboratory tests. (357)
80. Unfractionated heparin has unpredictable pharmacokinetics caused by heparin binding to plasma proteins, macrophages, endothelial cells, and proteins released from activated platelets and endothelial cells. These properties are a function of the saccharide chain length, which is greater for unfractionated heparin than for LMWH or pentasaccharide drugs. Therefore these shorter drug preparations do not require monitoring with partial thromboplastin time. (357)
81. The efficacy of unfractionated heparin is monitored using the partial thromboplastin time. Heparin given intraoperatively can be monitored through measurement of the ACT. (357)
82. Cardiac surgery, vascular surgery, and percutaneous interventional procedures such as neuroangiography and cardiac arrhythmic tract ablations are some procedures in which heparin is administered to prevent clotting. The degree of anticoagulation required with heparin varies in these procedures. In cardiac surgery, heparin is administered to achieve a level of anticoagulation that would allow cannulation for cardiopulmonary bypass without risking clot formation in the bypass circuit. To achieve this level of anticoagulation 300 to 400 U/kg of unfractionated heparin is usually required, and the goal for treatment usually requires an ACT of greater than 400 seconds. Most vascular and percutaneous procedures require lower levels of heparin anticoagulation; for these procedures the goal is to achieve an ACT of twice baseline or less. (357)
83. Heparin anticoagulation during surgery is reversed through the administration of protamine. The dose of protamine for this purpose is 1 mg for every 100 units of heparin that has been administered. Protamine binds to heparin and reverses its effect. (357)
84. A negative effect of protamine is its potential to cause a significant histamine release manifested as bronchoconstriction, and a decrease in systemic vascular resistance resulting in hypotension. Protamine administration can also cause pulmonary hypertension. The pulmonary hypertension that can result from the administration of protamine can be severe in rare cases. (357-358)
85. Heparin-induced thrombocytopenia and osteopenia are two potential side effects of the administration of heparin that are directly related to the number of saccharide residues and therefore occur with lower frequency or not at all with LMWH or pentasaccharide drugs. (358)
86. HIT is characterized by a decrease in platelet count after initiation of heparin therapy. HIT type 1 is not mediated by immunoglobulin G (IgG), is self-limited, and does not require intervention. HIT type 2 is the most feared nonhemorrhagic complication of heparin treatment and is usually due to antiplatelet factor 4 antibodies causing platelet aggregation. (358, Table 22-6)
87. HIT type 2 is a clinical diagnosis, which requires a decrease in the platelet count to less than 100,000 cells/μL or less than 50% of baseline 5 to 10 days after the initiation of heparin therapy. There is a recovery of the platelet count after discontinuation of heparin. Heparin-platelet factor 4 antibody testing confirms the diagnosis. (358)
88. HIT type 2 occurs with an incidence of 1% to 3% among patients treated with heparin. The mortality rate for patients with HIT type 2 is 20% to 30%. (358)
89. Heparin-induced thrombocytopenia type 1 does not require any special therapeutic intervention, since the condition is self-limiting. Heparin-induced thrombocytopenia type 2 requires cessation of all heparin, including heparin flushes or heparin-coated central venous catheters. An alternative form of anticoagulation must be sought (e.g., direct thrombin inhibitors). (358)
90. Heparin resistance is present when the usual heparin doses do not result in adequate prolongation of the partial thromboplastin time or ACT. Insufficient antithrombin or excessive heparin-binding proteins (factor VIII, fibrinogen, and other acute-phase proteins) are thought to be the cause. (358)
91. Heparin resistance can be treated initially with additional doses of heparin. If insufficient anticoagulation persists after the administration of additional heparin, fresh frozen plasma may be used in an attempt to increase plasma concentrations of antithrombin. (358)
92. LMWH and pentasaccharide drugs, unlike unfractionated heparin, do not directly inhibit thrombin. Eighteen saccharide subunits (pentasaccharide plus 13 additional subunits) are required to bridge the gap between antithrombin and thrombin. LMWH, by definition, is any heparin molecule that does not have the sufficient saccharide chain length to inhibit thrombin. (358)
93. Any drug containing the pentasaccharide subunit that is shared by unfractionated heparin, LMWH, and pentasaccharide binds antithrombin. Antithrombin inhibits factor Xa, regardless of its activity against thrombin. This confers the anticoagulant efficacy of LMWH and pentasaccharide. (358)
94. LMWH and pentasaccharide drugs have a slower onset time (20 to 60 minutes) but a longer half-time than heparin. This allows for once or twice a day administration and it can be administered subcutaneously. In addition, the predictable pharmacokinetics of LMWH and pentasaccharide drugs makes laboratory monitoring of its efficacy unnecessary. Thus, these drugs are easier to manage on an outpatient basis. LMWH and pentasaccharide drugs also have lower to nonexistent risks of osteopenia and heparin-induced thrombocytopenia. One disadvantage of LMWH and pentasaccharide drugs is that they have an increased risk of bleeding complications when compared to unfractionated heparin. Another disadvantage is the inability to reverse the effects of these drugs with protamine. (358)
95. There are three intravenous direct thrombin inhibitor drugs in current clinical use. These are hirudin, argatroban, and bivalirudin. There is also one oral direct thrombin inhibitor drug, dabigatran, which was FDA approved in October of 2010 for the treatment of atrial fibrillation. (358)
96. Compared to unfractionated heparin at equipotent doses, direct thrombin inhibitors are associated with an exceedingly high risk of bleeding. In addition, no reversal agent exists for this group of drugs. (358-359)
97. If systemic anticoagulation is required in a patient with a recent history of HIT type 2, the surgery could be delayed until such time as the antiplatelet factor 4 antibodies, which are thought to be responsible for the thrombotic complications of HIT type 2, have disappeared. This will usually take 3 to 4 months. If that is considered unacceptably long, plasmapheresis can be used in an attempt to eliminate the antiplatelet factor 4 antibodies. (359)
98. Thrombolytic drugs currently used in clinical practice include streptokinase and urokinase, alteplase, and tenecteplase. Streptokinase and urokinase are native tissue plasminogen activators, while alteplase and tenecteplase are exogenous tissue plasma activators. (359)
99. The mechanism of action of thrombolytic drugs is through the activation of plasmin. Exogenous tissue plasminogen activators are more fibrin sensitive. All tissue plasminogen activators are both thrombolytics and anticoagulants since fibrinolysis generates increased amounts of circulating fibrin degradation products. This inhibits platelet aggregation. (359)
100. Surgery or puncture of noncompressible vessels is contraindicated within a 10-day period after the administration of thrombolytic drugs. (359)
101. Antiplatelet drugs are classified by their mechanism of action, such as cyclooxygenase inhibitors, thienopyridine derivates, and GPIIb/IIIa antagonists. Cyclooxygenase inhibitors include nonselective inhibitors such as aspirin or nonsteroidal antiinflammatory drugs, such as ibuprofen, diclofenac, and naproxen. Selective cyclooxygenase-2 inhibitors include valdecoxib and celecoxib. Examples of thienopyridine derivatives are ticlopidine and clopidogrel. Examples of GPIIb/IIIa antagonists are abciximab, eptifibatide, and tirofiban. (359)
102. Aspirin inhibits platelet granule release irreversibly for the life of the platelet. Platelet function recovers by means of replacing inhibited platelets with newly generated and thus functional platelets. Nonsteroidal antiinflammatory drugs reversibly inhibit platelets with return of normal platelet function within 3 days after drug administration. Cyclooxygenase-2 inhibitors do not affect platelet function. (359)
103. The thienopyridine derivatives clopidogrel and ticlopidine inhibit the binding of platelets to fibrinogen. This results in an inhibition of platelet aggregation. (359)
104. Platelet functions normalize 7 days after discontinuing clopidogrel, and 14 to 21 days after discontinuing ticlopidine. (359)
105. The platelet GPIIb/IIIa receptor mediates platelet aggregation by allowing the binding of platelets to fibrinogen or von Willebrand factor. GPIIb/IIIa antagonists are therefore potent inhibitors of platelet aggregation. (359)
106. Platelet aggregation normalizes 8 hours after discontinuing eptifibatide and tirofiban, and 24 to 48 hours after discontinuing abciximab. (359)
An approach to patients who are anticoagulated
107. Patients on warfarin undergoing surgery are challenging to manage perioperatively. On the one hand, the anticoagulant could predispose to bleeding complications if it is not discontinued far enough in advance of the surgery. On the other hand, when the anticoagulant is discontinued, it adds to the overall risk of thrombotic complications, which can have devastating consequences. The risk of bleeding is a function of reversal of the drug effect with time, which is assessed by the INR. The risk for a thrombotic complication after stopping warfarin therapy depends on the surgical procedure, the original indication for warfarin therapy, and the degree of the rebound hypercoagulable state associated with warfarin cessation. This risk is assessed jointly by a multidisciplinary team. (359)
108. Major abdominal and cardiothoracic procedures generally carry the highest risk of perioperative thrombosis. (359)
109. Patients on chronic warfarin therapy who have had a venous thrombotic or arterial embolic event within a month before surgery, or who have mitral or cage valve prosthesis are at a high risk of perioperative thrombosis regardless of the type of surgery. (359, Figure 22-2)
110. Patients on chronic warfarin therapy who have had a venous thrombosis less than 2 to 3 months prior, with atrial fibrillation with a history of prior embolism or with recurrent venous thrombosis, are at an intermediate risk of perioperative thrombosis regardless of the type of surgery. (360, Figure 22-2)
111. Patients on chronic warfarin therapy who have atrial fibrillation without a history of prior embolism, or who have a valve prosthesis other than mitral or cage prosthesis, are at a low risk of perioperative thrombosis regardless of the type of surgery. (360, Figure 22-2)
112. It is important to stratify the risk of perioperative thrombosis for patients on chronic warfarin therapy because patients must be managed differently with regard to anticoagulation in the perioperative period based on their risk of thrombosis. (359, Figure 22-2)
113. Patients on chronic warfarin therapy at high risk for a perioperative thrombosis should be managed differently with regard to anticoagulation in the perioperative period than those at a low or intermediate risk of thrombosis. In either case, the warfarin is discontinued 5 days before surgery. However, patients at a high risk for thrombosis receive an intravenous unfractionated heparin infusion that is closely monitored as an inpatient. All others can receive bridging therapy as an outpatient using either LMWH or pentasaccharide. Postoperative anticoagulation starts 12 hours after hemostasis has been achieved in either case, but high-risk patients receive either an intravenous infusion of unfractionated heparin or LMWH, or pentasaccharide for a full 5 days while warfarin therapy is reinitiated early and as an inpatient. Patients with intermediate or low risk for thrombosis can be treated with subcutaneously injected unfractionated heparin, LMWH, or pentasaccharide as an outpatient and warfarin can be recommenced electively. (359-360, Figure 22-2)
114. In a patient receiving perioperative heparin bridging therapy for warfarin treatment, the intravenous heparin infusion is discontinued 6 hours prior to surgery and should not be restarted before 12 hours after hemostasis is achieved. (359)
115. In a patient receiving perioperative LMWH bridging therapy for warfarin treatment, LMWH is discontinued 12 hours before surgery and restarted 12 hours after hemostasis is achieved. (359)
116. Patients with a high likelihood of perioperative bleeding should likely not be administered heparin in the perioperative period. This may include patients with thrombocytopenia or concurrent antiplatelet therapy, or patients with a history of bleeding in the gastrointestinal, genitourinary, or central nervous system. (359-360)
117. For the emergency surgical patient on chronic warfarin therapy, the administration of fresh frozen plasma or prothrombin complex concentrate will restore the concentration of vitamin K dependent coagulation factors, and thus reverse the effects of warfarin. Vitamin K dependent coagulation factors are quickly restored with these products. (360)
118. The administration of oral vitamin K should be considered for the emergency patient on chronic warfarin therapy who is receiving fresh frozen plasma or prothrombin complex to reverse the effects of warfarin because of the half-life of these products. The restoration of vitamin K dependent coagulation factors by transfusion of these products is immediate, but the duration of the effect is only 4 to 6 hours. Thus oral vitamin K at a dose of 1 mg should be administered concomitantly. (360)
119. Vitamin K is administered at 1 mg orally in addition to intravenous infusions of fresh frozen plasma or prothrombin complex concentrate in patients on warfarin that require emergency surgery. The subcutaneous or intramuscular routes can have prolonged action and can make postoperative warfarin therapy challenging. Intravenous vitamin K is associated with a greater risk of anaphylaxis. (360)
An approach to patients receiving antiplatelet therapy
120. Patients with bare metal coronary stents require antiplatelet therapy for at least 4 months after stent placement. (360)
121. Patients with drug-eluting coronary stents require antiplatelet therapy for at least 12 months after stent placement. (360)
122. Drug-eluting coronary stents are designed to retard intimal hyperplasia, but in so doing they also delay the formation of an antithrombotic intimal layer. The intimal layer forms very slowly in the area of the drug-eluting stent, and this intimal layer confers the anticoagulant property of the vessels. Hence patients with drug-eluting coronary stents are at much greater risk for perioperative myocardial infarctions when the antiplatelet therapy is stopped than those with bare metal coronary stents. (360-361)
123. Patients with coronary stents that require antiplatelet therapy should have their elective surgical procedure postponed until the antiplatelet therapy is no longer recommended. In cases in which the surgery cannot be postponed, the risks of bleeding and thrombosis need to be carefully weighed often by a multidisciplinary approach including the cardiologist, surgeon, and anesthesiologist. If the risk of thrombosis is high, bridging therapy with a short-acting antiplatelet agent may be indicated. (361, Figure 22-3)
Neuraxial interventions in patients being treated with anticoagulant drugs
124. There is a risk of bleeding and neurologic injury in patients who are undergoing neuraxial interventions while receiving anticoagulant drug therapy. The management of these patients should be guided by the recommendations of the American Society of Regional Anesthesia, who have provided algorithms for management for each type of anticoagulant drug. (361, Table 22-7)
An intraoperative approach to uncontrolled bleeding
125. In the absence of laboratory testing during the massive transfusion of packed red blood cells, fresh frozen plasma is generally indicated after the replacement of about one blood volume. Platelets are generally indicated after the replacement of about two blood volumes. (361)
126. During ongoing blood loss, a prothrombin time of 1.5 times the normal range or greater would indicate the need for the replacement of coagulation factors with fresh frozen plasma. (361)
127. During ongoing blood loss, a platelet count lower than 50,000 to 80,000 cells/μL would indicate the need for the replacement of platelets with a transfusion of concentrated platelets. (361-362)
128. During ongoing blood loss, a fibrinogen level of less than 125 mg/dL would indicate the need for a transfusion of cryoprecipitate. Cryoprecipitate (one concentrate per 10 kg of body weight) can be used to augment fibrinogen. However, each fresh frozen plasma and platelet pheresis unit has approximately twice the amount of fibrinogen contained in one cryoprecipitate concentrate. (362)
129. An indication for the transfusion of cryoprecipitate would be to treat a low fibrinogen level in small children. Also, a cryoprecipitate transfusion is appropriate when factor VIII or von Willebrand factor needs to be replaced specifically. (362)
130. Recombinant factor VIIa has been designed and licensed for the treatment of bleeding in hemophilia patients. It has also been used off-label in patients with life-threatening, uncontrolled intraoperative bleeding unresponsive to conventional therapy. It is of unproven benefit and extremely expensive. (363)
131. Other hemostatic drugs used perioperatively include DDAVP and the lysine analogs antifibrinolytics, ε-aminocaproic acid and tranexamic acid. DDAVP (0.3 μg/kg IV) releases von Willebrand factor from endothelial cells and the lysine analogues inhibit fibrinolysis. (362)
132. DDAVP has proven useful for the prevention of bleeding in some forms of von Willebrand disease. It is also useful in mild forms of factor VIII deficiency and for bleeding associated with uremia. (362)