CHAPTER 35 Hemi-resection Interposition Arthroplasty
In the setting of advanced articular involvement of the distal radioulnar joint (DRUJ), a salvage or ablative procedure is recommended. Ablative procedures of the distal ulna include the hemi-resection interposition technique (HIT) arthroplasty,1 the Sauvé-Kapandji procedure,2 the matched resection,3 and the Darrach procedure.4 The author has no personal experience with the matched resection procedure, but it is conceptually similar to the HIT procedure. Implant arthroplasty of the DRUJ is yet another alternative, and favorable early results have been reported using the implant developed by van Schoohoven and colleagues in the setting of a failed salvage procedure.5
The HIT procedure was developed by William H. Bowers in 1981 as an integral part of managing the rheumatoid ulnar wrist. The principle of the procedure is to maintain a strong soft tissue connection of the ulna to the carpus and radius while removing the damaged joint surface. Although originally designed primarily for the rheumatoid wrist, the HIT procedure has also been used successfully in the nonrheumatoid wrist and, in particular, as a reconstructive option in the setting of distal radial malunion.6–8 It has also been successfully employed in patients affected by symptomatic, primary osteoarthritis of the DRUJ.
Caveats
Conceptually, the HIT procedure preserves the ulnocarpal ligament complex, thus maintaining some stability while simultaneously addressing the problematic DRUJ by removing the involved distal ulnar articular surface. Thus, the resection involves resection of the ulnar articular head while the shaft/styloid relationship is left intact. The ideal nonrheumatoid candidate presents with a painful distal radioulnar joint with or without a distal radius malunion. The procedure is rarely indicated in the acute setting. The TFCC can be partially deficient, but it must be able to be repaired. It is best if the TFCC is intact; and if it is neither intact nor can be repaired, the procedure offers no advantages over a Darrach procedure. The HIT procedure may also be successfully utilized in the setting of a partially treated distal radius fracture associated with a fracture of the ulnar styloid with associated dislocation of the distal ulna (Fig. 35-1).
The HIT Arthroplasty
The procedure is typically performed utilizing general or regional anesthesia under arm tourniquet control. Prophylactic antibiotics are recommended. If a distal radius osteotomy is required, it is recommended that this be performed first. A separate incision is most often required in this setting.
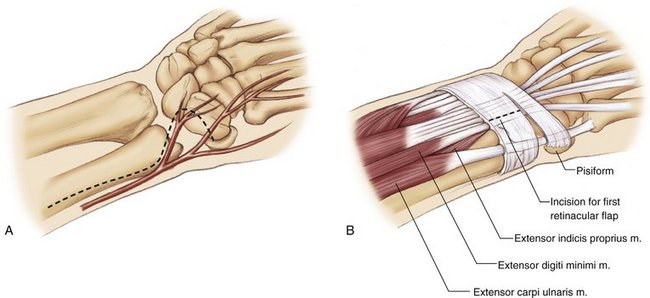
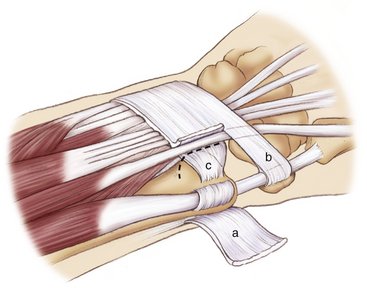
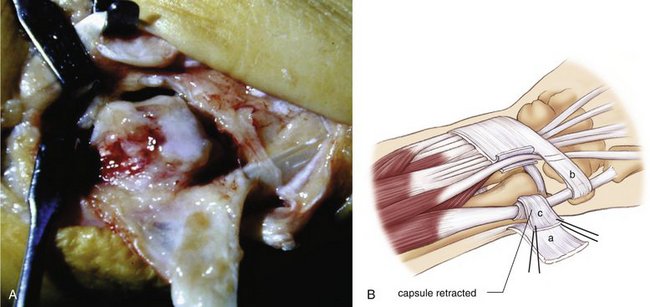
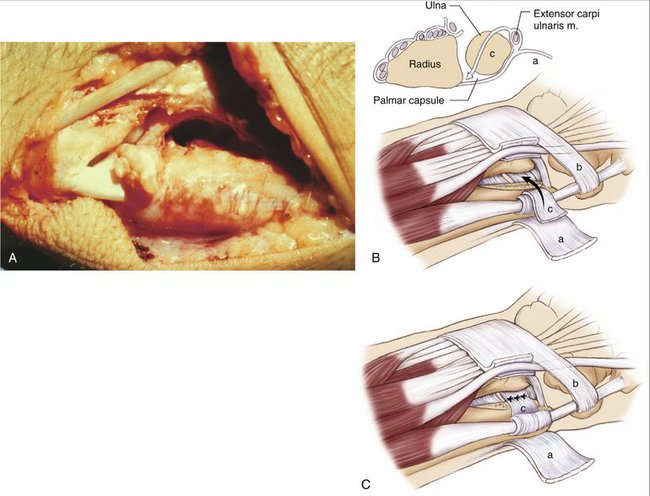
With the forearm pronated, an angled or straight incision is made over the distal ulna (Fig. 35-2). The incision lies dorsal to the dorsal sensory branches of the ulnar nerve. Care is taken to preserve these small branches, which often include both transverse and oblique branches around the DRUJ. The ulnar head presents beneath the retinaculum, between the extensor carpi ulnaris and the extensor digiti minimi (Fig. 35-3). The extensor digiti minimi is used as a guide for fashioning the retinacular flap. In a nonrheumatoid wrist it is recommended that both the retinacular and capsular flaps be ulnar based (Fig. 35-4). The retinaculum is incised over the extensor digiti minimi, retracting the tendon radialward. Once the tendon is retracted, the dorsal margin of the sigmoid notch, the DRUJ capsule, and the TFCC are easily identified. The capsule is then detached from the radius reflecting it ulnarward, leaving a 1-mm cuff for possible later repair (Fig. 35-5). The capsule is dissected along the head of the ulna subperioseally beneath the extensor carpi ulnaris sheath. For more distal exposure, the distal aspect of the dorsal retinaculum can also be reflected as an ulnarly based flap, with care taken to avoid disrupting the dorsal fibers of the TFCC (Fig. 35-6). In the nonrheumatoid wrist, it is not necessary to violate the extensor carpi ulnaris subsheath.
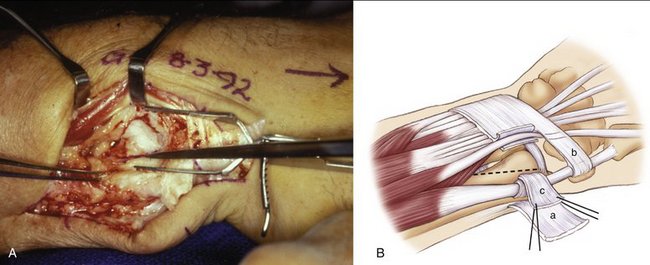
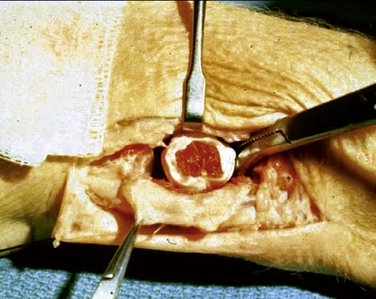
At this point, if the articular surface is sufficiently involved, the ulna articular surface is removed with small, flat osteotomes and a rongeur (Figs. 35-6 and 35-7). I recommend starting with a flat osteotome from distal to proximal, removing the dorsal half of the ulna head. Care is taken to ensure that the foveal attachment of the TFCC is not disrupted. A second oblique cut is then made once again from distal to proximal after rotating the forearm. It is typically necessary to make a third cut from proximal to distal once again using a small, flat osteotome. This “third cut” removes the palmar portion of the head, which is easy to miss if one is not careful. A rasp or small rongeur is used to smooth out the remaining bone. The remaining shaft/styloid axis should be round in cross section and resemble a tapering 1-cm diameter dowel. A small laminar spreader is used to facilitate exposure to be sure an adequate resection has been performed, particularly volarward. All osteophytes around the sigmoid notch and all the bone of the ulnar head beneath the articular surface must be excised. Inadequate bone removal can result in a clinical failure.
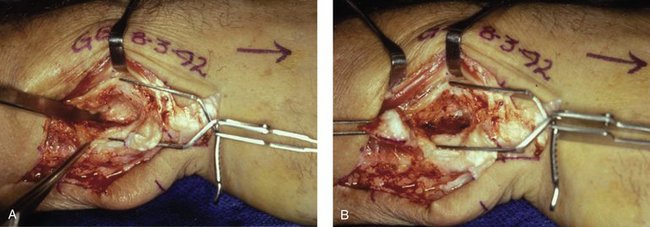
FIGURE 35-7 A, The third cut is from proximal to distal, once again using the same flat osteotome. B, Resected specimen.
After completing the bony resection, all remaining synovium is excised and the integrity of the TFCC is inspected. If necessary, the articular disc can be débrided at this point. An assessment of stylocarpal impingement is then performed, typically with the aid of a portable fluoroscopy unit (Fig. 35-8). While under fluoroscopy, the radius and ulna are compressed and rotated with the wrist in ulnar deviation. If one remains concerned that the styloid will impinge on the carpus, options include interposing a tendon “anchovy,” such as the palmaris longus (Fig. 35-9), or performing an ulnar shortening for more obvious degrees of impingement. Available expendable tendons would include the palmaris longus (most common), one half of the flexor carpi radialis, the extensor indicis proprius, or a long toe extensor. The tendon graft is rolled into a ball around a straight clamp and sutured with absorbable 3-0 Vicryl sutures to keep it intact. It is then placed into the cavity after the partial ulnar head resection and sutured to the volar capsule and pronator quadratus to prevent displacement. The dorsal capsule is then anatomically repaired back to the septum between the extensor digiti minimi and the DRUJ.
If one decides that an anchovy is inadequate to prevent impingement and that an ulnar shortening is required, it can be performed at one of three locations. The first and most straightforward location is at the tip of the styloid. This is useful in those cases in which there is a long, hooked styloid. In this instance, the distal aspect of the styloid is exposed and excised. Preservation of the deep fibers of the TFCC attached to the fovea preserves DRUJ stability. The second option is a shortening through the metaphyseal base of the ulnar head at the proximal margin of the head excision, with excision of a wedge of bone and fixation using a compression interosseous wire loop (Fig. 35-10). This is technically more demanding. The final alternative is a formal shortening through the proximal ulnar shaft and plate fixation. This is typically recommended when the preoperative ulnar-positive variance is greater than 3 to 4 mm. When considering stylocarpal impingement, the preoperative variance radiographs are critical. The variance is best determined by an anteroposterior pronated grip radiograph.9 In borderline cases (preoperative variance between neutral and 2 mm positive), an anchovy may be utilized, but in most cases the capsule and retinaculum are the only materials interposed and are sutured to the volar capsule (Fig. 35-11).
Complications
The most common complication involves stylocarpal impingement. It does not typically occur if it is anticipated and dealt with at the primary procedure. Another potential complication is painful and/or restricted forearm rotation. In the absence of stylocarpal impingement, this is usually the result of inadequate bony resection. Computed tomography obtained in full pronation/supination can be helpful in this regard. Another potential complication involves painful instability of the remaining distal ulna. Because of the lack of the “ulnar seat,” some degree of instability is inevitable. Most often, however, this does not result in significant symptoms.
1. Bowers WH. Distal radioulnar joint arthroplasty: the hemiresection-interposition technique. J Hand Surg [Am].. 1985;10:169-178.
2. Sauvé L, Kapandji M. Nouvelle technique de traitment chirurgical des luxations récidivantes isolées de l’extrémité inférieure du cubitus. J Chir (Paris).. 1936;47:589-594.
3. Watson HK, Gabuzda GM. Matched distal ulnar resection for posttraumatic disorders of the distal radioulnar joint. J Hand Surg [Am].. 1992;17:724-730.
4. Darrach W. Anterior dislocation of the head of the ulna. Ann Surg.. 1912;56:802-803.
5. Van Schooven J, Fernandez DL, Bowers WH, Herbert TJ. Salvage of failed resection arthroplasties of the distal radioulnar joint using a new ulnar head prosthesis. J Hand Surg [Am].. 2000;25:438-446.
6. Van Schoohoven J, Kall S, Schober F, et al. The hemiresection-interposition arthroplasty as a salvage procedure for the arthrotically destroyed distal radioulnar joint. Handchir Microchir Plast Chir.. 2003;35:175-180.
7. Bowers WH. Distal radioulnar joint arthroplasty: current concepts. Clin Orthop Relat Res.. 1992;275:104-109.
8. Fernandez DL. Radial osteotomy and Bowers arthroplasty for malunited fractures of the distal end of the radius. J Bone Joint Surg Am.. 1988;70:1538-1551.
9. Tomaino MM. The importance of the pronated grip x-ray. J Hand Surg [Am].. 2000;25:352-357.