Heineke-Mikulicz Pyloroplasty and Duodenotomy for Bleeding Ulcer
Principles of Treatment
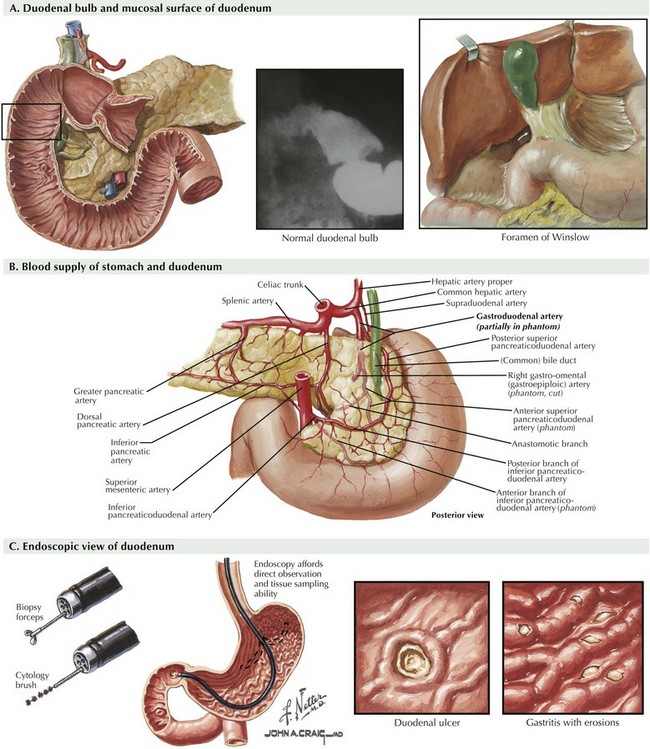
Duodenal ulcers that result in bleeding are usually positioned in the posterior duodenal bulb (Fig. 9-1, A). There are numerous submucosal arterial vessels around the duodenum, but invasion of the gastroduodenal artery is the predominant source for massive duodenal ulcer bleeding (Fig. 9-1, B).
After stabilization of the patient, the first diagnostic (and often therapeutic) intervention is upper endoscopy (Fig. 9-1, C). Multiple endoscopic adjuncts for providing hemostasis are available, including clips, cautery, and injection of sclerotherapy agents. If these endoscopic approaches are unsuccessful and the patient continues to have evidence of bleeding from an identified duodenal ulcer, radiologic interventions are typically used. The gastroduodenal artery is accessed with transarterial catheters through the celiac trunk, and the site of bleeding is then identified and treated with a combination of intraluminal coils, foams, and autologous clots. Vasoactive medications can also be delivered by a subselective catheter left in place with its tip into the gastroduodenal artery to assist in hemostasis.
Surgical Approach
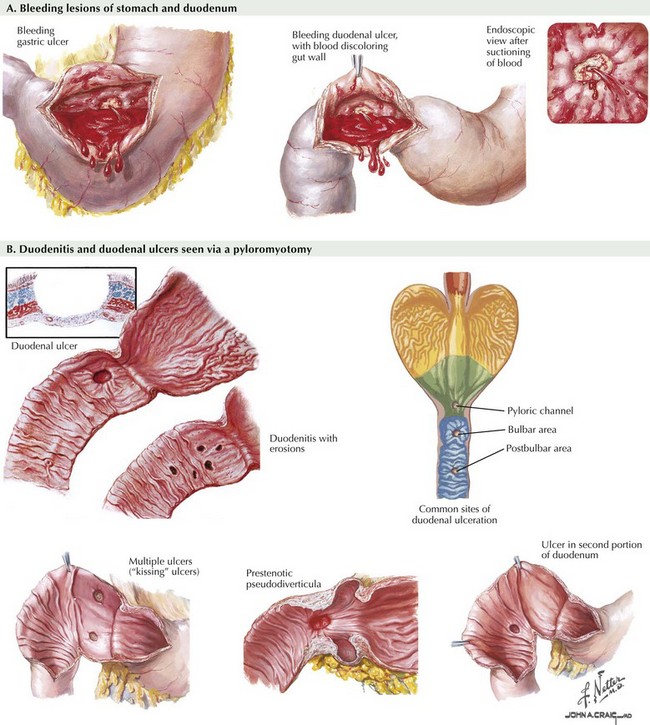
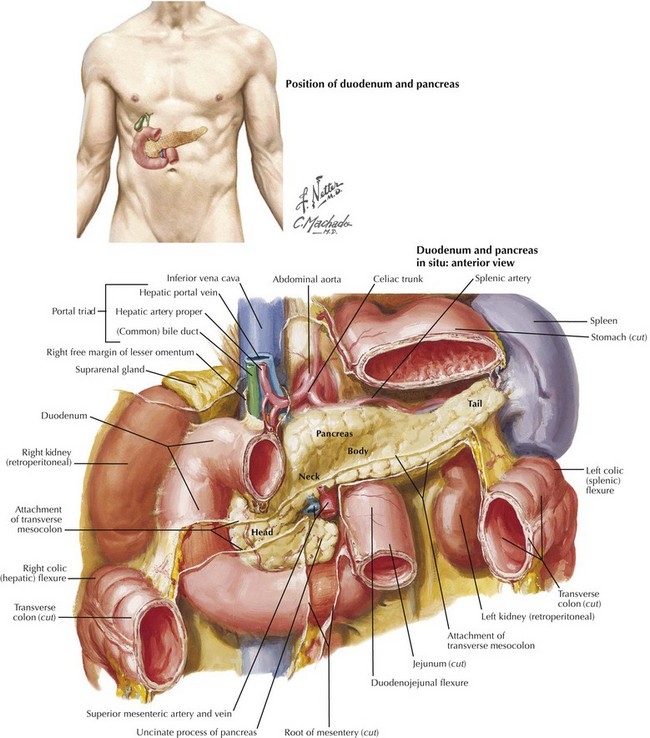
Bleeding duodenal ulcers are often located in the posterior pyloric bulb and penetrate into the gastroduodenal artery, which lies just posterior to the duodenum (see Fig. 9-2, A). Access to these ulcers is best achieved using a longitudinal incision across the pylorus, including several centimeters of both the stomach and the duodenum. This procedure is termed a pyloromyotomy (Fig. 9-2, B). Once the duodenum has been entered at this site, control of the bleeding posterior ulcer is achieved by placement of sutures in the four quadrants around the ulcer. It must be remembered that the common bile duct is just lateral and posterior to this site, so sutures should not be placed too deep (Fig. 9-3).
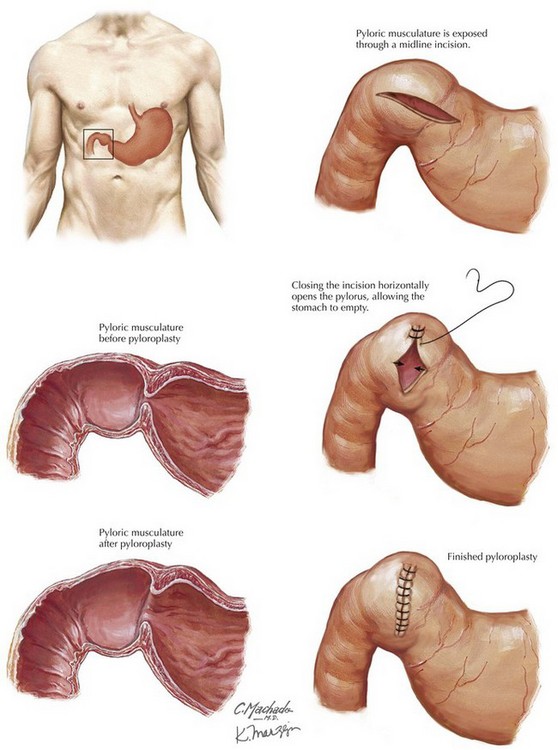
After suture control of a bleeding duodenal ulcer through a pyloromyotomy, the gastroduodenotomy or pyloromyotomy must be closed. To avoid narrowing of this site, as well as to provide adequate drainage if a truncal vagotomy is also performed, the longitudinal incision is closed in a transverse orientation. This repair is called a Heineke-Mikulicz pyloroplasty (Fig. 9-4).
Hunt, PS, McIntyre, RL. Choice of emergency operative procedure for bleeding duodenal ulcer. Br J Surg. 1990;77(9):1004–1006.
Jawaid, W, Abdalwahab, A, Blair, G, Skarsgard, E, Webber, E. Outcomes of pyloroplasty and pyloric dilatation in children diagnosed with nonobstructive delayed gastric emptying. J Pediatr Surg. 2006;41(12):2059–2061.
Millat, B, Hay, JM, Valleur, P, Fingerhut, A, Fagniez, PL. Emergency surgical treatment for bleeding duodenal ulcer: oversewing plus vagotomy versus gastric resection—a controlled randomized trial. French Associations for Surgical Research. World J Surg. 1993;17(5):568–573.
Sharma, KK, Ranka, P, Goyal, P, Dabi, DR. Gastric outlet obstruction in children: an overview with report of Jodhpur disease and Sharma’s classification. J Pediatr Surg. 2008;43(10):1891–1897.