Chapter 108 Heat Injury
The interest in heat-related illnesses has grown enormously, largely because of global warming and an increased frequency of heat waves.1,2 According to the Centers for Disease Control and Prevention, from 1999 to 2003, excessive heat exposure caused 3442 deaths in the United States.3 During this period, more people died of extreme heat than as a result of hurricanes, lightning, tornadoes, floods, and earthquakes. Among the pediatric population, neonates and infants are at highest risk, mainly because of poorly developed thermoregulatory mechanisms and total dependence on caregivers to provide adequate protection from excessive heat. Children with mental illness and chronic diseases are at high risk. Adolescents are also at increased risk mostly due to poor judgment or intoxication.
Over the past decade, the understanding of cellular and molecular responses to heat stress has improved dramatically. This is a multiorgan injury resulting from a complex interplay between the cytotoxic effect of the heat and the inflammatory and coagulation responses of the host.4 Despite progress in the understanding of the pathophysiology of heat injury, treatment remains supportive, with emphasis on immediate cooling. Prevention and education are still the best tools available in the hands of healthcare providers to minimize heat-related morbidity and death. This chapter covers the epidemiology, pathophysiology, clinical manifestations, and treatment of nonexertional heat-related illness in the pediatric population.
Definitions
Epidemiology
Excessive heat is the second largest contributor to death by natural events in the United States.8 In the period from 1999 to 2003, an annual average of 688 deaths in the United States was attributable to “excessive heat exposure.” Persons aged 15 years and younger accounted for 7% of deaths within the group of deaths caused by weather conditions.9 During heat waves, there is a significant increase in the heat-related death rate. For example, in 1980, a year with a record heat wave, the death rate was more than three times higher than that for any other year during the 19-year period of 1979 to 1997.10 Data on heat-related death are imprecise because this condition is underdiagnosed, its definition varies,4 and many cases of patients with near-fatal heat stroke who survive the acute hospitalization have a high 1-year death rate.11 In Saudi Arabia, where the temperature is extremely hot, the incidence of heat stroke varies seasonally, from 22 to 250 cases per 100,000 population.12 Heat-related illness is reported from subtropical and cold parts of the world as well. In Taiwan, a subtropical country without any history of heat waves, a cluster of heat shock cases was reported during periods of sustained hotter-than-average temperatures.13 In an observational study in which cold and hot areas in Europe were compared, it was shown that heat-related death started at higher temperatures in hot regions than in cold ones.14 High ambient temperature and humidity, lack of acclimatization, unavailability of air conditioning, and vigorous physical activity15 are major predisposing factors for heat-related illness. Within the pediatric population, children younger than 2 years are at higher risk, with specific factors like diarrheal disease, sweat gland dysfunction, child neglect, and underlying chronic or febrile illness contributing. Risk factors for adolescents include poor judgment that may lead to continuation of physical exertion despite warning symptoms. Alcohol and drug abuse and exposure to environmental toxins may put the adolescent at risk. Neuroleptic phenothiazines and tricyclic antidepressants, taken for medical indications; amphetamine and derivatives; marijuana and cocaine; or organophosphates, constituents of many pesticides, may all lead to heat-related illness.16 Their effect may be due to impaired heat loss or increased heat production.17 Lithium and fluoxetine (Prozac) may induce heat intolerance.18
Pathophysiology and Pathogenesis of Heat-Related Illnesses
Understanding the systemic and cellular pathophysiology of heat-related illnesses involves an appreciation of thermoregulation, physiologic alterations directly related to hyperthermia, acute phase response, and the production of heat shock proteins (HSPs). For normal enzymatic and cellular function, it is essential that body core temperature be maintained within a narrow range of about 37° C ± 0.5 to 0.9° C.16,19 The thermoregulation system, controlled by the hypothalamus, receives input from thermosensitive receptors in the skin and body core, compares the data with a reference level (the “set point”), and responds to an elevation of 0.3° C16,20 with activation of heat loss mechanisms.4,16,21
Heat dissipation occurs by means of four mechanisms: (1) conduction to the adjacent air and objects, (2) convection through air or liquid, (3) radiation of heat energy, and (4) evaporation. Once activated by the hypothalamus, the efferent heat response is both autonomic and behavioral. Blood delivery to the body surface is increased by sympathetic discharge causing cutaneous vasodilatation. Blood flow may increase eightfold to sixteenfold, up to 8 L/min.22 Thermal sweating, in response to parasympathetic discharge, can produce approximately 1 L/h/m2 of body surface of sweat. Evaporation of 1.7 mL of sweat will consume 1 kCal of heat energy; thus at maximal efficiency sweating can dissipate 588 kCal of energy per hour. Secondary to cutaneous vasodilatation and sweating, blood is shunted toward the periphery, and visceral perfusion is reduced, especially to the liver, kidneys, and intestines.23 Rising core temperature will also lead to tachycardia, a high cardiac output state, and an increase in minute ventilation. When ambient temperature equals or exceeds body temperature, conduction, convection, and radiation cease to be effective. Losses of salt and water through sweating may lead to dehydration and salt depletion, resulting in impaired thermoregulation.24 A combination of high ambient humidity and temperature creates a particularly dangerous situation. With ambient humidity of 90% to 95%, evaporation of sweat essentially stops, and if ambient temperature reaches body temperature, the body can no longer eliminate heat.
Acclimatization
Prolonged exposure to a hot environment results in adaptation and tolerance to higher temperature levels. Acclimatization to heat may take several weeks and involves multiple organs. Sweat glands develop increased capacity to secrete sweat, plasma volume is increased, and the renin-angiotensin-aldosterone axis is activated and leads to improved salt conservation. The adaptability of the cardiovascular system is probably the most important single determinant of one’s ability to tolerate heat stress.4,25 Even acclimatized people have definite limitations for heat tolerance. Once driven beyond a critical level, progression to a catastrophic condition may result.
Hyperthermia directly induces cellular injury. The severity of injury is cumulative, so exposure to a very high temperature for a brief period of time may cause similar injury to an exposure to a lower temperature for a longer period of time.26 Once extreme temperatures of 49° to 50° C have been reached, full destruction and cell necrosis occur. At lower temperatures cell death is mainly due to apoptosis.27
Acute Phase Response
Heat stress initiates cellular acute phase responses aimed at protecting against injury and promoting tissue repair. A variety of cytokines are produced in response to heat stress. Cytokines mediate a wide range of cellular, systemic, and both proinflammatory and antiinflammatory acute phase protein productions. For example, interleukin-6 (IL-6) has a pivotal role in modulating synthesis of inflammatory cytokines, both locally and systemically.4,28 IL-6 also stimulates production of antiinflammatory cytokines, which inhibit production of reactive oxygen species (ROS) and proteolytic enzyme release from activated leukocytes.28,29 Plasma levels of both proinflammatory (tumor necrosis factor alpha [TNF-α], IL-1, and interferon-γ) and antiinflammatory cytokines (IL-6, IL-10, TNF receptors p55 and p75) are elevated in patients with heat stroke.30–35 Soluble TNF, IL-2, and IL-6 receptors are also elevated in heat stroke.36,37 It has been shown that the severity of symptoms during heat stroke correlates well with IL-1 and IL-6 levels.30 Progression from heat stress to heat stroke depends on the time and extent of exposure to severe environmental conditions, but the acute phase response may continue after the patient is cooled. Onset of inflammation may be local with systemic progression,4,35 involving endothelial cell activation, release of endothelial vasoactive factors,38 endothelial cell injury, and microvascular thrombosis.38–41 The gastrointestinal tract may also play a role in the exaggeration of the inflammatory response. Vascular congestion, hemorrhage, thrombosis, and massive loss of surface epithelium in the jejunum was observed in a baboon model of heat stroke.42 These changes facilitate bacterial and endotoxin translocation which contributes significantly to inflammation and multiple organ dysfunction syndrome (MODS).23,43–46 Evidence for this phenomenon exists in animal models, but much less in humans.23,43,45–49 Alterations in the barrier function of the intestines may allow leakage of endotoxins that fuel the inflammatory response.
Part of the effect on endothelial cells involves activation of both the coagulation and the fibrinolytic systems.40 Heat stress by itself is a procoagulation condition since it causes platelet clumping in small vessels. In addition, heat stress may mediate endotoxemia, elevated levels of proinflammatory cytokines, and macrophage activation (via factor VIIa), all of which are well known inducers of coagulation. Injured endothelium, (e.g., heat stroke) plays an important role in producing and releasing both procoagulant and anticoagulant substances (e.g., von Willebrand factor antigen [vWF-Ag], tissue plasminogen activator, and plasminogen activator inhibitor).38,39 Circulating vWF-Ag, thrombomodulin, endothelin-1, nitric oxide (NO) metabolites, soluble E-selectin, and ICAM-1 (intercellular adhesion molecule 1) are elevated in heat-related illness, creating a clinical picture of disseminated intravascular coagulation (DIC).38,50–52 The cooling of patients with heat stroke reverses only part of these coagulation abnormalities.40 Another aspect of the cellular response to stress involves the heat shock response.
Nearly all cells will respond to heat stress with increased production of HSPs. Expression of HSP is controlled mainly at the gene transcription level. Increased intracellular HSP levels facilitate tolerance to heat stress with better cell survival.53,54 In animal models, it has been shown that preconditioning with heat or chemical stress conferred significant protection against heat stroke-induced hyperthermia, hypotension, and brain injury.55–57 These effects were mediated mainly by Hsp70 and Hsp72.56 Blocking the production of HSP results in increased cellular sensitivity to even mild degrees of heat stress.58 Conditions associated with low level of expression of HSP such as lack of acclimatization or certain genetic polymorphisms may make certain patients more vulnerable to heat stress or faster progression to heat stroke. There appears to be a preferential expression of different families of HSPs in different cell populations. There are also distinct post-injury time frames of induction for each family of HSP, emphasizing differences in cellular functional requirements for each family of HSP.59 It was suggested that Hsp72 may be used as a semiquantitative diagnostic probe of heat stress.60 In one human study, researchers found that levels of autoantibodies against Hsp71 in heat-induced diseases correlated well with the severity of illness.61 Thus the individual response to heat stress depends on the direct thermal injury (including thermal cytotoxicity, cardiovascular failure, and hypoxia in the face of increased metabolic requirement) and the acute-phase response of the host. Genetic factors likely play a significant role in determining response to heat stress. This complex interplay between leukocytes, endothelial and epithelial cells, and a variety of systemic changes may lead to the most extreme form of heat-related illness, heat stroke. A similar sequence of events has been shown to occur in sepsis.62 Recent studies, using a baboon model for heat stroke, provide more data on pathways of heat stroke-induced tissue injury and cell death. This model can be used to evaluate clinical changes and may be suitable to test immunomodulation therapies to improve outcome.42,63
Systemic Clinical Features
Involvement of multiple organs may be seen, to a certain degree, in heat syncope, heat cramps, and exhaustion. Heat stroke is a true systemic disorder. Per definition, core temperature must exceed 40° C, and the patient exhibits hypovolemic shock and central nervous system abnormalities such as delirium, convulsions, or coma. The heat stroke-mediated systemic dysfunction was shown to be similar to exertional heat stroke in reported cases with adult patients.11
Central Nervous System
Neurologic dysfunction is a cardinal feature of heat stroke. Brain dysfunction is usually severe but may be subtle, manifesting only as inappropriate behavior or impaired judgment; more often, however, patients have delirium or coma.21 Seizures may occur, especially during cooling. The central nervous system is particularly vulnerable to heat, the cerebellum being most susceptible.64 Pyramidal dysfunction, dysphagia, mental changes, quadriparesis, extrapyramidal syndrome, and neuropathy have all been described.21,65 No data regarding long-term neurologic outcome in children have been reported. In one adult series, 33% of the patients had moderate to severe impairment of neurologic function at discharge from the hospital.11
Pulmonary
The pulmonary system is not involved in early stages of heat-related illnesses. However, a high incidence (23% to 25%) of acute respiratory distress syndrome (ARDS) has been reported in adult patients with heat stroke.66,67 Patients with ARDS have a poor prognosis, with up to a 75% mortality rate.66 Lung involvement is part of the systemic response, as indicated by the fact that all patients who had ARDS also had coagulopathy and DIC.66
Cardiovascular
The cardiovascular system is usually compromised in heat-related illness. Hypotension and shock may result from dehydration, translocation of blood from central circulation to the periphery, or increased production of NO.21 Usually, circulation is hyperdynamic in these patients, with tachycardia and high cardiac output.68 Vasomotor tone may remain abnormally low, even after normal temperature and intravascular volume have been restored.25 Electrocardiographic changes are common in patients with heat stroke, including rhythm disturbances, conduction defects, prolonged QT interval, and ST segment changes. These may subside with cooling or may require correction of potassium, magnesium, or calcium abnormalities.69
Renal
Elevated blood urea nitrogen and creatinine levels are seen even in mild heat-related disease such as heat cramps.70 Moderate to severe renal insufficiency is common in classic heat stroke (up to 53% in one series11). Direct thermal injury, hypoperfusion (due to dehydration, cardiac failure, or both), rhabdomyolysis with myoglobinuria, release of vasoactive mediators, and DIC may all contribute to renal injury.4,21,71,72
Gastroenterologic
Involvement of the gastrointestinal system plays a significant role in the development of MODS in patients with heat stroke.4,73 The importance of the gastrointestinal system in other forms of heat-related illnesses is not well studied. Jejunal injury may lead to mild to moderate diarrhea. The liver may be severely injured in heat stroke. This is a metabolically active organ and a major site of heat production in the body. During periods of hyperthermia, liver temperature is among the highest of any organ in the body, putting it at high risk for injury.26 Abnormal liver function tests may be seen during heat-related illnesses. Elevation of aspartate aminotransferase (AST), alanine aminotransferase (ALT), γ-glutamyl transpeptidase (γ-GT), lactate dehydrogenase (LDH), and total bilirubin have been described.11,21,70 Patients with heat stroke demonstrate a typical rise in AST and ALT levels within 30 minutes from onset, that peaks at 48 to 72 hours following injury, with return to normal values after 10 to 14 days.26,74 Severe liver damage is more common in exertional heat stroke. Fulminant liver failure is rare and usually carries a grave prognosis even with liver transplantation.75
Metabolic
Early in the course of heat injury, the most common acid-base abnormality is a mixed non-anion gap metabolic acidosis and respiratory alkalosis. Hypokalemia resulting from the respiratory alkalosis, sweat losses, and renal wasting may change to hyperkalemia because of leak of cellular potassium. Several hours into the injury the clinical picture changes into a predominantly metabolic acidosis that is caused by sustained tissue injury.11,21,76
Hematologic
Thrombocytopenia, an elevated clotting time, and DIC are well documented in patients with heat stroke.4,11,21,41 The pathophysiology of DIC in patients with heat stroke has been previously discussed. The rapid decline of hematocrit in the first 24 hours following heat stroke is a common feature. This is partially explained by rehydration, but is most probably multifactorial. The red blood cell (RBC) half-life is shortened after heat stroke. In addition, RBCs are more fragile following exposure to high temperatures, leading to early removal from the circulation.26 Hypersegmented neutrophils may be observed in peripheral blood for the first few hours following the onset of heat stroke. The cause for theis phenomenon is unclear. These cells are thought to be undergoing changes associated with apoptosis.26
Infectious
In the early phase of heat stroke, blood culture findings are negative,77 but within 24 hours from admission, one study demonstrated that up to 27% of patients had positive blood cultures and 25% had positive urine cultures.11 The existing data come from adult series. The incidence of positive findings in blood or urine cultures in the pediatric population with heat stroke is unknown.
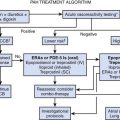
Treatment
The treatment of heat stroke starts at the scene with removing the patient from the circumstances that led to heat stroke in order to prevent any further increase in core temperature.
Rapid cooling and maintenance of organ system perfusion and function are the two major goals. Adherence to the basic resuscitative guidelines is required, with protection of the airway, management of breathing and monitoring for hypovolemia/shock, and appropriate fluid resuscitation. The most severely affected children have altered mental status, rising body temperature, and hypovolemic shock. After the airway is secured, the child with heat stroke should be moved to a cool environment; clothes should be removed; intravenous access should be obtained with one or two large-bore catheters; and a normal saline or lactated Ringer solution bolus of 20 mL/kg should be administered. Fluid resuscitation, besides ensuring organ perfusion, increases heat dissipation and lowers core temperature24 by improving skin blood flow. Cooling should be started as early as possible with whatever method is available, and the patient should be transported to the nearest hospital appropriate for children. Decreasing body temperature below 38.9° C within 30 minutes of presentation has been shown to improve survival.21
A variety of cooling methods have been used to promote heat loss, and controversy continues regarding the best cooling technique. Cold/ice-water immersion was twice as rapid in reducing the core temperature as the evaporative spray method in patients with exertional heat stroke.78 The mechanism for this rapid cooling relates to the high thermal gradient between skin and ice-water, leading to a faster heat loss by conductance as compared with evaporation.79 Ice water is readily available, does not require special equipment, and is suitable for both classic and exertional heat stroke. While some authors regard ice water immersion to be the most efficient cooling method,80 others claim there is no evidence to support the superiority of any cooling technique, especially in classic heat stroke.81,82 Critics of immersion point out that it may complicate resuscitation efforts of the comatose child who requires endotracheal intubation, mechanical ventilation, and close observation. Also, it is uncomfortable to the conscious child and may cause shivering and cutaneous vasoconstriction, which is counterproductive. Sponging the patient with ice water while massaging the body and using a fan may overcome some of these disadvantages, yet other studies have shown that keeping the skin relatively warm while allowing evaporation and convection to dissipate body heat is the most rapid way to decrease core body temperature.83,84 This can be done with special cooling units,83,85 but the concept of keeping the patient “wet and windy” can be easily achieved with the application of tepid water to the skin while a fan is used to keep high air flow and to maintain cool ambient temperature.86 Thus hospitals located in high-risk areas may consider buying special equipment, but most emergency departments and pediatric intensive care units (PICUs) may use this technique with readily available equipment.
Cooling blankets are widely used in the PICU setting. The effectiveness of this approach was evaluated only in patients with fever87 and no data are available concerning heatstroke patients. Invasive cooling techniques including iced peritoneal lavage as well as bladder and gastric lavage have been suggested and investigated to some extent. Peritoneal lavage is difficult to perform and requires placement of a peritoneal catheter and trained personnel. Evidence for gastric lavage comes mostly from canine models and was found to have no advantage over evaporative cooling.82 Recent reports of an intravascular cooling device to control body temperature found the system to be highly effective. However, as this was not evaluated on patients with heatstroke, it cannot be recommended at this point.88,89 Antipyretics cannot be recommended since their effect has not been systematically studied in this group of patients.82 In addition, these drugs lower body temperature by normalizing the elevated hypothalamic set point. In heat stroke, the elevated body temperature reflects failure of cooling mechanism rather than abnormal set point. Acetaminophen and salicylates should be avoided due to their potential to aggravate coagulopathy and hepatic injury.81,82 Dantrolene, which has been used successfully in the treatment of malignant hyperthermia and neuroleptic malignant syndrome, has been administered in the treatment of heat stress. Some studies have claimed that it may be effective in the treatment of heat stroke,90,91 whereas in others, including a double-blind randomized study,92 it was shown to be ineffective.
Once a core body temperature of 38.9° C has been achieved, active cooling may be be stopped. This end point appears to be safe in terms of mortality. Unfortunately a safe end point for long-term morbidity (particularly neurologic outcome) has not yet been established.81 All pediatric patients with heat stroke should be observed in the PICU, even if respiratory support is not required. Basic laboratory workup should include electrolytes (including sodium, potassium, magnesium, phosphate, and calcium), renal and liver function tests, complete blood count, and coagulation studies. Urine output should be followed closely, and a urine sample should be sent for myoglobin analysis. As previously mentioned, patients with heat stroke may continue to deteriorate even after body temperature is normalized because of the inflammatory response. There are no specific guidelines for treating patients with MODS that results from heat stroke.
Prevention is still the best treatment for heat-related illness. Whenever possible, people should acclimatize themselves to hot weather. Physical activity should be undertaken during cooler hours, and water intake should be increased. Children should never be left unattended in a closed car, especially during hot weather. Physicians’ awareness and knowledge may promote diagnosis of early forms of heat-related illness, thus preventing progression to heat stroke. On a national level, a good weather forecasting system and air-conditioned shelters for vulnerable populations may decrease heat-related morbidity and death during heat waves.93,94
References are available online at http://www.expertconsult.com.
1. Kalkstein L.S., Greene J.S. An evaluation of climate/mortality relationships in large U.S. cities and the possible impacts of a climate change. Environ Health Perspect. 1997;105:84-93.
2. O’Neill M.S., Ebi K.L. Temperature extremes and health: impact of climate variability and change in the United States. J Emerg Med. 2009;51(1):13-25.
3. Centers for Disease Control and Prevention. heat related death—United States, 1999-2003. MMWR. 2006;55(29):796-798.
4. Bouchama A., Knochel J.P. Heat stroke. N Engl J Med. 2002;346:1978-1988.
5. Eichner E.R. Treatment of suspected heat illness. Int J Sports Med. 1998;19:S150-S153.
6. Squire D.L. Heat illness. Fluid and electrolyte issues for pediatric and adolescent athletes. Pediatr Clin North Am. 1990;37:1085-1109.
7. Centers for Disease Control and Prevention (CDC). Heat-related deaths-United States, 1993. MMWR Morb Mortal Wkly Rep. 1993;42:558-560.
8 Thacker M.T., Lee R., Sabogal R.I., Henderson A. Overview of deaths associated with natural events, United States 1979-2004. Disasters. 2008;32(2):303-315.
9 Centers for Disease control and prevention (CDC). Heat related deaths- United States, 1999-2003. MMWR Morb Mortal Wkly Rep. 2006;55:796-798. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5529a2.htm
10. Centers for Disease Control and Prevention (CDC. Heat-related illnesses, deaths, and risk factors—Cincinnati and Dayton, Ohio, 1999, and United States, 1979-1997. MMWR Morb Mortal Wkly Rep. 2000;49:470-473.
11. Dematte J.E., O’Mara K., Buescher J., et al. Near-fatal heat stroke during the 1995 heat wave in Chicago. Ann Intern Med. 1998;129:173-181.
12. Ghaznawi H.I., Ibrahim M.A. Heat stroke and heat exhaustion in pilgrims performing the Haj (annual pilgrimage)in Saudi Arabia. Ann Saudi Med. 1987;7:323-326.
13. How C.K., Chern C.H., Wang L.M., et al. Heat stroke in a subtropical country. Am J Emerg Med. 2000;18:474-477.
14. Keatinge W.R., Donaldson G.C., Cordioli E., et al. Heat related mortality in warm and cold regions of Europe: observational study. BMJ. 2000;321:670-673.
15. Kilbourne E.M., Choi K., Jones T.S., et al. Risk factors for heatstroke: a case-control study. JAMA. 1982;247:3332-3336.
16. Lomax P., Schonbaum E. The effects of drugs on thermoregulation during exposure to hot environments. Prog Brain Res. 1998;115:193-204.
17. Clark W.G., Lipton J.M. Drug-related heatstroke. Pharmacol Ther. 1984;26:345-388.
18. Epstein Y., Albukrek D., Kalmovitc B., et al. Heat intolerance induced by antidepressants. Ann N Y Acad Sci. 1997;813:553-558.
19. Cox B., Green M.D., Lomax P. Behavioral thermoregulation in the study of drugs affecting body temperature. Pharmacol Biochem Behav. 1975;3:1051-1054.
20. Cox B., Ary M., Lomax P. Dopaminergic involvement in withdrawal hypothermia and thermoregulatory behavior in morphine dependent rats. Pharmacol Biochem Behav. 1976;4:259-262.
21. Grogan H., Hopkins P.M. Heat stroke: implications for critical care and anaesthesia. Br J Anaesth. 2002;88:700-707.
22. Rowell L.B. Cardiovascular aspects of human thermoregulation. Circ Res. 1983;52:367-379.
23. Hall D.M., Buettner G.R., Oberley L.W., et al. Mechanisms of circulatory and intestinal barrier dysfunction during whole body hyperthermia. Am J Physiol Heart Circ Physiol. 2001;280:H509-H521.
24. Deschamps A., Levy R.D., Cosio M.G., et al. Effect of saline infusion on body temperature and endurance during heavy exercise. J Appl Physiol. 1989;66:2799-2804.
25. Knochel J.P. Catastrophic medical events with exhaustive exercise: “white collar rhabdomyolysis,. Kidney Int. 1990;8:709-719.
26. Jardine D.S. Heat illness and Heat stroke. Pediatr Rev. 2007;28(7):249-258.
27. Sakaguchi Y., Stephens L.C., Makino M., et al. Apoptosis in tumors and normal tissues induced by whole body hyperthermia in rats. Cancer Res. 1995;55:5459-5464.
28. Gabay C., Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340:448-454.
29. Xing Z., Gauldie J., Cox G., et al. IL-6 is an antiinflammatory cytokine required for controlling local or systemic acute inflammatory responses. J Clin Invest. 1998;101:311-320.
30. Bouchama A., Al Sedairy S., Siddiqui S., et al. Elevated pyrogenic cytokines in heatstroke. Chest. 1993;104:1498-1502.
31. Bouchama A., Parhar R.S., el-Yazigi A., et al. Endotoxemia and release of tumor necrosis factor and interleukin 1 alpha in acute heatstroke. J Appl Physiol. 1991;70:2640-2644.
32. Camus G., Nys M., Poortmans J.R., et al. Endotoxaemia, production of tumour necrosis factor alpha and polymorphonuclear neutrophil activation following strenuous exercise in humans. Eur J Appl Physiol. 1998;79:62-68.
33. Chang D.M. The role of cytokines in heat stroke. Immunol Invest. 1993;22:553-561.
34. Lu K.C., Wang J.Y., Lin S.H., et al. Role of circulating cytokines and chemokines in exertional heatstroke. Crit Care Med. 2004;32:399-403.
35. Moldoveanu A.I., Shephard R.J., Shek P.N. Exercise elevates plasma levels but not gene expression of IL-1beta, IL-6, and TNF-alpha in blood mononuclear cells. J Appl Physiol. 2000;89:1499-1504.
36. Hammami M.M., Bouchama A., Al-Sedairy S., et al. Concentrations of soluble tumor necrosis factor and interleukin-6 receptors in heatstroke and heatstress. Crit Care Med. 1997;25:1314-1319.
37. Hammami M.M., Bouchama A., Shail E., et al. Elevated serum level of soluble interleukin-2 receptor in heatstroke. Intensive Care Med. 1998;24:988.
38. Bouchama A., Hammami M.M., Haq A., et al. Evidence for endothelial cell activation/injury in heatstroke. Crit Care Med. 1996;24:1173-1178.
39. Ang C., Dawes J. The effects of hyperthermia on human endothelial monolayers: modulation of thrombotic potential and permeability. Blood Coagul Fibrinolysis. 1994;5:193-199.
40. Bouchama A., Bridey F., Hammami M.M., et al. Activation of coagulation and fibrinolysis in heatstroke. Thromb Haemost. 1996;76:909-915.
41. al-Mashhadani S.A., Gader A.G., al Harthi S.S., et al. The coagulopathy of heat stroke: alterations in coagulation and fibrinolysis in heat stroke patients during the pilgrimage (Haj) to Makkah. Blood Coagul Fibrinolysis. 1994;5:731-736.
42 Roberts G.T., Ghebeh H., Chishti M.A., et al. Microvascular injury, thrombosis, inflammation, and apoptosis in the pathogenesis of heatstroke: a study in baboon model. Arterioscler Thromb Vasc Biol. 2008;28(6):1130-1136.
43. Bosenberg A.T., Brock-Utne J.G., Gaffin S.L., et al. Strenuous exercise causes systemic endotoxemia. J Appl Physiol. 1988;65:106-108.
44. Eshel G.M., Safar P., Stezoski W. The role of the gut in the pathogenesis of death due to hyperthermia. Am J Forensic Med Pathol. 2001;22:100-104.
45. Sakurada S., Hales J.R. A role for gastrointestinal endotoxins in enhancement of heat tolerance by physical fitness. J Appl Physiol. 1998;84:207-214.
46. Shapiro Y., Alkan M., Epstein Y., et al. Increase in rat intestinal permeability to endotoxin during hyperthermia. Eur J Appl Physiol Occup Physiol. 1986;55:410-412.
47. Gathiram P., Wells M.T., Brock-Utne J.G., et al. Antilipopolysaccharide improves survival in primates subjected to heat stroke. Circ Shock. 1987;23:157-164.
48. Gathiram P., Wells M.T., Raidoo D., et al. Portal and systemic plasma lipopolysaccharide concentrations in heat-stressed primates. Circ Shock. 1988;25:223-230.
49. Graber C.D., Reinhold R.B., Breman J.G., et al. Fatal heat stroke. Circulating endotoxin and gram-negative sepsis as complications. JAMA. 1971;216:1195-1196.
50. Alzeer A.H., Al-Arifi A., Warsy A.S., et al. Nitric oxide production is enhanced in patients with heat stroke. Intensive Care Med. 1999;25:58-62.
51. Hammami M.M., Bouchama A. Al Sedairy S: Levels of soluble l-selectin and E-selectin in heatstroke and heatstress. Chest. 1998;114:949-950.
52. Shieh S.D., Shiang J.C., Lin Y.F., et al. Circulating angiotensin-converting enzyme, von Willebrand factor antigen and thrombomodulin in exertional heat stroke. Clin Sci (Lond). 1995;89:261-265.
53. Moseley P.L. Heat shock proteins and heat adaptation of the whole organism. J Appl Physiol. 1997;83:1413-1417.
54. Polla B.S., Bachelet M., Elia G., et al. Stress proteins in inflammation. Ann N Y Acad Sci. 1998;851:75-85.
55. Chen J., Graham S.H., Zhu R.L., et al. Stress proteins and tolerance to focal cerebral ischemia. J Cereb Blood Flow Metab. 1996;16:566-577.
56. Yang Y.L., Lin M.T. Heat shock protein expression protects against cerebral ischemia and monoamine overload in rat heatstroke. Am J Physiol Heart Circ Physiol. 1999;276:H1961-H1967.
57. Yellon D.M., Marber M.S. Hsp70 in myocardial ischaemia. Experientia. 1994;50:1075-1084.
58. Riabowol K.T., Mizzen L.A., Welch W.J. Heat shock is lethal to fibroblasts microinjected with antibodies against hsp70. Science. 1988;242:433-436.
59. Reynolds L.P., Allen G.V. A review of heat shock protein induction following cerebellar injury. Cerebellum. 2003;2:171-177.
60. Bratton S.L., Jardine D.S., Mirkes P.E. Constitutive synthesis of heat shock protein (72 kD) in human peripheral blood mononuclear cells: implications for use as a clinical test of recent thermal stress. Int J Hyperthermia. 1997;13:157-168.
61. Wu T., Chen S., Xiao C. Presence of antibody against the inducible Hsp71 in patients with acute heat-induced illness. Cell Stress Chaperones. 2001;6:113-120.
62. Despond O., Proulx F., Carcillo J.A., et al. Pediatric sepsis and multiple organ dysfunction syndrome. Curr Opin Pediatr. 2001;13:247-253.
63. Bouchama A., Roberts G., Al Mohanna F., et al. Inflammatory, hemostatic, and clinical changes in a baboon experimental model for heatstroke. J Appl Physiol. 2005;98(2):697-705.
64. Albukrek D., Bakon M., Moran D.S., et al. Heat-stroke-induced cerebellar atrophy: clinical course, CT and MRI findings. Neuroradiology. 1997;39:195-197.
65. Kalita J., Misra U.K. Neurophysiological studies in a patient with heat stroke. J Neurol. 2001;248:993-995.
66. El-Kassimi F.A., Al-Mashhadani S., Abdullah A.K., et al. Adult respiratory distress syndrome and disseminated intravascular coagulation complicating heat stroke. Chest. 1986;90:571-574.
67. Soliman S.M., Abu-Taleb Z., Khogali M., et al. Pulmonary aspiration and adult respiratory distress syndrome in 40 cases of heat stroke. In: Khogali M.K., Hales J.R.S., editors. Heat stroke and temperature regulation. Sydney: Academic Press, 1983.
68. Shahid M.S., Hatle L., Mansour H., et al. Echocardiographic and doppler study of patients with heat stroke and heat exhaustion. Int J Cardiac Imaging. 1999;15:279-285.
69. Akhtar M.J., Al-Nozha M., AL-harti S., et al. Electrocardiographic abnormalities in patients with heat stroke. Chest. 1993;104:411-414.
70. Donoghue A.M., Sinclair M.J., Bates G.P. Heat exhaustion in a deep underground metalliferous mine. Occup Environ Med. 2000;57:165-174.
71. Lin Y.F., Wang J.Y., Chou T.C., et al. Vasoactive mediators and renal haemodynamics in exertional heat stroke complicated by acute renal failure. QJM. 2003;96:193-201.
72. Semenza J.C. Acute renal failure during heat waves. Am J Prev Med. 1999;17:97.
73. Yoshitake S., Noguchi T., Hoasi S., et al. Changes in intramucosal pH and gut blood flow during whole body heating in porcine model. Int J Hyperthermia. 1998;14:285-291.
74. Garcin J.M., Bronstein J.A., Cremades S., et al. Acute liver failure is frequent during heat stroke. W J Gastroentorol. 2008;14:158-159.
75. Berger J., Hart J., Millis M., et al. Fulminant hepatic failure from heat stroke requiring liver transplantation. J Clin Gastroenterol. 2000;30:429-431.
76. Bouchama A., De Vol E.B. Acid-base alterations in heatstroke. Intensive Care Med. 2001;27:680-685.
77. Bouchama A. Features and outcomes of classic heat stroke. Ann Intern Med. 1999;130:613.
78. Armstrong L.E., Crago A.E., Adams R., et al. Whole-body cooling of hyperthermic runners: comparison of two field therapies. Am J Emerg Med. 1996;14:355-358.
79. Gaffin S.L., Gardner J.W., Flinn S.D. Cooling methods for heatstroke victims. Ann Intern Med. 2000;132:678.
80. MecDermott B.P., Casa D.J., Ganio M.S., et al. Acute whole body cooling for exercise-induced hyperthermia: a systematic review. J Athl Train. 2009;44(1):84-93.
81. Bouchama A., Dehbi M., Chaves-Carballo E. Cooling and hemodynamic management in heatstroke: practical recommendations. Crit Care. 2007;11(3):R54.
82. Hadad E., Rav-Acha M., Heled Y., et al. Heat stroke: a review of cooling methods, Sports Med. 2004;34(8):501-511.
83. Weiner J.S., Khogali M. A physiological body-cooling unit for treatment of heat stroke. Lancet. 1980;1:507-509.
84. Wyndham C.H., Strydom N.B., Cooke H.M., et al. Methods of cooling subjects with hyperpyrexia. J Appl Physiol. 1959;14:771-776.
85. Al-Aska A.K., Abu-Aisha H., Yaqub B., et al. Simplified cooling bed for heatstroke. Lancet. 1987;1:381.
86. Slovis C.M. Features and outcomes of classic heat stroke. Ann Intern Med. 1999;130:614-615.
87. Henker R., Rogers S., Kramer D.J., et al. Comparison of fever treatments in the criticallly ill: a pilot study. Am J Crit Care. 2001;10(4):276-280.
88. Schmutzhard E., Engelhardt K., Beer R., et al. Safety and efficacy of a novel intravascular cooling device to control body temperature in neurologic intensive care patients: a prospective pilot study. Crit Care Med. 2002;30(11):2481-2488.
89. Bernard S., Buist M. Induced hypothermia in critical care medicine: a review. Crit Care Med. 2003;32:1928-1948.
90. Channa A.B., Seraj M.A., Sadique A.A., et al. Is dantrolene effective in heat stroke patients? Crit Care Med. 1990;18:290-292.
91. Moran D., Epstein Y., Wiener M., et al. Dantrolene and recovery from heat stroke. Aviat Space Environ Med. 1999;70:987-989.
92. Bouchama A., Cafege A., Devol E.B., et al. Ineffectiveness of dantrolene sodium in the treatment of heatstroke. Crit Care Med. 1991;19:176-180.
93. Changnon S.A., Easterling D.R. Disaster management: U.S. policies pertaining to weather and climate extremes. Science. 2000;289:2053-2055.
94. Kalkstein L.S. Saving lives during extreme weather in summer. BMJ. 2000;321:650-651.