Chapter 11 Heart Sounds and Extra Sounds
B. Cardiac Auscultation: Some Suggestions
1 Why is cardiac auscultation so difficult?
 Cardiac sounds are often at the threshold of audibility. The human ear can only perceive sounds between 20 and 20,000 Hz: it can neither reach beyond (as dolphins and whales do) nor go below it (as elephants often do). Yet, in this range, it has a preferential bandwidth of 1000–5000 Hz, corresponding to that of the human voice. Yet, most cardiac sounds are <500 Hz. In fact, many are so low pitched to be almost inaudible (S3 or S4 can be <100 Hz).
Cardiac sounds are often at the threshold of audibility. The human ear can only perceive sounds between 20 and 20,000 Hz: it can neither reach beyond (as dolphins and whales do) nor go below it (as elephants often do). Yet, in this range, it has a preferential bandwidth of 1000–5000 Hz, corresponding to that of the human voice. Yet, most cardiac sounds are <500 Hz. In fact, many are so low pitched to be almost inaudible (S3 or S4 can be <100 Hz).
 Cardiac sounds are crammed in a very little time interval. At a rate of 70/minute, a cycle of 0.8 seconds can easily harbor four to five sounds, many barely detectable.
Cardiac sounds are crammed in a very little time interval. At a rate of 70/minute, a cycle of 0.8 seconds can easily harbor four to five sounds, many barely detectable.
 Patients’ hair and respiration create misleading artifacts.
Patients’ hair and respiration create misleading artifacts.
 The obesity epidemic has given many patients a much fattier chest muffler.
The obesity epidemic has given many patients a much fattier chest muffler.
 Pathology has shifted from rheumatic to coronary, thus reducing the pool of teaching patients.
Pathology has shifted from rheumatic to coronary, thus reducing the pool of teaching patients.
 Our ever-increasing fascination with the inanimate and the machine (and the sophistication of technology), compounded by:
Our ever-increasing fascination with the inanimate and the machine (and the sophistication of technology), compounded by:
2 How can you make auscultation a little easier?
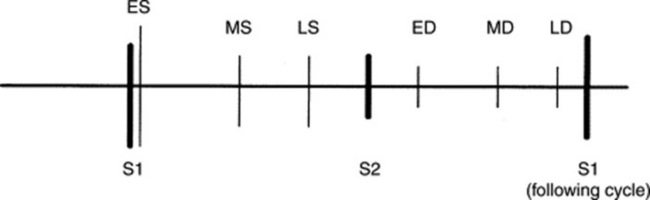
 Separate systole from diastole (easily done in normal rates by recognizing the acoustic differences of S1 and S2 plus the long and short intervals; in faster hearts, it may require simultaneous assessment of the arterial pulse or precordial impulse).
Separate systole from diastole (easily done in normal rates by recognizing the acoustic differences of S1 and S2 plus the long and short intervals; in faster hearts, it may require simultaneous assessment of the arterial pulse or precordial impulse).
 “Inch” (move your stethoscope inch by inch, from auscultatory area to auscultatory area).
“Inch” (move your stethoscope inch by inch, from auscultatory area to auscultatory area).
 Know how to use your tool: (1) bell versus diaphragm; (2) patient’s position (supine, seated, and left lateral decubitus); (3) changes with respiration; and (4) dynamic bedside maneuvers (straight-leg raising, squatting-standing, Valsalva, hand-gripping, exercise).
Know how to use your tool: (1) bell versus diaphragm; (2) patient’s position (supine, seated, and left lateral decubitus); (3) changes with respiration; and (4) dynamic bedside maneuvers (straight-leg raising, squatting-standing, Valsalva, hand-gripping, exercise).
 When challenged by feeble and crammed signals, focus on one sound at a time.
When challenged by feeble and crammed signals, focus on one sound at a time.
 Develop pattern recognition. This means practice, practice, practice…. In fact, you may need to hear an individual acoustic event as many as 500 times before you can master it.
Develop pattern recognition. This means practice, practice, practice…. In fact, you may need to hear an individual acoustic event as many as 500 times before you can master it.
C. Normal Heart Sounds
5 What are the cardiac areas?
They are areas of chest wall projection that correspond to the four cardiac valves (see Chapter 12, questions 1 and 2). In a clockwise fashion:
 Aortic area: Second right parasternal interspace
Aortic area: Second right parasternal interspace
 Pulmonic area: Second left parasternal interspace
Pulmonic area: Second left parasternal interspace
 Erb’s point: Third left parasternal interspace (area of left ventricular outflow)
Erb’s point: Third left parasternal interspace (area of left ventricular outflow)
 Mitral area: Apex (fifth interspace left midclavicular line)
Mitral area: Apex (fifth interspace left midclavicular line)
 Tricuspid area: Fourth to fifth left parasternal space, at times extending into the epigastrium/subxiphoid
Tricuspid area: Fourth to fifth left parasternal space, at times extending into the epigastrium/subxiphoid
(1) First Heart Sound (S1)
6 Where is S1 best heard?
At the apex (for its mitral component) and over the subxiphoid/epigastrium (for the tricuspid).
7 How is S1 generated?
By the vibration of valves, ventricles, and blood that coincides with:
1. Closure of the atrioventricular (A-V) valves
2. Opening of the semilunar valves. This in turn leads to two separate sounds, caused by:
In the absence of pathology, only A-V closure is responsible for S1. Semilunar opening is silent.
8 Which characteristics of S1 are clinically valuable and should therefore be identified?
The most valuable is intensity (and variations thereof). The next most valuable is splitting.
11 Which factors are responsible for the loudness of S1?
In addition to shape and thickness of the chest wall, three major factors play a role:
1. The rate of rise in left ventricular pressure: This is a function of ventricular contractility, with stronger contractions causing a faster rise in left ventricular pressure and thus brisker and more forceful A-V closure. Hence, a loud S1 is typical of the hyperkinetic heart syndrome, whereas a soft (muffled) S1 is instead common in congestive heart failure, whose failing ventricles can only generate a slow rise in systolic pressure.
2. The separation between atrioventricular leaflets at the onset of ventricular systole: The closer the leaflets, the softer S1 is; conversely, the wider apart the leaflets, the louder S1 is. This mechanism feeds into two other important variables:
 The duration of the P-R interval: A short P-R forces the ventricles to contract while the leaflets are still widely separated, so that their closure occurs on a steeper part of the left ventricular pressure curve. This, in turn, means a more forceful and louder closure. Conversely, a long P-R provides enough time for the leaflets to come close to each other, thus softening S1. A muffled S1 used to be quite common in rheumatic fever with first- degree A-V block. The progressive P-R lengthening of the Wenckebach phenomenon may also gradually (and increasingly) soften S1.
The duration of the P-R interval: A short P-R forces the ventricles to contract while the leaflets are still widely separated, so that their closure occurs on a steeper part of the left ventricular pressure curve. This, in turn, means a more forceful and louder closure. Conversely, a long P-R provides enough time for the leaflets to come close to each other, thus softening S1. A muffled S1 used to be quite common in rheumatic fever with first- degree A-V block. The progressive P-R lengthening of the Wenckebach phenomenon may also gradually (and increasingly) soften S1. The atrioventricular pressure gradient: A large A-V pressure gradient keeps the leaflets widely separated until ventricular pressure rises high enough to shut them close. Since the closure takes place on a steeper part of the left ventricular pressure curve, it will be forceful and loud. Hence, the longer the ventricle has to contract in order to close the A-V valve, the louder S1 will be. This is quite common in mitral stenosis, where it contributes to the loudness of S1.
The atrioventricular pressure gradient: A large A-V pressure gradient keeps the leaflets widely separated until ventricular pressure rises high enough to shut them close. Since the closure takes place on a steeper part of the left ventricular pressure curve, it will be forceful and loud. Hence, the longer the ventricle has to contract in order to close the A-V valve, the louder S1 will be. This is quite common in mitral stenosis, where it contributes to the loudness of S1.3. The thickness of the atrioventricular leaflet: The thicker the leaflets, the louder S1 is (banging hardbacks against each other generates more noise than banging paperbacks). Still, a soft S1 may indicate leaflets that are too rigid. Hence, a thickened and stenotic mitral valve may generate a booming S1 early on in the disease, but a softer (or absent) S1 when the leaflets get eventually calcified and fixed.
13 Which diseases present with a variable intensity of S1?
Heart blocks, such as second degree (i.e., Mobitz I or Wenckebach) and third degree:
 In second-degree A-V block, there is progressive softening of S1, while S2 remains constant. This is due to the increasing P-R lengthening, until a beat is eventually dropped. It is so typical of Mobitz I that Wenckebach could describe it even before electrocardiogram (ECG) availability.
In second-degree A-V block, there is progressive softening of S1, while S2 remains constant. This is due to the increasing P-R lengthening, until a beat is eventually dropped. It is so typical of Mobitz I that Wenckebach could describe it even before electrocardiogram (ECG) availability.
 In third-degree A-V block (typical of Morgagni-Adams-Stokes syndrome), the change in S1 intensity is instead random and chaotic because the atrium and ventricle march to the beat of a different drummer, with rates that are totally independent—when ventricular contraction catches the A-V valves wide apart, S1 booms; when it catches them partially closed, S1 softens. The varying S1 intensity is so typically random to allow the recognition of complete block just on the basis of auscultation (Table 11-1).
In third-degree A-V block (typical of Morgagni-Adams-Stokes syndrome), the change in S1 intensity is instead random and chaotic because the atrium and ventricle march to the beat of a different drummer, with rates that are totally independent—when ventricular contraction catches the A-V valves wide apart, S1 booms; when it catches them partially closed, S1 softens. The varying S1 intensity is so typically random to allow the recognition of complete block just on the basis of auscultation (Table 11-1).
| Loud | Variable | Soft |
|---|---|---|
| Short P-R interval (<160 msec) | Atrial fibrillation | Long P-R interval (>200 msec) |
| Increased contractility (hyperkinetic states) | Atrioventricular block (Wenckebach and third degree) | Decreased contractility (left ventricular dysfunction) |
| Thickening of mitral (or tricuspid) leaflets | Ventricular tachycardia (due to atrioventricular dissociation) | Left bundle branch block |
| Increased atrioventricular pressure gradient (stenosis of the A-V valves) | Pulsus alternans | Calcification of A-V valve(s) |
| Premature closure of mitral valve (acute aortic regurgitation) | ||
| Mitral (or tricuspid) regurgitation |
18 How is S1 in mitral stenosis (MS)?
 Thickening of the mitral leaflets: In the late stages of MS, however, leaflets can become stiff and poorly mobile, which, in turn, softens S1 and eventually eliminates it.
Thickening of the mitral leaflets: In the late stages of MS, however, leaflets can become stiff and poorly mobile, which, in turn, softens S1 and eventually eliminates it.
 High atrioventricular pressure gradient: This is produced by the stenotic valve and keeps the A-V leaflets maximally separated at the onset of ventricular contraction.
High atrioventricular pressure gradient: This is produced by the stenotic valve and keeps the A-V leaflets maximally separated at the onset of ventricular contraction.
19 What other conditions can be associated with a loud S1?
 Holosystolic mitral valve prolapse with regurgitation (where the prolapse delays the tension of the redundant mitral leaflet, thus allowing it to occur at peak of ventricular contraction, which makes it louder). A similar mechanism takes place in:
Holosystolic mitral valve prolapse with regurgitation (where the prolapse delays the tension of the redundant mitral leaflet, thus allowing it to occur at peak of ventricular contraction, which makes it louder). A similar mechanism takes place in:
 A left-atrial myxoma. Here it is the tumor that delays the closure of the mitral valve, thus allowing it to occur at peak of ventricular contraction and making it, therefore, louder. As a result, 80% of patients with this condition will have a loud S1.
A left-atrial myxoma. Here it is the tumor that delays the closure of the mitral valve, thus allowing it to occur at peak of ventricular contraction and making it, therefore, louder. As a result, 80% of patients with this condition will have a loud S1.
 Short P-R interval, as in the pre-excitation syndromes of Wolff-Parkinson-White and Ganong-Levine syndromes.
Short P-R interval, as in the pre-excitation syndromes of Wolff-Parkinson-White and Ganong-Levine syndromes.
(2) Second Heart Sound (S2)
31 How is S2 generated?
By sudden deceleration of blood following the closure of aortic (A2) and pulmonic (P2) valves.
32 Which of the two semilunar valve closes earlier?
The aortic, due to systemic pressure being normally higher than pulmonic pressure.
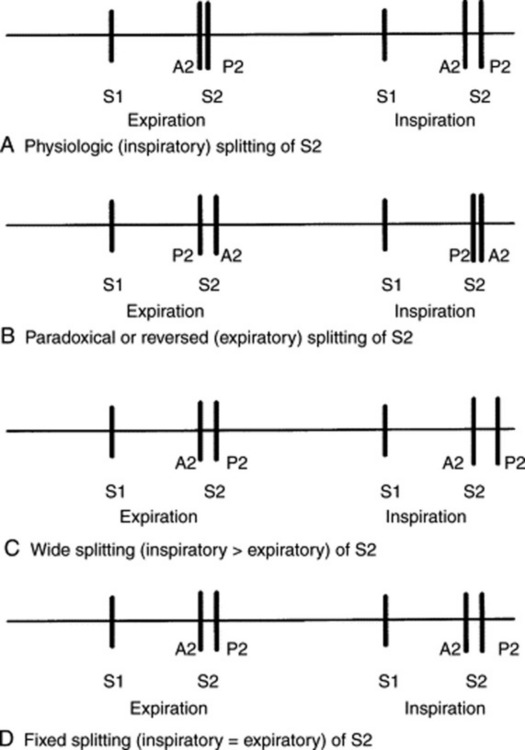
35 What is a physiologic splitting of S2?
It is the inspiratory widening of the normal interval between A2 and P2. This is triggered by:
37 How common is a physiologic splitting of S2?
Not very common. In a study of 196 normal adults examined in the supine position, only 52.1% had an audible inspiratory split of S2. Physiologic splitting was much more common in younger individuals (60% of those between ages 21 to 30, and 34% of those older than 50). Indeed, after age 50, S2 appeared single in more than 60% of subjects, as opposed to 36% for all ages. Hence, in older patients a single S2 should not be considered evidence for a delayed A2 (and therefore it should not suggest underlying aortic stenosis [AS] or a left bundle branch block) (see Fig. 11-1).
38 Why does S2 splitting disappear with aging?
Because of senile emphysema, with greater air muffling of the pulmonic component of S2.
39 How important is a patient’s position on S2 splitting?
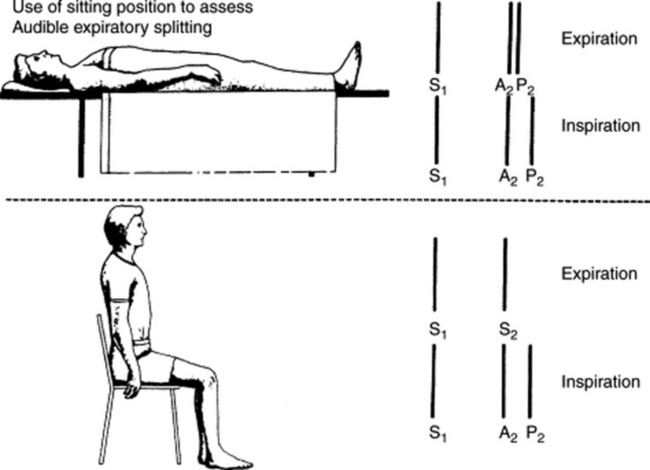
Very important. A supine position increases venous return, lengthens right ventricular systole, and thus widens the physiologic splitting of S2. Conversely, a sitting (or standing) position decreases venous return, shortens right ventricular systole, and narrows the physiologic split (Fig. 11-2). This is especially important when analyzing an expiratory splitting of S2. In a study by Adolph and Fowler, 22/200 (11%) normal subjects had an expiratory split while supine, but only 1/22 maintained it upon sitting or standing. Hence, a true expiratory splitting of S2 is one that is present both in a recumbent and upright position.
40 What is the significance of a true expiratory splitting of S2?
44 What is a fixed splitting of S2? What does it mean?
It is an S2 that remains audibly split throughout respiration, both in the supine and upright positions, and with a consistent interval between its two components. Although encountered in severe ventricular failure, a fixed splitting of S2 should suggest a septal defect (most often atrial but occasionally ventricular), especially if associated with pulmonary hypertension. The defect (and its shunt) eliminate the respiratory changes in right and left ventricular stroke volume, thus fixing the S2 splitting (more rarely, a fixed S2 split will occur in severe impedance to right ventricular emptying, such as that of pulmonary stenosis, pulmonary hypertension, or massive pulmonary embolism—with or without bundle branch block). These patients cannot cope with the increased venous return of inspiration by increasing right ventricular stroke volume. Hence, they maintain their S2 widely and persistently split throughout respiration (see Fig. 11-3).
45 What is the differential diagnosis of a fixed splitting of S2?
A late-systolic click (which precedes S2) and an early diastolic extra sound (which follows S2):
 The late-systolic click varies with bedside maneuvers and is loudest at the apex (conversely, the split S2 is unchanged with maneuvers and only heard at the base).
The late-systolic click varies with bedside maneuvers and is loudest at the apex (conversely, the split S2 is unchanged with maneuvers and only heard at the base).
 The two most common early diastolic extra sounds are the S3 and the opening snap (OS) of mitral (or tricuspid) stenosis (for a discussion of how to differentiate an opening snap from a widely split S2 or an S3, see questions 103, 104, and 130). OS is primarily apical, whereas the split S2 is basilar. Still, OS can be loud enough to transmit to the base, thus producing a triple lilt in inspiration (OS + split S2, with a loud P2 because of pulmonary hypertension). Note that the interval between S2 and OS is wider than that between the two components of S2. Finally, an OS is usually (but not necessarily) associated with a diastolic rumble.
The two most common early diastolic extra sounds are the S3 and the opening snap (OS) of mitral (or tricuspid) stenosis (for a discussion of how to differentiate an opening snap from a widely split S2 or an S3, see questions 103, 104, and 130). OS is primarily apical, whereas the split S2 is basilar. Still, OS can be loud enough to transmit to the base, thus producing a triple lilt in inspiration (OS + split S2, with a loud P2 because of pulmonary hypertension). Note that the interval between S2 and OS is wider than that between the two components of S2. Finally, an OS is usually (but not necessarily) associated with a diastolic rumble.
48 What are the causes of paradoxical S2 splitting?
 Delayed aortic closure. This is indeed the most common reason, usually due to a complete left bundle branch block (where reversed S2 splitting can occur in 84% of the cases). Other causes include increased impedance to left ventricular emptying (hypertension, AS, coarctation) or left ventricular dysfunction. The latter can occur in acute ischemia and various cardiomyopathies.
Delayed aortic closure. This is indeed the most common reason, usually due to a complete left bundle branch block (where reversed S2 splitting can occur in 84% of the cases). Other causes include increased impedance to left ventricular emptying (hypertension, AS, coarctation) or left ventricular dysfunction. The latter can occur in acute ischemia and various cardiomyopathies.
 Early pulmonic closure. This is a much less common cause of paradoxical splitting, usually due to decreased right ventricular filling—from either tricuspid regurgitation or right atrial myxoma.
Early pulmonic closure. This is a much less common cause of paradoxical splitting, usually due to decreased right ventricular filling—from either tricuspid regurgitation or right atrial myxoma.
50 What is the significance of a “single splitting” of S2?
 Aging: The audible splitting of S2 decreases in prevalence with age, to the point of becoming absent in most subjects older than 60. This is probably due to the muffling of P2 by the “physiologic” senile emphysema.
Aging: The audible splitting of S2 decreases in prevalence with age, to the point of becoming absent in most subjects older than 60. This is probably due to the muffling of P2 by the “physiologic” senile emphysema.
 Emphysema: The hyperinflated lungs will muffle P2 during inspiration, thus making A2 the only audible sound. Because this phenomenon is less pronounced in exhalation, these patients may be misdiagnosed as having paradoxical splitting of S2 (while, in fact, they have a pseudo-paradoxical splitting that becomes evident only in expiration).
Emphysema: The hyperinflated lungs will muffle P2 during inspiration, thus making A2 the only audible sound. Because this phenomenon is less pronounced in exhalation, these patients may be misdiagnosed as having paradoxical splitting of S2 (while, in fact, they have a pseudo-paradoxical splitting that becomes evident only in expiration).
 Reversed (or paradoxical) splitting: In this case, the split will indeed occur only in exhalation.
Reversed (or paradoxical) splitting: In this case, the split will indeed occur only in exhalation.
 Pulmonary hypertension: Increased impedance on right ventricular emptying makes the ventricle unable to cope with the increased venous return of inspiration. Hence, there will be no inspiratory lengthening of right ventricular systole and no inspiratory splitting of S2.
Pulmonary hypertension: Increased impedance on right ventricular emptying makes the ventricle unable to cope with the increased venous return of inspiration. Hence, there will be no inspiratory lengthening of right ventricular systole and no inspiratory splitting of S2.
 Semilunar valvular disease: Stiffening and reduced mobility of semilunar valves may also lead to the disappearance of either A2 or P2, thus making S2 “single.”
Semilunar valvular disease: Stiffening and reduced mobility of semilunar valves may also lead to the disappearance of either A2 or P2, thus making S2 “single.”
D. Extra Sounds
60 What are extra heart sounds?
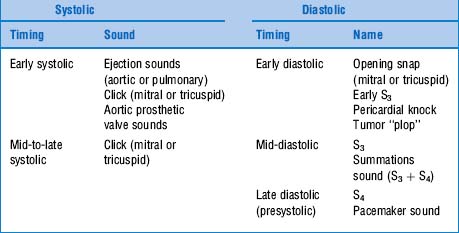
They are pathologic sounds that may occur in addition to the normal sounds (S1 and S2). Based on location within the cardiac cycle, extra sounds are classified into systolic (usually referred to as clicks: early systolic, mid systolic, and late systolic) or diastolic (usually referred to as snaps, knocks, or plops) (see Table 11-2 and Fig. 11-4). For each of them, we shall review acoustic characteristics, pathogenesis, and clinical significance.
64 Which bedside maneuvers can intensify S3 and S4?
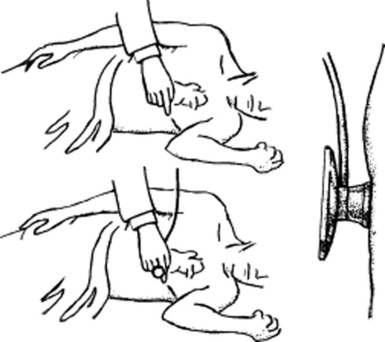
Maneuvers that increase venous return, intracardiac blood volume, and flow across the atrioventricular valves (Fig. 11-5). These include (1) leg raising, (2) mild exercise (such as assuming the left lateral decubitus—or even coughing a few times may unmask a gallop), (3) abdominal compression, (4) the release phase of Valsalva, and (5) respiration. Held-exhalation tends to intensify the left-sided S3 and S4 (with S4 increasing in early exhalation and S3 in end-exhalation), whereas held-inspiration tends to intensify the right-sided S3 and S4. Conversely, maneuvers that decrease venous return, intracardiac blood volume, and transvalvular flow (such as sitting, standing, and the strain phase of Valsalva) will soften a pathologic S3 or S4 and totally eliminate a physiologic S3. Note that all these maneuvers increase (or decrease) the intensity of both S4 and S3, but they will do so much more dramatically with S3.
70 How is S3 after an extra systole?
Louder. The mechanism is the same: increased ventricular filling following the premature beat.
74 Which is easier to detect: S3 or S4?
S4. It is higher pitched and louder, even though not quite as long (the S3 is often prolonged by a series of low-pitched and humming vibrations, rumble-like—see question 90).
77 Is S3 always a gallop?
No. A gallop is any triple lilt whose cadence resembles the canter of a horse. Accordingly, a ventricular gallop (i.e., a gallop produced by S3) is only one of three forms of gallop (see also S4 and summation gallop). The sine qua non for a gallop is its lilt, which usually requires S1 and S2 to be almost as soft as the pathologic extra sound. It also requires a relatively fast heart rate, even though gallops can at times be rather slow, as long as they maintain the necessary cadence. Still, tachycardia remains the prerequisite for the summation gallop (see questions 81–84).
91 What are the hemodynamic implications of an S3?
They depend on the mechanism responsible for its generation.
 In patients with increased left ventricular preload (diastolic overload), the atrial pressure is not necessarily elevated, while cardiac index and ejection fraction may even be increased.
In patients with increased left ventricular preload (diastolic overload), the atrial pressure is not necessarily elevated, while cardiac index and ejection fraction may even be increased.
 In patients with systolic dysfunction (and abnormal ventricular compliance), the cardiac index and ejection fraction are instead both decreased, whereas left atrial, pulmonary diastolic, pulmonary capillary wedge, and left ventricular pressures are all increased. Hence, the left ventricle is dilated and the end-diastolic volume increased. S3 in ventricular dysfunction reflects ejection fraction <30% and filling pressure >25 mmHg. That the sound is partly due to an increased atrial pressure is demonstrated by its disappearance after diuresis.
In patients with systolic dysfunction (and abnormal ventricular compliance), the cardiac index and ejection fraction are instead both decreased, whereas left atrial, pulmonary diastolic, pulmonary capillary wedge, and left ventricular pressures are all increased. Hence, the left ventricle is dilated and the end-diastolic volume increased. S3 in ventricular dysfunction reflects ejection fraction <30% and filling pressure >25 mmHg. That the sound is partly due to an increased atrial pressure is demonstrated by its disappearance after diuresis.
94 Which conditions are responsible for an S3 of diastolic overload?
 Intracardiac or intravascular shunts, such as a ventricular septal defect (VSD) or a patent ductus arteriosus (PDA). Note that an atrial septal defect is not responsible for diastolic overload of the left ventricle because the right-to-left atrial shunt actually decreases the transmitral flow (while the increased tricuspid flow is much less likely to cause a right-sided S3).
Intracardiac or intravascular shunts, such as a ventricular septal defect (VSD) or a patent ductus arteriosus (PDA). Note that an atrial septal defect is not responsible for diastolic overload of the left ventricle because the right-to-left atrial shunt actually decreases the transmitral flow (while the increased tricuspid flow is much less likely to cause a right-sided S3).
 Mitral regurgitation (MR) with increased diastolic flow across the mitral valve. Here, S3 is louder and higher pitched than the more typical S3, almost resembling an opening snap. S3 in MR does not necessarily indicate heart failure, but it does indicate a severe regurgitation.
Mitral regurgitation (MR) with increased diastolic flow across the mitral valve. Here, S3 is louder and higher pitched than the more typical S3, almost resembling an opening snap. S3 in MR does not necessarily indicate heart failure, but it does indicate a severe regurgitation.
102 How can you differentiate right from left ventricular S3?
Mostly through the different location (the right-sided S3 is best heard over the left lower sternal border/epigastric area, and not at the apex). Response to respiration also will be different (Fig. 11-6): the right-sided S3 gets louder with inspiration, whereas the left-sided gets louder with exhalation (Carvallo maneuver). Finally, a right-sided S3 is often associated with a parasternal “lift” (see Chapter 10, Cardiovascular Exam, question 129).
103 What is the differential diagnosis of S3?
 A split S2: In contrast to S3, a split S2 is higher pitched (and thus best heard through the diaphragm) and “basilar.” It also has respiratory variations, but does not soften with either a sitting or standing position.
A split S2: In contrast to S3, a split S2 is higher pitched (and thus best heard through the diaphragm) and “basilar.” It also has respiratory variations, but does not soften with either a sitting or standing position.
 Tumor (plop): The hallmark of this sound is its cycle-to-cycle variability, which is not a feature of S3.
Tumor (plop): The hallmark of this sound is its cycle-to-cycle variability, which is not a feature of S3.
 Pericardial knock and opening snap: In contrast to S3, both the knock and the snap (OS) are medium- to high-frequency sounds—thus best detected through the diaphragm.
Pericardial knock and opening snap: In contrast to S3, both the knock and the snap (OS) are medium- to high-frequency sounds—thus best detected through the diaphragm.
112 Why is S4 late diastolic?
Because it is generated immediately before ventricular systole. Hence, it is presystolic.
116 Which disease processes can cause an S4?
 Hypertension, either systemic or pulmonary (note that S4 may precede the electrocardiographic signs of ventricular hypertrophy)
Hypertension, either systemic or pulmonary (note that S4 may precede the electrocardiographic signs of ventricular hypertrophy)
 Aortic stenosis (where S4 is usually associated with a gradient >70 mmHg)
Aortic stenosis (where S4 is usually associated with a gradient >70 mmHg)
 Hypertrophic cardiomyopathy (an audible, and palpable, S4 is almost a sine qua non for this condition)
Hypertrophic cardiomyopathy (an audible, and palpable, S4 is almost a sine qua non for this condition)
 Coronary artery disease (S4 can be heard in as many as 90% of patients with myocardial infarction)
Coronary artery disease (S4 can be heard in as many as 90% of patients with myocardial infarction)
119 Can S4 occur in mitral regurgitation?
Only if acute. Otherwise, mitral regurgitation is typically associated with an S3.
121 Can patients with atrial fibrillation have an S4?
No, since they cannot muster an adequate atrial contraction. The same applies to atrial flutter.
122 What is the differential diagnosis of an S4?
 A split S1: In contrast to S4, a split S1 (1) widens (or shortens) with respiration in one third of patients, (2) does not soften upon standing or sitting, (3) is best heard with the diaphragm, and (4) presents all the way up to the upper left sternal border (the S4, instead, is mostly localized over the apex or lower sternal border).
A split S1: In contrast to S4, a split S1 (1) widens (or shortens) with respiration in one third of patients, (2) does not soften upon standing or sitting, (3) is best heard with the diaphragm, and (4) presents all the way up to the upper left sternal border (the S4, instead, is mostly localized over the apex or lower sternal border).
 S1-ejection click (sound) complex: This may easily simulate an S4–S1 complex and thus be difficult to separate. In contrast to S4, both S1 and ES are medium to high pitched and thus best heard with the diaphragm. They also do not soften when the patient assumes an upright position (as does the S4). Finally, ES is usually audible all the way up to the base, intensifying with exhalation when pulmonic in origin. Note that although S4 can be palpable (as a presystolic impulse), a split S1 and the ES can only be audible.
S1-ejection click (sound) complex: This may easily simulate an S4–S1 complex and thus be difficult to separate. In contrast to S4, both S1 and ES are medium to high pitched and thus best heard with the diaphragm. They also do not soften when the patient assumes an upright position (as does the S4). Finally, ES is usually audible all the way up to the base, intensifying with exhalation when pulmonic in origin. Note that although S4 can be palpable (as a presystolic impulse), a split S1 and the ES can only be audible.
Opening Snap
123 What is an opening snap?
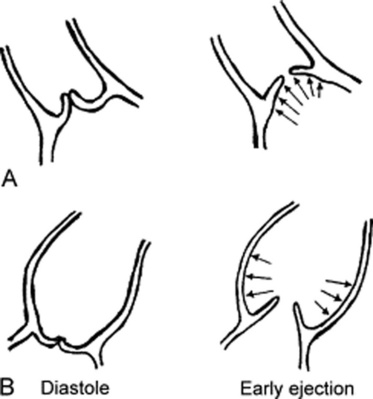
It is a pathologic, loud, snapping, short, high-pitched, and early diastolic extra sound of patients with mitral (or tricuspid) stenosis. It is loudest over the lower left sternal border (a little less at the apex), and is best heard by either using the diaphragm or by applying firm pressure on the bell (thus converting it into a diaphragm). It is produced by the tensing and deceleration of a stenotic but still mobile A-V valve (Fig. 11-7). In this, it resembles the snapping of a sail that is filling with wind. Note that in mitral stenosis, much of the snapping is produced by the filling of the anterior leaflet, which is larger and more mobile than the posterior.
127 Does the timing of OS (i.e., the length of A2–OS) reflect the severity of stenosis?
Yes: the earlier the snap, the worse the stenosis. OS timing is controlled by:
 The pressure in the left atrium at the time of mitral opening (the greater the pressure, the earlier the snap)
The pressure in the left atrium at the time of mitral opening (the greater the pressure, the earlier the snap)
 The heart rate (bradycardia delays the snap, whereas tachycardia anticipates it)
The heart rate (bradycardia delays the snap, whereas tachycardia anticipates it)
 The stiffness of the mitral valve (the stiffer the valve, the longer the A2–OS and thus the later the snap)
The stiffness of the mitral valve (the stiffer the valve, the longer the A2–OS and thus the later the snap)
 Myocardial contractility (ventricular dysfunction lengthens the A2–OS and delays the snap)
Myocardial contractility (ventricular dysfunction lengthens the A2–OS and delays the snap)
 The closing pressure for the aortic valve (the higher the aortic pressure, the later the snap)
The closing pressure for the aortic valve (the higher the aortic pressure, the later the snap)
131 What is a tricuspid opening snap?
It is the opening sound of a stenotic tricuspid valve. This may occur in 5% of MS patients.
136 What other physical findings may accompany constrictive pericarditis?
 Findings of right-sided heart failure: Hepatomegaly (90–100%), ascites (50–90%), leg edema (60%), and often anasarca. The key feature, however, is distention of neck veins (present in 98% of cases), with typically deep X and Y descents that mimic on tracing an “M” or “W.” The deep “Y” (Friedreich’s sign present in 60–90% of cases) is due to the fact that ventricular filling is only impaired at the very end of diastole.
Findings of right-sided heart failure: Hepatomegaly (90–100%), ascites (50–90%), leg edema (60%), and often anasarca. The key feature, however, is distention of neck veins (present in 98% of cases), with typically deep X and Y descents that mimic on tracing an “M” or “W.” The deep “Y” (Friedreich’s sign present in 60–90% of cases) is due to the fact that ventricular filling is only impaired at the very end of diastole.
 Kussmaul’s sign: Inspiratory distention (and not collapse) of the neck veins. This is present in one half of patients with constriction.
Kussmaul’s sign: Inspiratory distention (and not collapse) of the neck veins. This is present in one half of patients with constriction.
 Pulsus paradoxus: This can be present in up to 40% of the cases, but only in the low range of 10–20 mmHg (see Chapter 2, question 92).
Pulsus paradoxus: This can be present in up to 40% of the cases, but only in the low range of 10–20 mmHg (see Chapter 2, question 92).
 Systolic retraction of the apical impulse (see Chapter 10, questions 134 and 135): This occurs in 90% of cases.
Systolic retraction of the apical impulse (see Chapter 10, questions 134 and 135): This occurs in 90% of cases.
(2) Systolic Extra Sounds
140 What is the mechanism of production?
Ejection sounds are produced by blood flowing across the semilunar valves and into the large vessels (Fig. 11-8). Thus, they are normal, but usually inaudible, components of S1. Only in disease, however, they become loud enough to be identifiable as separate acoustic events. In patients with no cardiovascular pathology, ejection sounds are usually the result of a hyperkinetic heart syndrome. In patients with cardiovascular pathology, they reflect instead one of two processes:
 The opening (or doming) of a congenitally bicuspid semilunar valve with/or without stenosis
The opening (or doming) of a congenitally bicuspid semilunar valve with/or without stenosis
 A dilatation of the aortic (or pulmonic) root. The enlarged trunk creates the sound through its sudden tensing in early systole. This is invariably associated with arterial stiffening or high pressure in the corresponding vascular bed (i.e., pulmonary or systemic hypertension).
A dilatation of the aortic (or pulmonic) root. The enlarged trunk creates the sound through its sudden tensing in early systole. This is invariably associated with arterial stiffening or high pressure in the corresponding vascular bed (i.e., pulmonary or systemic hypertension).
141 How do you distinguish an aortic from a pulmonic ejection sound?
 By their different location (left upper parasternal border for the pulmonic, apex for the aortic—even though the latter also can be heard over the aortic area).
By their different location (left upper parasternal border for the pulmonic, apex for the aortic—even though the latter also can be heard over the aortic area).
 By their different response to respiration: The aortic ES has constant intensity throughout respiration, whereas the pulmonic gets louder in exhalation and softer in inspiration because the ballooning of the pulmonic valve (which causes the sound) tends to be less in inspiration, due to the increase in venous return that, in turn, causes a stronger right atrial contraction. The inspiratory softening (and even disappearing) of the pulmonary ES is very much in contrast to the respiratory behavior of all other right-sided findings, whose intensity increases during inspiration, while decreasing during exhalation (Rivero-Carvallo maneuver).
By their different response to respiration: The aortic ES has constant intensity throughout respiration, whereas the pulmonic gets louder in exhalation and softer in inspiration because the ballooning of the pulmonic valve (which causes the sound) tends to be less in inspiration, due to the increase in venous return that, in turn, causes a stronger right atrial contraction. The inspiratory softening (and even disappearing) of the pulmonary ES is very much in contrast to the respiratory behavior of all other right-sided findings, whose intensity increases during inspiration, while decreasing during exhalation (Rivero-Carvallo maneuver).
143 And so, what causes an aortic ES?
 Forceful ejection of blood into a normal aortic root (as it may occur in high output states, like AR) or normal ejection of blood into a stiffened and dilated aortic root (as may occur in patients with hypertension, atherosclerosis, aortic aneurysm, or aortic regurgitation)
Forceful ejection of blood into a normal aortic root (as it may occur in high output states, like AR) or normal ejection of blood into a stiffened and dilated aortic root (as may occur in patients with hypertension, atherosclerosis, aortic aneurysm, or aortic regurgitation)
 Normal ejection of blood through an abnormal aortic valve. This is either a native trileaflet valve that has been stiffened and fused by a rheumatic process or (more commonly) a congenital bicuspid valve.
Normal ejection of blood through an abnormal aortic valve. This is either a native trileaflet valve that has been stiffened and fused by a rheumatic process or (more commonly) a congenital bicuspid valve.
150 What causes a nonvalvular pulmonic ejection sound?
Two possible mechanisms, both taking place in the pulmonary artery:
 Pulmonary hypertension: The ES is caused by ejection of blood into a stiffened pulmonary trunk. The timing of the sound correlates with pulmonary artery diastolic pressure—the higher the pressure, the later the systolic occurrence of ES.
Pulmonary hypertension: The ES is caused by ejection of blood into a stiffened pulmonary trunk. The timing of the sound correlates with pulmonary artery diastolic pressure—the higher the pressure, the later the systolic occurrence of ES.
 Dilation of the pulmonary artery: Contrary to the valvular pulmonic ejection sound, these two arterial ES remain constant throughout respiration.
Dilation of the pulmonary artery: Contrary to the valvular pulmonic ejection sound, these two arterial ES remain constant throughout respiration.
156 Why do clicks of mitral valve prolapse not occur in early systole?
Because they have different modes of generation:
 Early systolic clicks are ejection sounds due to blood flowing across the semilunar valves and into the arterial root (aortic or pulmonic). Hence, they occur at the beginning of ventricular ejection (i.e., early systole).
Early systolic clicks are ejection sounds due to blood flowing across the semilunar valves and into the arterial root (aortic or pulmonic). Hence, they occur at the beginning of ventricular ejection (i.e., early systole).
 Mid- to late-systolic clicks, on the other hand, are regurgitant sounds caused by the posterior billowing of a mitral leaflet. Since this requires a significant decrease in left ventricular size, mid-systolic clicks usually take place during mid to late systole.
Mid- to late-systolic clicks, on the other hand, are regurgitant sounds caused by the posterior billowing of a mitral leaflet. Since this requires a significant decrease in left ventricular size, mid-systolic clicks usually take place during mid to late systole.
160 Which bedside maneuvers can change the timing of an MVP click/murmur?
Maneuvers that modify left ventricular diameter (Fig. 11-9). For a more detailed discussion, please refer to Chapter 12, questions 22, 24, 178, and 179.
E. Pericardial Friction Rub
169 What bedside maneuvers can intensify a pericardial friction rub?
The most common is inspiration: in approximately one third of the patients, rubs become louder in deep and held inspiration because the inspiratory descent of the diaphragm stretches the pericardium, thus making the rubbing of the two layers more likely to occur and more intense. Note, however, that rubs also may be enhanced by held exhalation. This brings the heart closer to the chest wall but also increases venous return to the left ventricle, thus better stretching the pericardial layers onto each other. Finally, having the patient sit up, lean forward, and rest on elbows and knees also may increase contact between the visceral and parietal pericardium and thus their rubbing (Fig. 11-10).
171 Which disease processes are associated with rubs?
 Pericarditis, usually acute or subacute. This can be localized (as in case of trauma or myocardial ischemia) or diffuse (viral or bacterial infections, radiation changes, uremia, and collagen vascular diseases like rheumatoid arthritis and systemic lupus erythematosus). Prevalence of rubs varies from condition to condition. In uremic pericarditis, for example, they can be heard in 14–83% of patients. Still, a rub is only one of the three diagnostic features of acute pericarditis (the others being chest pain and ECG changes).
Pericarditis, usually acute or subacute. This can be localized (as in case of trauma or myocardial ischemia) or diffuse (viral or bacterial infections, radiation changes, uremia, and collagen vascular diseases like rheumatoid arthritis and systemic lupus erythematosus). Prevalence of rubs varies from condition to condition. In uremic pericarditis, for example, they can be heard in 14–83% of patients. Still, a rub is only one of the three diagnostic features of acute pericarditis (the others being chest pain and ECG changes).
 Acute myocardial infarction. Rubs occur in 20% of cases, usually a few days into the course (they are typically absent in the first 24 hours). Rubs carry a worse prognosis, reflecting larger infarcts, more extensive coronary disease, lower ejection fractions, and a greater number of complications—including arrhythmias and pump failure (but not tamponade). Although fleeting in simple post infarction pericarditis, rubs can last much longer in post–myocardial infarction (Dressler’s) syndrome.
Acute myocardial infarction. Rubs occur in 20% of cases, usually a few days into the course (they are typically absent in the first 24 hours). Rubs carry a worse prognosis, reflecting larger infarcts, more extensive coronary disease, lower ejection fractions, and a greater number of complications—including arrhythmias and pump failure (but not tamponade). Although fleeting in simple post infarction pericarditis, rubs can last much longer in post–myocardial infarction (Dressler’s) syndrome.
 A pericardial rub also can occur (albeit rarely) in patients with pulmonary embolism.
A pericardial rub also can occur (albeit rarely) in patients with pulmonary embolism.
 Finally, a localized rub is often heard in patients with metastatic involvement of the pericardium, even though only 7% of all neoplastic effusions are associated with a rub. Curiously, in patients with known cancer who develop a rub, the finding argues against a neoplastic etiology, predicting instead either an idiopathic or a radiation-induced process.
Finally, a localized rub is often heard in patients with metastatic involvement of the pericardium, even though only 7% of all neoplastic effusions are associated with a rub. Curiously, in patients with known cancer who develop a rub, the finding argues against a neoplastic etiology, predicting instead either an idiopathic or a radiation-induced process.
172 Does the presence of a rub exclude a pericardial effusion?
No. One tenth of all rubs will be associated with a pericardial effusion. In fact, rubs can occur in up to one fourth of tamponade cases. Although this is counterintuitive, it reflects a loculated process, capable of compromising ventricular filling (the sine qua non of tamponade) while simultaneously allowing parts of the pericardium to rub against each other. Hence, never exclude tamponade because of a rub. Instead, measure pulsus paradoxus—especially in patients with tachycardia, tachypnea, distended neck veins, and clear lungs (see Chapter 2, questions 93–97).
173 What is the differential diagnosis of a pericardial friction rub?
A three-component rub must be differentiated from the to-and-fro murmur of aortic regurgitation and the continuous murmur of patent ductus arteriosus, and the systo-diastolic murmur of severe mitral regurgitation (see “lots of noise,” Chapter 12, question 263). The scratching and creaking qualities of the rub will usually help recognize it. A three-component rub also may resemble a ventricular gallop (because its early diastolic component coincides with the S3 timing), especially in tachycardic patients, who, after all, represent the majority of pericarditis cases. To identify the rub, rely on its loudness, high frequency, and typical scratchy quality. A one-component (systolic) rub may pose the greatest diagnostic challenge, since it is often misdiagnosed as a systolic ejection murmur. To sort it out, monitor the sound over time: a rub will usually change in quality and intensity, often acquiring one or two diastolic components.
1 Benchimol A, Desser KB. The fourth heart sound in patients without demonstrable heart disease. Chest. 1977;93:298-301.
2 Breen WJ, Rekate AG. Effect of posture on splitting of the second heart sound. JAMA. 1960;173:1326-1328.
3 Constant J. Bedside Cardiology. Boston: Little, Brown & Co; 1985.
4 Evans W, Jackson F. Constrictive pericarditis. Br Heart J. 1952;14:53-69.
5 Folland ED, Kriegel BJ, Henderson WG, et al. Implications of third heart sounds in patients with valvular heart disease. N Engl J Med. 1992;327:458-462.
6 Fontana ME, Wooley CF, Leighton RF, et al. Postural changes in left ventricular and mitral valvular dynamics in systolic click—Late systolic murmur syndrome. Circulation. 1975;51:165-173.
7 Fowler NO, Adolph RJ, et al. Fourth sound gallop or split first sound. Am J Cardiol. 1972;30:441-444.
8 Hancock EW. The ejection sound in aortic stenosis. Am J Med. 1966;40:569-577.
9 Ishikawa M, Sakata K, Maki A, et al. Prognostic significance of a clearly audible fourth heart sound detected a month after an acute myocardial infarction. Am J Cardiol. 1997;80:619-621.
10 Ishmail AA, Wing S, Ferguson J, et al. Interobserver agreement by auscultation in the presence of a third heart sound in patients with congestive heart failure. Chest. 1987;91:870-873.
11 Leatham A. The second heart sound: Key to heart auscultation. Acta Cardiol. 1964;19:395.
12 Leech G, Brooks N, Green-Wilkinson A, et al. Mechanism of influence of PR interval on loudness of first heart sound. Br Heart J. 1980;43:138-142.
13 Marcus GM, Michaels AD, De Marco T, et al. Usefulness of the third heart sound in predicting an elevated level of B-type natriuretic peptide. Am J Cardiol. 2004;93:1312-1313.
14 McGee S. Evidence-based Physical Diagnosis. Philadelphia: Saunders, 2001.
15 Nelson WP, North RL, et al. Splitting of the second heart sound in adults forty years and older. Am J Med Sci. 1967;254:805. 80
16 Patel R, Bushnell DJ, Sobotka PA. Implications of an audible third heart sound in evaluating cardiac function. West J Med. 1993;158:606-609.
17 Perloff JK, Harvey WP. Mechanisms of fixed splitting of the second heart sound. Circulation. 1958;18:998-1009.
18 Pitt A, Pitt B, Schaefer J, et al. Myxoma of the left atrium: Hemodynamic and phonocardiographic consequences of sudden tumor movement. Circulation. 1967;36:408-416.
19 Posner MR, Cohen GI, Skarin AT, et al. Pericardial disease in patients with cancer: The differentiation of malignant from idiopathic and radiation-induced pericarditis. Am J Med. 1981;71:407-413.
20 Ronan JA. Cardiac auscultation: Opening snaps, systolic clicks, and ejection sounds. Heart Dis Stroke. 1993;2:188-191.
21 Ronan JA. Cardiac auscultation: The first and second heart sounds. Heart Dis Stroke. 1992;1:113-116.
22 Ronan JA. Cardiac auscultation: The third and fourth heart sounds. Heart Dis Stroke. 1992;1:267-270.
23 Shaver JA, O’Toole JD. The second heart sound: Newer concepts. Part 2: Paradoxical splitting and narrow physiological splitting. Mod Concept Cardiovasc Dis. 1977;46:13-16.
24 Spodick DH. Pericardial rub: Prospective, multiple-observer investigation of pericardial friction in 100 patients. Am J Cardiol. 1975;35:357-362.
25 Sutton G, Harris A, Leatham A. Second heart sound in pulmonary hypertension. Br Heart J. 1968;30:743-756.
26 Van de Werf F, Geboers J, Kesteloot H, et al. The mechanisms of disappearance of the physiologic third heart sound with age. Circulation. 1986;73:877-884.