Chapter 27 Heart Failure and Valvular Heart Disease
1 What are the causes of cardiomyopathy resulting in the syndrome of heart failure (HF)?
 Reduced ejection fraction (HFREF, systolic HF, dilated cardiomyopathy): impaired contraction and/or loss of cardiomyocytes. Multiple causes but approximately 65% ischemic.
Reduced ejection fraction (HFREF, systolic HF, dilated cardiomyopathy): impaired contraction and/or loss of cardiomyocytes. Multiple causes but approximately 65% ischemic.
 Normal or preserved ejection fraction (HFNEF, diastolic HF): abnormal relaxation and/or increased stiffness of the left ventricle (LV), most commonly associated with hypertension, type 2 diabetes mellitus, and aging. Comorbidities (e.g., chronic obstructive pulmonary disease, stroke, obstructive sleep apnea) are very common.
Normal or preserved ejection fraction (HFNEF, diastolic HF): abnormal relaxation and/or increased stiffness of the left ventricle (LV), most commonly associated with hypertension, type 2 diabetes mellitus, and aging. Comorbidities (e.g., chronic obstructive pulmonary disease, stroke, obstructive sleep apnea) are very common.
 Restrictive cardiomyopathy: markedly decreased LV compliance leading to impaired diastolic filling. The usual cause is infiltrative disease.
Restrictive cardiomyopathy: markedly decreased LV compliance leading to impaired diastolic filling. The usual cause is infiltrative disease.
 Hypertrophic cardiomyopathy: LV hypertrophy usually with asymmetric septal thickening and often outflow tract systolic pressure gradient. The mechanisms of HF are complex, but the presumed cause is sarcomeric protein mutations.
Hypertrophic cardiomyopathy: LV hypertrophy usually with asymmetric septal thickening and often outflow tract systolic pressure gradient. The mechanisms of HF are complex, but the presumed cause is sarcomeric protein mutations.
 Right ventricular (RV) failure: Most common causes are LV failure, obstructive sleep apnea, pulmonary hypertension, and RV myocardial infarction (MI).
Right ventricular (RV) failure: Most common causes are LV failure, obstructive sleep apnea, pulmonary hypertension, and RV myocardial infarction (MI).
2 What are the causes of HFREF besides ischemic heart disease or MI?
| Type | Cause |
|---|---|
| Myocarditis | Infectious (viral) or inflammatory (e.g., systemic lupus erythematosus) giant cell (may require transplant) |
| Toxins | EtOH, cocaine, cancer chemotherapy, radiation |
| Stress-induced cardiomyopathy | Catecholamine surge from stress, apical ballooning (takotsubo syndrome) |
| Genetic | Idiopathic, familial (multiple mutations) |
| Valvular disease | Aortic, mitral (see valvular disease section) |
| Other | Peripartum, sustained tachycardia, HTN, DM, endocrine or nutritional, acidosis, sepsis |
DM, Diabetes mellitus; EtOH, ethyl alcohol; HTN, hypertension.
3 How do we classify HF by functional status or stage?
Table 27-2 Classifying Heart Failure by Functional Status/Stage
| NYHA Functional Classification | |
| Class I (mild) | No limitation of physical activity |
| Class II (mild) | Slight limitation of physical activity |
| Class III (moderate) | Marked limitation of physical activity |
| Class IV (severe) | Unable to carry out any physical activity without discomfort, symptoms at rest |
| ACC-AHA Staging System | |
| Stage A | Patients at high risk for development of HF in the future but no functional or structural heart disease |
| Stage B | Structural heart disease but no symptoms |
| Stage C | Previous or current symptoms of HF in the context of underlying structural heart disease, adequately managed with medical treatment |
| Stage D | Advanced disease requiring hospital-based support, heart transplantation or mechanical support, or palliative care |
ACC, American College of Cardiology; AHA, American Heart Association; NYHA, New York Heart Association.
5 How is acute decompensated HF treated?
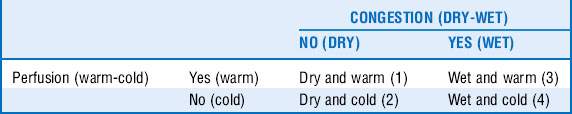
Treatment is based on systemic perfusion and evidence of vascular congestion. See Table 27-3.
Congestion: dyspnea, orthopnea, crackles, elevated venous pressure, ascites, peripheral edema
Impaired perfusion: reduced pulse pressure, cold extremities, altered mentation
The numbers in Table 27-3 can be defined as follows:
1. Normal and requires no intervention.
2. Pump failure without pulmonary edema. Usually represents end-stage HF. Patients require inotropic support: dobutamine (β1-adrenergic agonist), milrinone (phosphodiesterase inhibitor), mechanical support (intraaortic balloon pump [IABP], LV assist device); consider cardiac transplantation.
3. Adequate perfusion with volume overload and increased filling pressures. The treatment focus is intravenous loop diuretics (most commonly furosemide) or bedside ultrafiltration. Reduction of preload with intravenous vasodilators (morphine sulfate, nitroglycerin or nitroprusside, angiotensin-converting enzyme inhibitors [ACEIs]) is another option.
4. Volume overload with pump failure. These patients require inotropes, vasodilators, diuretics, and consideration of mechanical support.
 Ultrafiltration can remove large amounts of volume rapidly and is usually reserved for patients in whom an adequate response to IV diuretics is not achieved.
Ultrafiltration can remove large amounts of volume rapidly and is usually reserved for patients in whom an adequate response to IV diuretics is not achieved.
 Nesiritide is an alternative vasodilator therapy in patients whose blood pressure is normal and who continue to have dyspnea because of volume overload despite the use of intravenous loop diuretics.
Nesiritide is an alternative vasodilator therapy in patients whose blood pressure is normal and who continue to have dyspnea because of volume overload despite the use of intravenous loop diuretics.
Aortic stenosis
9 What is the classic triad of symptoms of AS, and what is its significance?
10 How is the severity of AS graded with use of echocardiographic-Doppler methods?
Table 27-4 Grading Aortic Stenosis with Use of Echocardiographic-Doppler Methods
| Severity | Mean gradient (mm Hg) | Valve area (cm2) |
|---|---|---|
| Mild | < 25 | > 1.5 |
| Moderate | 25-40 | 1.0-1.5 |
| Severe | > 40 | < 1.0 |
Mitral stenosis
15 How is mitral stenosis graded with use of echocardiographic-Doppler methods?
Table 27-5 Grading Mitral Stenosis with Use of Echocardiographic Doppler Methods
| Severity | Mean gradient (mm Hg) | Mitral valve area (cm2) |
|---|---|---|
| Mild | < 5 | > 1.5 |
| Moderate | 5-10 | 1.0-1.5 |
| Severe | > 10 | < 1.0 |
Aortic regurgitation
18 What are the causes of aortic regurgitation (AR)?
| Valvular disease | Aortic disease |
|---|---|
| Rheumatic | — |
| Bicuspid | Type A aortic dissection |
| Endocarditis (bacterial or marantic) | Marfan |
| Degenerative or calcified | Degenerative |
| Vasculitis | Inflammatory (syphilis, Reiter syndrome) |
Mitral regurgitation
25 What are the indications for surgery in MR?
Note: EF < 25% is usually prohibitive for surgery because of high operative mortality.
1 Bonow RO, Carabello BA, Chatterjee K, et al: 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons.J Am Coll Cardiol 52:e1-e142, 2008.
2 Carabello B.A. The current therapy for mitral regurgitation. J Am Coll Cardiol. 2008;52:319–326.
3 Carabello B.A. Contemporary aortic valve therapy. Methodist DeBakey Cardiovasc J. 2010;6:33–39.
4 Felker G.M., Thompson R.E., Hare J.M., et al. Underlying causes and long-term survival in patients with initially undiagnosed cardiomyopathy. N Engl J Med. 2000;342:1077.
5 Hunt SA, Abraham WT, Chin MH, et al: 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation 119:e391, 2009.
6 Nohria A., Mielniczuk L.M., Stevenson L.W. Evaluation and monitoring of patients with acute heart failure syndromes. Am J Cardiol. 2005;96:32G–40G.